Diets for diabetes
A systematic review and assessment of effects, health economic and ethical aspects
Introduction
The current publication is the English summary and conclusions of a health technology assessment in Swedish, comparing health outcomes of different diets and dietary treatments, as well as certain foods, nutrients, and beverages in individuals with type 1, type 2, and gestational diabetes [1]. The follow-up time was at least 6 months for individuals with type 1 and type 2 diabetes, and 6 weeks for gestational diabetes.
The correlations between what participants reported to ingest and the different health outcomes are based on prospective cohort studies, and the effects of interventions such as dietary advice are based on randomized controlled studies (RCT). In the conclusions referring to correlations, the causality between diet and health outcome could not be confirmed due to the study design, thus a causal relationship might exist, although it is also possible that confounding factors may have affected the result.
Conclusions
Type 1 and type 2 diabetes
- There is a correlation between Mediterranean diet and a lower risk of all-cause mortality (moderate certainty of evidence).
- There is a correlation between eating greater proportions of (footnote 1) fiber or legumes and a lower risk of all-cause mortality (moderate certainty of evidence). There may also be a link between greater proportions of nuts and a lower risk of all-cause mortality (low certainty of evidence) and a lower risk of cardiovascular disease (low certainty of evidence).
- There is a correlation between drinking more coffee and a lower risk of all-cause mortality and from coronary heart disease (moderate certainty of evidence) and possibly also a lower risk of mortality from cardiovascular disease (low certainty of evidence).
- There is an overall lack of long-term studies comparing the impact of different types of dietary advice on survival, diabetes complications, diabetes remission (footnote 2), quality of life, and side effects. In addition, the reliability of existing results is very low for most diets included in this review, as well as for dietary treatments, foods, and nutrients that have been evaluated. In these cases, effects on health and related measures cannot be assessed.
Footnote 1. The terms "greater proportion" or "more" do not necessarily refer to eating or drinking more in total, but rather to an increase in the amount by replacing it with other foods or beverages.
Footnote 2. Only applies to type 2 diabetes.
Type 2 diabetes
- There may be a correlation between eating a greater proportion of saturated fat and a higher risk of mortality from cardiovascular disease (low certainty of evidence). There may also be a correlation between eating a greater proportion of monounsaturated fat and a lower risk of mortality regardless of cause (low certainty of evidence).
- A treatment with an initial period of greatly reduced energy intake using very low-energy diet (VLED) with subsequent transition to food for weight stability compared to regular dietary treatment has beneficial effects on quality of life (assessed with EQ-5D), long-term blood sugar level (HbA1c) and weight up to 12 months (moderate certainty of evidence)3. Furthermore, methods including VLED may have beneficial effects on diabetes remission4 and waist circumference up to 12 months (low certainty of evidence) and long-term blood sugar levels (HbA1c) up to 24 months (low certainty of evidence).
- Intensive lifestyle treatment, combining low-fat diet with physical activity and reduced energy intake, has beneficial effects compared to regular dietary treatments on long-term blood sugar (HbA1c), weight, body mass index (BMI), waist circumference, and certain blood fats up to 12 months (moderate certainty of evidence)3. The weight loss can persist up to about 10 years (low certainty of evidence). The treatment can lead to better physical quality of life up to 8 years (low certainty of evidence), while the effect difference in mental quality of life over the same period can be non-existent or negligible (low certainty of evidence). The comparison shows no change in the risk of mortality regardless of cause or the risk of mortality or falling ill from cardiovascular causes after about 10 years (low certainty of evidence). From a health economic perspective, intensive lifestyle treatment is more resource-intensive than regular dietary treatments, and at the individual level calculations show small or no gains in quality-adjusted life years (QALYs).
- Energy restrictions aassociated with intensive lifestyle treatments with a ketogenic diet or with a high-protein diet (20E%) combined with physical activity, compared to regular dietary treatments can result in a weight loss lasting up to 11 months (low certainty of evidence), but we identified no studies investigating if the weight can be maintained for longer time periods. There is a lack of studies investigating clinically important outcomes, such as mortality, cardiovascular diseases, quality of life, and diabetes remission.
3. Based on individuals with a mean body weight of approximately 100 kg and mean HbA1c of 60 mmol/mol.
4. The results for the outcome diabetes remission (defined as an HbA1c of less than 48 mmol/mol and not taking blood sugar lowering drugs) apply when a diabetes diagnosis was made less than 6 or less than 3 years ago.
Gestational diabetes
- The effects and certainty of evidence were not assessed for diets for gestational diabetes due too few studies.
Comments to the above conclusions
Diet adherence is not commonly studied when dietary advice is given, and it is possible that the health effects may depend on adherence over time. As indicated by a greater weight loss at the beginning of studies, adherence to diets can be assumed to be better in the beginning of a study and decrease over time.
SBU has identified several possible risks of inequality in diabetes care. Self-care responsibility for diabetics, and compliance to dietary guidelines, can be challenging for person with mental or intellectual disabilities, low socioeconomic status, or lack of language skills.
Furthermore, the cost of a low-fat diet, high-protein diet, low-carb diet, Mediterranean diet, and ketogenic diet, were more expensive than a normal diet as estimated by the Swedish Consumer Agency. The lactovegetarian diet was an exception and were equally expensive. The Mediterranean and low-carbohydrate diets were estimated to have the highest costs, which can contribute to health inequalities. It is important that healthcare offers equal care for people with diabetes regardless of where they live and what socio-economic status they have.
