Treatment methods for rehabilitation of fibromyalgia
A systematic review
Conclusions
- Few high-quality studies of treatments for fibromyalgia study long-term effects on health. We identified some studies of psychological therapies, psycho-educative interventions, interventions that promote physical activity and acupuncture. However, the studies identified were too few and too small to allow us to reliably judge the health effects of the interventions.
- Results for two pharmacological substances, Duloxetine and Pregabalin show that, when measured three months after initiated treatment, patients assess themselves as improved (low certainty of evidence); that Duloxetine can reduce pain interference and depressive symptoms (low certainty of evidence); and that Pregabalin can reduce symptoms of fibromyalgia and pain intensity, and improve sleep quality (low certainty of evidence)..
Comment
Participants in the included studies may differ somewhat from fibromyalgia patients in the clinic today. A majority of the studies established a diagnosis of fibromyalgia using the 1990 criteria from American College of Rheumatology (ACR-1990). The criteria have been revised since and differences between the earlier and later versions of the ACR-criteria affect who gets diagnosed. Moreover, in the clinic patients often have comorbid conditions in addition to fibromyalgia.
The differences between fibromyalgia patients diagnosed with fibromyalgia before and after the criteria changed, as well as the presence of comorbid conditions, may affect both the need for, and the effects of treatments. Investigations of treatment effects in such subgroups of fibromyalgia patients are needed.
Background
Fibromyalgia is characterized by widespread musculoskeletal pain. In addition, people with fibromyalgia often experience sleep problems and fatigue. Comorbidity with depression and anxiety is common. There is no cure for fibromyalgia, rather the goal of treatment is to improve health and to restore function and quality of life.
Aim
The aim of the review is to present the current evidence for long-term effects on health of treatments used for rehabilitation of people with fibromyalgia, measured as quality of life, physical, psychological and social function, and pain.
The review did not include multimodal or multidisciplinary forms of rehabilitation which are instead covered in www.sbu.se/341e
Method
A systematic review was conducted in accordance with the PRISMA statement. The protocol is registered in Prospero. The certainty of evidence was assessed with GRADE.
Inclusion criteria
The review was limited to treatments of relevance for Swedish healthcare and to treatments used for long-term improvement of fibromyalgia. Studies had to fulfil the following criteria for inclusion in the review:
- Population – adults (≥18 years) diagnosed with fibromyalgia.
- Intervention – treatments aimed at improving fibromyalgia or consequences of the condition
- Control – other relevant treatments, no treatment, or treatment as usual.
- Outcomes – effects on health:pain, quality of life, and mental, physical or social function
- Study design – prospective and controlled clinical trials, with or without randomised allocation
- Length of follow-up – at least three months after initiated treatment. In addition, temporary interventions, i.e. all treatments except continuous pharmacological therapies, must report a follow-up directly after termination of treatment
- Language – English, Swedish, Danish or Norwegian
Exclusion criteria
We chose not to include:
- Studies that allowed participants with other primary conditions, apart from fibromyalgia
- Studies with fewer than 20 participants per comparison group
Search period: From 2000 to 2021. Final search February, 2021.
Databases searched: Cochrane (Wiley), Embase (Elsevier), Medline (OvidSP), PsycINFO (Ebsco), Scopus (Elsevier) and CINAHL (Ebsco).
Risk of bias
All relevant studies were assessed for risk of bias. Studies with results assessed as of low or moderate risk of bias were included in analyses. Studies with results assessed as of high risk of bias were not included.
Client/patient involvement: No
Results
A total of 34 studies are included in the assessments of health effects of different treatments:
- Pharmacological substances: 6 studies
- Psychological therapies: 15 studies
- Physical activity and acupuncture: 9 studies
- Psychoeducation: 4 studies
Interventions investigated in at least two studies are included in the assessments of health effects. We also identified interventions for which we only could include a single study. They were not assessed but we report them for information. Studies which investigated effects of multimodal treatments are reported in [länk till eng. sammanfattning av rapporten om multimodal behandling].
Pharmacological treatments
We evaluated the effects of two different substances for long-term improvement of fibromyalgia symptoms: duloxetine and pregabalin. For both substances the assessments included three original studies.