Offering health-promoting dietary advice while respecting the autonomy and integrity of the individual can pose an ethical dilemma for health professionals. For example, if the health professional wants to do good by giving dietary advice aimed for weight loss, this may however be perceived as violating the integrity and be moralizing by the patient. For health professionals, this means a balance between, available evidenced in dietary advice and person-centeredness with sensitivity and adherence to the individual's own wishes, perceptions, and conditions.
Background
Scientifical evidence show that specific dietary habits for people with diabetes leads to blood sugar levels within the normal range that potentially can reduce the risk for consequential nerve and kidney impairments and eye complications. Moreover, in diabetes, the risk for cardiovascular disease is increased, thus, the dietary habits need to have beneficial effects on established risk factors, such as obesity, elevated blood fats, and hypertension, and preferably also reduce the risk of morbidity and premature death.
Maintaining normal body weight or losing weight in obesity may also reduce the risk of developing type 2 diabetes. In type 2 diabetes, blood sugar levels can be improved by losing weight, especially in those with abdominal obesity. Maintaining normal body weight or losing weight in obesity may also reduce the risk of developing type 2 diabetes.
Aim
The aim of this project was to evaluate the positive and negative health effects of food and dietary treatments in individuals with type 1, type 2, and gestational diabetes, and additionally to analyse health economic and ethical aspects. The report will serve as a scientific basis for the development of new recommendations for dietary treatment in diabetes by the Swedish National Board of Health and Welfare.
Method
A systematic review conducted in accordance with the PRISMA statement. The protocol is registered in Prospero CRD42020173880. The certainty of evidence was assessed with GRADE.
Review questions
- What effect do food choices and dietary treatments have on mortality, morbidity, and quality of life in adults with type 1 and type 2 diabetes and gestational diabetes (GDM)?
- What effect do food choices and dietary treatments have on diabetes remission in adults with type 2 diabetes?
- What effect do food choices and dietary treatments have on glucose control, blood fats, body weight, and other risk factors in adults with type 1 and type 2 diabetes and GDM?
- What is the relationship between costs and effects of food choices and dietary treatments compared to the most relevant comparator?
- What effect does physical activity have in addition to the dietary treatment in the questions above?
Inclusion criteria
Population:
Adults, from 18 years with diabetes, type 1 and 2. Women from 18 years with gestational diabetes.
Intervention:
All types of food (recommended, self-reported and estimated by biomarkers) if any of the following is defined:
- diet composition
- individual foods
- dietary treatment
Meal replacement based on Very Low Energy Diet (VLED)
Beverages (beverages that contain alcohol is excluded)
Intermittent fasting or meal frequency
Carbohydrate counting
Diet in combination with physical activity
Control:
Conventional diabetic diets or other defined or established diets, and self-selected food (not dietary treatment) if defined or described on a group level.
Main outcomes:
- Mortality (total and cause-specific mortality)
- Morbidity (total morbidity, diabetes complications, need for drug treatment, osteoporosis)
- For newly diagnosed type 2 diabetes within 6 years or less: diabetes remission
- Quality of life (e.g. EQ-5D, SF-6D, SF-36, ADDQoL)
- Side effects (e.g. hypo- or hyperglycemia).
For the population with gestational diabetes: Preeclampsia and negative pregnancy outcomes.
Additional outcomes:
- Glucose control (HbA1c), body weight, BMI, waist circumference, blood pressure, and plasma lipids (LDL cholesterol, HDL cholesterol, total cholesterol, triglycerides)
- For the population with gestational diabetes, changes in fasting blood sugar, HbA1c, and 2h sugar after oral glucose tolerance test (OGTT), body weight and the child's birth weight
Study design:
Randomized controlled trials (RCT) and prospective cohort studies
Language:
English, Swedish, Norwegian, and Danish
Search period:
From 2009 to 2021. Final search was conducted in February 2021.
Databases searched:
CINAHL by EBSCO, Cochrane Library, Embase by Elsevier, Ovid MEDLINE
Additional searches:
All included studies from the former SBU report Mat vid Diabetes from 2010 were screened for inclusion [2]. Relevant systematic reviews and included articles were systematically screened for additional relevant studies.
Measures of effect:
Mean difference, odds ratio, risk difference, relative risks, hazard ratio.
Follow up time:
at least 24 weeks (6 months), for gestational diabetes 6 weeks or longer.
Data extraction (selection and coding)
Data was extracted to a separate table (Appendix 4) by two project members. One person extracted the data and the other doublechecked the information from the original article.
The following data was extracted from randomized controlled trials: a) first author, publication year, country, b) study design, population (diabetes type), setting, and duration of the follow-up, c) description of the intervention, participant characteristics at baseline (including number of participants, percentage of women/men, age, body weight, body mass index, HbA1c, and drop-outs at end point, d) description of the control, participant characteristics at baseline, d) results (effects and side effects).
The following data was extracted from prospective cohort studies: a) first author, publication year, country, b) study design, population (diabetes type), name of study (cohort), and duration of the follow-up, c) participant characteristics at baseline (the number of participants, percentage of women/men, age, BMI and insulin use, d) exposure, number per group at baseline, d) dietary assessment method, repeated measurements, and confounders, e) results (effects and side effects), number of events and drop-outs.
Risk of bias assessment
Included studies were assessed for risk of bias, using risk of bias tools developed by Cochrane, (the templates have been translated into Swedish and validated). The risk of bias tools were used according to study type (RCT/RoB-2 for RCT, and ROBINS-I for prospective cohort studies) [3]. The risk of bias tools were adjusted for the current assignment. Risk of bias was assessed by at least two independent reviewers. Discrepancies in risk of bias assessment were resolved to a unanimous decision by using a third reviewer.
Strategy for synthesis
When appropriate, data was synthesized by meta-analysis when at least two studies evaluated the same outcomes with similar follow-up time. The software RevMan (Version 5.3.5) was used. Random effects models, 95 percent confidence intervals, and inverse variance model were used. The principal measure calculated for continuous data were mean difference. Results from studies deemed too heterogeneous was not synthesized.
Appropriate analysis involves matching the intervention and the control diet.
Examples of diets that were matched include:
- intensive lifestyle treatment; low-fat diet (less than 30% energy from fat)
- low-carbohydrate diet (between 10% to 30% energy from carbohydrates)
- ketogenic diet (less than 50 gram or less than 10% energy from carbohydrates)
- high protein diet (more than 20% energy from protein)
- very high protein diet (equal to or more than 30% energy from protein)
- vegetarian diet (no meat, poultry, or fish); vegan diet (without meat, poultry, fish, eggs, or traditional dairy products)
- Mediterranean diet (fruit, vegetables, olive or rapeseed oil, legumes, cereals, fish, 30 to 44% energy from fat)
- DASH (high intake of fruits and vegetables, low-fat dairy, whole-grain cereals, and limited sodium)
- low-GI diet (values on the glycemic index must be reported)
- intermittent fasting (periodic fasting for a few days a week, usually 2 days)
- paleolithic diet (vegetables, fruits, meat, fish, nuts, and green “leafy” vegetables, limited or no intake of charcuterie, dairy products, starchy cereals, foods with solid fats and added sugar, alcohol, salt, and sugary drinks)
- Very Low Energy Diet, VLED (powder portion mixed with cold or hot water, three to five servings per day, depending on the brand, corresponds to an energy intake of about 500 to 800 kcal per day.
For the included prospective cohort studies, it was not possible to combine the results of multiple studies in meta-analyses. The reason was that there was too much heterogeneity in the included studies regarding how they chose to categorize what the individuals themselves chose to eat, the duration of the follow-up time, kind of statistical analysis performed, handling of confounding, and how the results were presented. The synthesis of the results was therefore made based on an analytical reasoning, using the method of Synthesis Without Meta-analysis (SWiM) (see Cochrane).
Assessing the certainty of evidence
The certainty of evidence of the combined results was assessed based on the overall scientific evidence. In this assessment, SBU uses a system based on the Grading of Recommendations Assessment, Development and Evaluation (GRADE) to classify reliability [4]. The assessments have not been based on a strict limit of clinical relevance as even small changes in outcomes over a lifetime can be considered clinically important. There has been a harmonization between all assessments.
| Certainty | What it means |
|---|---|
| Very low | The true effect is probably markedly different from the estimated effect |
| Low | The true effect might be markedly different from the estimated effect |
| Moderate | The authors believe that the true effect is probably close to the estimated effect |
| High | The authors have a lot of confidence that the true effect is similar to the estimated effect |
The evaluation included 81 articles with a low or moderate risk of bias (Figure 2). The tables below present a selection of summary of findings of the primary outcome measures assessed to have moderate or low certainty of evidence (full tables refer to the original publication in Swedish www.sbu.se/345)
| a Two prospective cohort studies (Bonaccio and Hodge), In total 4 145 participants, –1 due to Risk of bias from remaining confounding | |||
| Food | Outcome | Effect | GRADE |
|---|---|---|---|
| Greater consumption of Mediterranean food | All-cause mortality | SwiM due to different exposures and follow-up times. Lower risk | Moderate ⊕⊕⊕◯a |
| Mortality from cardiovascular disease | SwiM due to different exposures and follow-up times. Lower risk | Moderate ⊕⊕⊕◯a | |