| FIQ = Fibromyalgia Impact Questionnaire, QoL = Quality of Life * Results from the review: ↑ = Better effect; ↓ = Less effect; ↔ = No detectable effect (statistical test result of p >0.05 for a difference in effect between comparison groups). ** Evaluation of the strength of evidence of a result according to GRADE: ⊕⊕⊕⊕ = High; ⊕⊕⊕◯ = Moderate; ⊕⊕◯◯ = Low; ⊕◯◯◯ = Very low (meaning that the trustworthiness of the result is very low and can’t be used to evaluate the true effect – even if a statistical test reached p <0.05). |
|||||
| Outcome | Duloxetine 3 months after initiation of treatment |
Pregabalin 3 months after initiation of treatment |
|||
| Fibromyalgia symptoms | FIQ | ↑* | ⊕◯◯◯** | ↑* | ⊕⊕◯◯** |
| Quality of Life | Mental QoL | ↑ | ⊕⊕◯◯ | ↔ | ⊕◯◯◯ |
| Physical QoL | ↔ | ⊕◯◯◯ | ↔ | ⊕◯◯◯ | |
| Global change | ↑ | ⊕◯◯◯ | ↑ | ⊕⊕◯◯ | |
| Body Functions | |||||
| Pain | Pain intensity | ↔ | ⊕◯◯◯ | ↑ | ⊕⊕◯◯ |
| Pain interference | ↑ | ⊕⊕◯◯ | |||
| Psychological symptoms | Depression | ↑ | ⊕⊕◯◯ | ↔ | ⊕◯◯◯ |
| Anxiety | ↔ | ⊕◯◯◯ | ↑ | ⊕◯◯◯ | |
| Sleep Quality | ↑ | ⊕⊕◯◯ | |||
| Fatigue | ↑ | ⊕◯◯◯ | ↔ | ⊕◯◯◯ | |
| Mental and physical Function | Cognitive och Physical function | ↔ | ⊕◯◯◯ | ||
Psychological treatments
We evaluated the effects of Cognitive Behavioral Therapy (CBT), Acceptance and Commitment Therapy (ACT) and Mindfulness Based Stress Reduction (MBSR). The assessment of CBT, ACT, and MBSR included eight, two, and five studies respectively.
| FIQ = Fibromyalgia Impact Questionnaire; QoL = Quality of Life * Results from the review: ↑ = Better effect; ↓ = Less effect; ↔ = No detectable effect (statistical test result of p >0.05 for a difference in effect between comparison groups). ** Evaluation of the strength of evidence of a result according to GRADE: ⊕⊕⊕⊕ = High; ⊕⊕⊕◯ = Moderate; ⊕⊕◯◯ = Low; ⊕◯◯◯ = Very low (meaning that the trustworthiness of the result is very low and can’t be used to evaluate the true effect – even if a statistical test reached p <0.05). |
|||||||
| Outcome | CBT 3–6 months after end of treatment |
ACT 3 months after end of treatment |
MBSR 2–10 months after end of treatment |
||||
| Fibromyalgia symptoms | FIQ | ↔* | ⊕◯◯◯** | ↑* | ⊕◯◯◯** | ↑* | ⊕◯◯◯** |
| Quality of Life | Global QoL | ↔ | ⊕◯◯◯ | ↓ | ⊕◯◯◯ | ||
| Mental QoL | ↔ | ⊕◯◯◯ | |||||
| Physical QoL | ↔ | ⊕◯◯◯ | |||||
| Body Functions | |||||||
| Pain | Pain Intensity | ↔ | ⊕◯◯◯ | ↔ | ⊕◯◯◯ | ↔ | ⊕◯◯◯ |
| Pain Interference | ↔ | ⊕◯◯◯ | |||||
| Psychological symptoms | Depression | ↔ | ⊕◯◯◯ | ↑ | ⊕◯◯◯ | ↔ | ⊕◯◯◯ |
| Anxiety | ↔ | ⊕◯◯◯ | ↔ | ⊕◯◯◯ | |||
| Stress/Distress | ↑ | ⊕◯◯◯ | |||||
| Catastrophising | ↔ | ⊕◯◯◯ | ↔ | ⊕◯◯◯ | ↑ | ⊕◯◯◯ | |
| Sleep problems | ↑ | ⊕◯◯◯ | ↔ | ⊕◯◯◯ | ↔ | ⊕◯◯◯ | |
| Activities and Participation | |||||||
| Impairment | Physical | ↔ | ⊕◯◯◯ | ||||
| Cognitive | ↑ | ⊕◯◯◯ | |||||
| Personal Factors | |||||||
| Coping | Self efficacy | ↑ | ⊕◯◯◯ | ||||
| Coping with sleep | ↓ | ⊕◯◯◯ | |||||
| Acceptance | ↑ | ⊕◯◯◯ | ↑ | ⊕◯◯◯ | |||
Physical activity and Acupuncture
We evaluated the effects of guided physical activity (physical activity under guidance from a physiotherapist or other therapist) and of Acupuncture. The assessment of guided physical activity included nine studies, and the assessment of acupuncture included three studies.