| CI = Confidence interval; HbA1c = long term blood sugar; HR = Hazard ratio; MD = Mean difference; mmol/mol = Millimolar per mol; VLED = low energy powder, SF-36 = Short Form Health Survey -36; EQ-5D = EuroQol. a one RCT (Wing 2013), 5 135 participants, –1 Risk of bias (some concerns with blinding) and –1 Imprecision (one study that needs to be independently repeated) b Two RCT (Rock 2014, Williamson 2009), 5 295 participants, –1 Risk of bias (some concerns with blinding) and –1 Imprecision (Independently repeated studies may change the overall result) c one RCT (Rubin 2014), 5 135 participants, –1 Risk of bias (some concerns with blinding) and –1 Imprecision (one study that need to be independently repeated) d Three RCT (Lean 2018, Brown 2020, Taheri 2020), 535 participants, –1 Risk of bias (some concerns with blinding) e Two RCT (Lean 2018, Taheri 2020), 445 participants, –1 Risk of bias (some concerns with blinding) and –1 Imprecision (Independently repeated studies may change the overall result) |
||||
| Dietary treatments and comparison Type of diabetes | Outcome | Follow up | Effect (95 % CI) | GRADE |
|---|---|---|---|---|
| Intensive lifestyle treatment with low fat diet and physical activity compared to regular dietary treatment, type 2 diabetes | Mortality of any cause | Median 9.6 years | HR: 0.85 (0.69 to 1.04) No difference |
Low ⊕⊕◯◯a |
| Mortality from cardiovascular causes | Median 9.6 years | HR: 0.88 (0.61 to 1.29) No difference |
Low ⊕⊕◯◯a |
|
| Mortality from heart attack | Median 9.6 years | HR: 0.44 (0.15 to 1.26) No difference |
Low ⊕⊕◯◯a |
|
| Onset of stroke | Median 9.6 years | HR: 1.05 (0.77 to 1.42) No difference |
Low ⊕⊕◯◯a |
|
| Quality of life SF-36 Physical component |
12 months | MD 2.90 (2.52 to 3.29) points Better with intensive lifestyle treatment, low fat diet and physical activity |
Low ⊕⊕◯◯b |
|
| Quality of life SF-36 Physical component |
8 years | 0.93 (KI 0,54 to 1.32) points Better with intensive lifestyle treatment, low fat diet and physical activity |
Low ⊕⊕◯◯c |
|
| Quality of life SF-36 Mental component |
8 years | –0.20 (–0.65 to 0.25) points No or negligible difference |
Low ⊕⊕◯◯c |
|
| VLED compared to low fat diet, type 2 diabetes | Quality of life EQ-5D |
12 months | MD: 5.16 (2.33 to 7.99) points Better with VLED |
Moderate ⊕⊕⊕◯d |
| Diabetes remission Defined as: HbA1c <48 mmol/mol |
12 months | Odds ratio (95% CI) 10.83 (4.55 to 25.77) Increase with VLED |
Low ⊕⊕◯◯e |
|
| a Two prospective cohort studies (Sluik and Nöthlings), In total 16 833 participants, –1 due to Risk of bias from remaining confounding [5] [6]. b Three prospective cohort studies (He, Burger and Schoenaker), In total 17 264 participants, –1 due to Risk of bias from remaining confounding [7] [8] [9]. c Five prospective cohort studies (Bidel. Zhang (men), Zhang (women), Sluik, Komorita, In total 21 864 participants, –1 due to Risk of bias from remaining confounding [6] [10] [12] [13]. d Two prospective cohort studies (Bidel and Komorita), 4 831 participants, –1 due to Risk of from to remaining confounding, –1 Imprecision (independent studies may change the overall result) [10] [11]. e Two prospective cohort studies (Bidel and Zhang (women), 11 007 participants, –1 due to Risk of bias from remaining confounding [10] [13]. f Two prospective cohort studies (Liu and Sluik), 22 601 participants, –2 due to Risk of bias mainly from remaining confounding [6] [14]. g Two prospective cohort studies (Liu and Li), 22 526 participants, –2 due to Risk of bias mainly from remaining confounding [14] [15]. h Two prospective cohort studies (Campmans-Kuijpers and Jiao), 17 416 participants, –2 due to Risk of bias mainly from remaining confounding [16] [17]. i Four prospective cohort studies (Trichopoulou, Campmans-Kuijpers, Jiao and Sluik), 24 813 participants, –2 due to Risk of bias mainly from remaining confounding [6] [16] [17] [18]. |
|||
| Food or nutrient | Outcome | Effect | GRADE |
|---|---|---|---|
| Greater consumption of legumes | All-cause mortality | SwiM due to different exposures and follow-up times. Lower risk |
Moderate ⊕⊕⊕◯a |
| Greater consumption of fibers | All-cause mortality | SwiM due to different exposures and follow-up times. Lower risk |
Moderate ⊕⊕⊕◯b |
| Greater consumption of coffee | All-cause mortality | SwiM due to different exposures and follow-up times. Lower risk |
Moderate ⊕⊕⊕◯c |
| Mortality from cardiovascular disease | SwiM due to different exposures and follow-up times. Lower risk |
Low ⊕⊕◯◯d |
|
| Mortality from coronary artery disease | SwiM due to different exposures and follow-up times. Lower risk |
Moderate ⊕⊕⊕◯e |
|
| Greater consumption of nuts | All-cause mortality | SwiM due to different exposures and follow-up times. Lower risk |
Low ⊕⊕◯◯f |
| Disease rate of all cardiovascular disease | SwiM due to different exposures and follow-up times. Lower risk |
Low ⊕⊕◯◯g |
|
| Greater consumption of saturated fat | Mortality from cardiovascular disease | SwiM due to different exposures and follow-up times. Higher risk |
Low ⊕⊕◯◯h |
| Greater consumption of monounsaturated fat | All-cause mortality | SwiM due to different exposures and follow-up times. Lower risk |
Low ⊕⊕◯◯i |
Health Economic Assessment
Summary of the results
Health economic aspects of dietary treatments for diabetes were assessed through an overview of published cost-effectiveness analyses in the field, calculations of the cost of following selected diets evaluated in the project, and a model-based analysis of long-term health outcomes associated with one of the dietary treatments.
- The overview of health economic literature identified two studies of cost-effectiveness of the interventions in question. One was a cost-effectiveness analysis of intensive lifestyle treatment with low fat diet and physical activity, which in this report was found to have beneficial effects on several secondary outcomes compared to regular dietary treatment for people with type 2 diabetes with an average body weight of about 100 kg and an average HbA1c of approximately 60 mmol/mol (moderate certainty of evidence). According to the cost-effectiveness analysis, the intensive lifestyle treatment was resource-intensive and led to small or no gains in quality-adjusted life years (QALYs). The analysis was based on data from the Look AHEAD study.
- Calculations of the cost of following a low-fat diet, high-protein diet, low-carbohydrate diet, lactovegetarian diet, Mediterranean diet, and ketogenic diet showed that all diets except the lactovegetarian one had a higher estimated cost than the Swedish Consumer Agency's normal diet. The Mediterranean and low-carb diets were estimated to be the most expensive diets.
- The model-based analysis of intensive lifestyle treatment with low-fat diet and physical activity compared to regular dietary treatment was based on the effects on HbA1c, blood pressure, blood fats, and weight that emerged in the systematic review. The analysis showed that these effects are estimated to produce slightly more life years and quality-adjusted life years (QALYs) at group level and over a lifetime. However, the average slightly higher gains in years of life and QALYs per person were small (about 0.04 life years gained and about 0.05 QALYs gained over a lifetime perspective, according to discounted calculations).
Ethics
The aim of this report is to evaluate long-term effects, risks and health economic aspects of food choices and dietary treatment in individuals with type 1, type 2, and gestational diabetes, as well as to discuss ethical aspects arising from food recommendations. Overall, the results show that intensive lifestyle treatment is likely to have a more beneficial effects than regular dietary treatment for long-term blood sugar levels (HbA1c), weight, BMI, and waist circumference. Also, the results show that following a Mediterranean diet is likely to be related to lower risk of premature overall mortality and death from cardiovascular heart disease. Examples of individual foods that strengthen the picture of the effects of the Mediterranean diet are that the intake of legumes, fiber, nuts, and increased intake of monosaturated fat and reduced intake of saturated fat, may be related to lower premature mortality.
In conclusion, we see the following ethical aspects as important to consider:
- Self-care responsibilities linked to adherence to dietary advice may be challenging to people with diabetes who have mental or intellectual disabilities, weak socio-economics or lack of language skills.
- Intensive, highly supported lifestyle treatment, and the more expensive Mediterranean diet are likely to have more beneficial effects, which have ethical implications linked to the risk of negative discrimination in people less likely to participate in such treatment, or to afford the diet. It is important to consider an equality and justice perspective so that people with diabetes are offered equal treatment.
- Doing good by offering evidence-based general dietary advice while respecting the individual’s autonomy and integrity can pose an ethical dilemma for health workers, both in relation to the patients and to their loved ones (third parties).
Discussion
Overall, the conclusions of previous assessments from SBU (Dietary Treatment in Diabetes in 2010 and Dietary Treatment in Obesity in 2013) are reinforced by the conclusions of this assessment [2] [19]. Following a Mediterranean diet and food with a high proportion of fiber (such as whole grains, vegetables, fruit) and legumes (peas and beans) are associated with a lower risk of disease and/or premature death. There is also a link between greater consumption of coffee and lower risk of all-cause mortality
There also seem to be a link between nuts and unsaturated fats and lower risk of disease and premature death. On the other hand, consumption of more saturated fats seems to be a linked to an increased risk for premature death.
There is lack of reliable scientific evidence for effects of food eaten by women with gestational diabetes about the health of the child and mother. However, the results relating to diets in type 1 and type 2 diabetes are likely to be transferable to gestational diabetes.
Scientific studies of the effects of different diets, are usually done either in randomized clinical trials or in prospective cohort studies. In the randomized clinical trials, it was decided by a randomization process which diet the participants should follow and thus it is possible to conclude that the effect for a particular group depends on the diet they have followed. However, in randomized studies there are some obvious limitations: 1) the group of people with diabetes included in the studies may not constitute a representative sample of all people with diabetes; 2) it is difficult to carry out these studies with long follow up times in order to examine long-term effects such as diabetes complications; 3) the studies are usually too strictly controlled and difficult to transfer to everyday conditions; 4) participants, assessors, and evaluators are often unblinded, which may cause a methodological shortcoming. However, the methodological quality can be increased if assessors and evaluators were blinded; 5) randomized controlled trials have often assessed secondary outcome measures or surrogate measures, which cannot be directly linked to the primary and near-patient outcomes.
The prospective cohort studies map the eating habits of a large group of people with diabetes and then follow them for several years and record possible diabetes complications and deaths. These studies are therefore important when drawing conclusions on the long-term effects that certain eating habits have on diabetes. The main limitation when investigating eating habits is linked to other factors, such as lifestyle in general. Even though the statistical analysis adjusted the results for differences in, for example, smoking and physical activity, it is difficult to say with certainty that the relationship between a particular type of food and a diabetes complication depends on eating habits. As concluded already in the SBU 2010 Dietary Treatment at Diabetes report, many prospective cohort studies have serious methodological shortcomings, when it comes to adjusting for socio-economic factors [2]. It is also difficult to measure eating habits reliably. Methods that are demanding for the participant, such as dietary registration over several days, are associated with low response rates. Most studies have measured eating habits with a questionnaire, a so-called Food Frequency Questionnaire (FFQ), which is a less demanding dietary examination method. If the measurement method has difficulty estimating the actual intake, the possibilities of detecting actual relationships between diet and health outcomes in people with diabetes are reduced. As the participants are followed-up for several years, it is important to repeat the measurement of eating habits during the follow-up period. Many of the studies have only measured eating habits at one time-point, which is a weakness. Finally, one can question how representative the study group is for all people with diabetes in these cohort studies.
Conflicts of Interest
In accordance with SBU’s requirements, the experts and scientific reviewers participating in this project have submitted statements about conflicts of interest. These documents are available at SBU’s secretariat. SBU has determined that the conditions described in the submissions are compatible with SBU’s requirements for objectivity and impartiality.
The full report in Swedish
The full report in Swedish, Mat vid diabetes.
Project group
Experts
- Mette Axelsen, Associate Professor, Clinical Nutrition Physiologist, Chairman
- Lars Ellegård, Associate Professor, Senior Consultant, Sahlgrenska University Hospital
- Åsa Hörnsten, Professor Umeå University
- David Iggman, M.D., Ph.D. General practitioner, researcher, Norslund-Svärdsjö Academic Primary Health Care Center
- Ingrid Larsson, Associate Professor Sahlgrenska University Hospital
- Ulf Risérus, PhD, Associate Professor, Uppsala University
- Emily Sonestedt, Associate Professor, Associate Senior Lecturer, Lund University
- Åsa Tornberg, Associate Professor, Senior Lecturer, Lund University
SBU
- Göran Bertilsson, Project Manager
- Annicka Hedman, assisting Project Manager
- Anna Ringborg and Martina Lundqvist, Health Economists
- Anna Attergren Granath, Project Coordinator
External reviewers
- Upon request
Flow charts
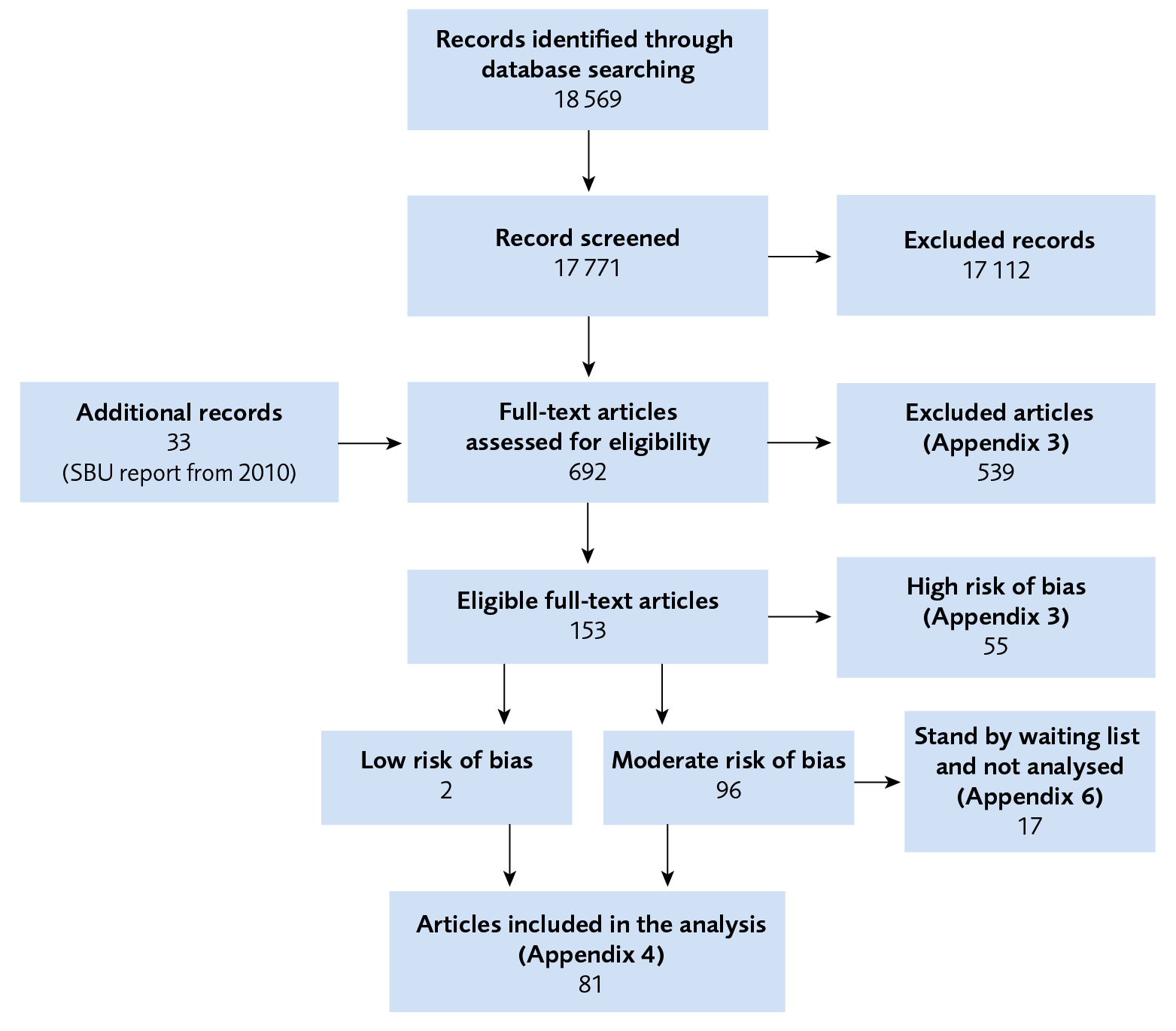
Figure 1 Flow chart of included studies.
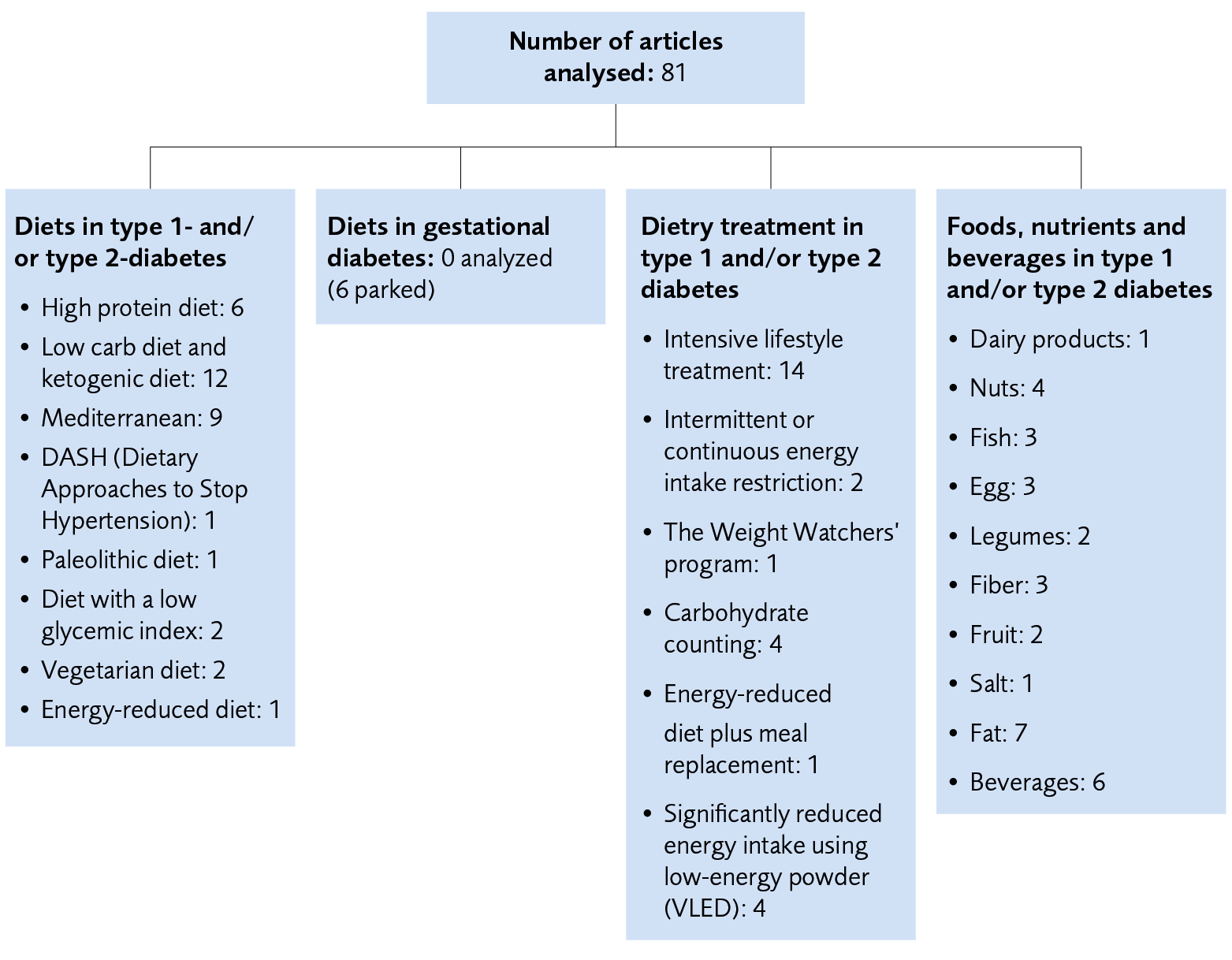
Figure 2 Overview of the number of included articles for the diets, dietary treatments, foods, nutrients, and beverages included in the result.
References
- SBU. Mat vid diabetes.: en systematisk översikt och utvärdering av medicinska, hälsoekonomiska, sociala och etiska aspekter. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2022. SBU Utvärderar 345. [accessed May 12 2022]. Available from: https://www.sbu.se/345.
- SBU. Mat vid diabetes. En systematisk litteraturöversikt. Stockholm: Statens beredning för medicinsk utvärdering (SBU); 2010. SBU Utvärderar 201. [accessed Okt 19 2021]. Available from: https://www.sbu.se/matviddiabetes.
- SBU. Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten: en metodbok. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2020. [accessed 15 jun 2020]. Available from: http://www.sbu.se/sv/var-metod/.
- GRADE handbook for grading quality of evidence and strength of recommendations. 2013. [updated October 2013. ; accessed Feb 20 2021].
- Nothlings U, Schulze MB, Weikert C, Boeing H, van der Schouw YT, Bamia C, et al. Intake of vegetables, legumes, and fruit, and risk for all-cause, cardiovascular, and cancer mortality in a European diabetic population. J Nutr. 2008;138(4):775-81. Available from: https://doi.org/138/4/775 [pii].
- Sluik D, Boeing H, Li K, Kaaks R, Johnsen NF, Tjonneland A, et al. Lifestyle factors and mortality risk in individuals with diabetes mellitus: are the associations different from those in individuals without diabetes? Diabetologia. 2014;57(1):63-72. Available from: https://doi.org/10.1007/s00125-013-3074-y.
- Burger KN, Beulens JW, van der Schouw YT, Sluijs I, Spijkerman AM, Sluik D, et al. Dietary fiber, carbohydrate quality and quantity, and mortality risk of individuals with diabetes mellitus. PLoS One. 2012;7(8):e43127. Available from: https://doi.org/10.1371/journal.pone.0043127.
- He M, van Dam RM, Rimm E, Hu FB, Qi L. Whole-grain, cereal fiber, bran, and germ intake and the risks of all-cause and cardiovascular disease-specific mortality among women with type 2 diabetes mellitus. Circulation. 2010;121(20):2162-8. Available from: https://doi.org/10.1161/CIRCULATIONAHA.109.907360.
- Schoenaker DA, Toeller M, Chaturvedi N, Fuller JH, Soedamah-Muthu SS, Group EPCS. Dietary saturated fat and fibre and risk of cardiovascular disease and all-cause mortality among type 1 diabetic patients: the EURODIAB Prospective Complications Study. Diabetologia. 2012;55(8):2132-41. Available from: https://doi.org/10.1007/s00125-012-2550-0.
- Bidel S, Hu G, Qiao Q, Jousilahti P, Antikainen R, Tuomilehto J. Coffee consumption and risk of total and cardiovascular mortality among patients with type 2 diabetes. Diabetologia. 2006;49(11):2618-26. Available from: https://doi.org/10.1007/s00125-006-0435-9 [doi].
- Komorita Y, Iwase M, Fujii H, Ohkuma T, Ide H, Jodai-Kitamura T, et al. Additive effects of green tea and coffee on all-cause mortality in patients with type 2 diabetes mellitus: the Fukuoka Diabetes Registry. BMJ Open Diabetes Res Care. 2020;8(1):10. Available from: https://doi.org/10.1136/bmjdrc-2020-001252.
- Zhang W, Lopez-Garcia E, Li TY, Hu FB, van Dam RM. Coffee consumption and risk of cardiovascular diseases and all-cause mortality among men with type 2 diabetes. Diabetes Care. 2009;32(6):1043-5. Available from: https://doi.org/10.2337/dc08-2251.
- Zhang WL, Lopez-Garcia E, Li TY, Hu FB, van Dam RM. Coffee consumption and risk of cardiovascular events and all-cause mortality among women with type 2 diabetes. Diabetologia. 2009;52(5):810-7. Available from: https://doi.org/10.1007/s00125-009-1311-1.
- Liu G, Guasch-Ferre M, Hu Y, Li Y, Hu FB, Rimm EB, et al. Nut Consumption in Relation to Cardiovascular Disease Incidence and Mortality Among Patients With Diabetes Mellitus. Circ Res. 2019;124(6):920-9. Available from: https://doi.org/10.1161/CIRCRESAHA.118.314316.
- Li TY, Brennan AM, Wedick NM, Mantzoros C, Rifai N, Hu FB. Regular consumption of nuts is associated with a lower risk of cardiovascular disease in women with type 2 diabetes. J Nutr. 2009;139(7):1333-8. Available from: https://doi.org/10.3945/jn.108.103622.
- Campmans-Kuijpers MJ, Sluijs I, Nothlings U, Freisling H, Overvad K, Boeing H, et al. The association of substituting carbohydrates with total fat and different types of fatty acids with mortality and weight change among diabetes patients. Clin Nutr. 2016;35(5):1096-102. Available from: https://doi.org/10.1016/j.clnu.2015.08.003.
- Jiao J, Liu G, Shin HJ, Hu FB, Rimm EB, Rexrode KM, et al. Dietary fats and mortality among patients with type 2 diabetes: analysis in two population based cohort studies. BMJ. 2019;366:l4009. Available from: https://doi.org/10.1136/bmj.l4009.
- Trichopoulou A, Psaltopoulou T, Orfanos P, Trichopoulos D. Diet and physical activity in relation to overall mortality amongst adult diabetics in a general population cohort. J Intern Med. 2006;259(6):583-91. Available from: https://doi.org/10.1111/j.1365-2796.2006.01638.x.
- SBU. Mat vid fetma. En systematisk litteraturöversikt. Stockholm: Statens beredning för medicinsk utvärdering (SBU); 2013. SBU Utvärderar 218. [accessed Okt 19 2021]. Available from: https://www.sbu.se/218.

 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services
 Share on Facebook
Share on Facebook
 Share on LinkedIn
Share on LinkedIn
 Share via Email
Share via Email