| FIQ = Fibromyalgia Impact Questionnaire; QoLADL = Activities of Daily Life * Results from the review: ↑ = Better effect; ↓ = Less effect; ↔ = No detectable effect (statistical test result of p >0.05 for a difference in effect between comparison groups). ** Evaluation of the strength of evidence of a result according to GRADE: ⊕⊕⊕⊕ = High; ⊕⊕⊕◯ = Moderate; ⊕⊕◯◯ = Low; ⊕◯◯◯ = Very low (meaning that the trustworthiness of the result is very low and can’t be used to evaluate the true effect – even if a statistical test reached p <0.05). |
|||||
| Outcome | Guided Physical Activity 3–12 months after end of treatment |
Acupuncture 3–24 months after end of treatment |
|||
| Fibromyalgia symptoms | FIQ | ↑* | ⊕◯◯◯** | ↑* | ⊕◯◯◯** |
| Quality of Life | Mental QoL | ↔ | ⊕◯◯◯ | ||
| Physical QoL | ↔ | ⊕◯◯◯ | |||
| Gobal change | ↔ | ⊕◯◯◯ | |||
| Body Functions | |||||
| Pain | Pain intensity | ↔ | ⊕◯◯◯ | ↔ | ⊕◯◯◯ |
| Psychological symptoms | Depression | ↔ | ⊕◯◯◯ | ↓ | ⊕◯◯◯ |
| Anxiety | ↔ | ⊕◯◯◯ | |||
| Stress/Distress | ↔ | ⊕◯◯◯ | |||
| Sleep problems | ↔ | ⊕◯◯◯ | |||
| Fatigue | ↔ | ⊕◯◯◯ | ↔ | ⊕◯◯◯ | |
| Activities and Participation | |||||
| Impairment | ADL | ↔ | ⊕◯◯◯ | ||
| Personal Factors | |||||
| Coping | Acceptance | ↔ | ⊕◯◯◯ | ||
Psychoeducation
We evaluated the effects multimodal psychoeducation (psychoeducative interventions led by lecturers/therapists from several clinical professions). The assessment included four studies.
| FIQ = Fibromyalgia Impact Questionnaire; ADL = Activities of Daily Life * Results from the review: ↑ = Better effect; ↓ = Less effect; ↔ = No detectable effect (statistical test result of p >0.05 for a difference in effect between comparison groups). ** Evaluation of the strength of evidence of a result according to GRADE: ⊕⊕⊕⊕ = High; ⊕⊕⊕◯ = Moderate; ⊕⊕◯◯ = Low; ⊕◯◯◯ = Very low (meaning that the trustworthiness of the result is very low and can’t be used to evaluate the true effect – even if a statistical test reached p <0.05). |
|||
| Outcome | Psychoeducation 6–12 months after end of treatment |
||
| Fibromyalgia symptoms | FIQ | ↑* | ⊕◯◯◯** |
| Body Functions | |||
| Pain | Pain intensity | ↑ | ⊕◯◯◯ |
| Pain interference | ↑ | ⊕◯◯◯ | |
| Psychological symptoms | Depression | ↔ | ⊕◯◯◯ |
| Anxiety | ↔ | ⊕◯◯◯ | |
| Stress/Distress | ↔ | ⊕◯◯◯ | |
| Catastrophising | ↑ | ⊕◯◯◯ | |
| Activities and Participation | |||
| Impairment | ADL | ↑ | ⊕◯◯◯ |
Other treatments
In total, 19 studies were identified which were considered single studies of an intervention: other pharmacological treatments (mirtazapin, gabapentin and pregabaline in combination with amitriptyline, venlafaxine or paroxetine); psychological therapies (CBT for insomnia and Emotional Written Exposure), psychoeducative interventions, interventions for physical activity, manual therapy (myofascial release) and nerve stimulation of the brain (rTMS). The studies are listed in the report but not included in the assessments.
Conflicts of Interest
In accordance with SBU’s requirements, the experts and scientific reviewers participating in this project have submitted statements about conflicts of interest. These documents are available at SBU’s secretariat. SBU has determined that the conditions described in the submissions are compatible with SBU’s requirements for objectivity and impartiality.
The full report in Swedish
Project group
Experts
- Monica Buhrman, Ph D., Associate Professor
- Diana Kadetoff, Ph D.
- Björn Äng, Ph D, Professor
From SBU
- Anna Christensson, Project Manager
- Martin Norman, Assistant Project Manager
- Susanne Johansson, Assistant Project Manager (until May 2020)
- Jessica Dagerhamn, Assistant Project Manager
- Anna Attergren Granath, Project Administrator
- Agneta Brolund, Information Specialist (until December 2020)
- Carl Gornitzki, Information Specialist (from January 2021)
Scientific reviewers
- Mari Lundberg, Ph D., Professor
- Hans Westergren, Ph D., Associate Professor
Flow chart
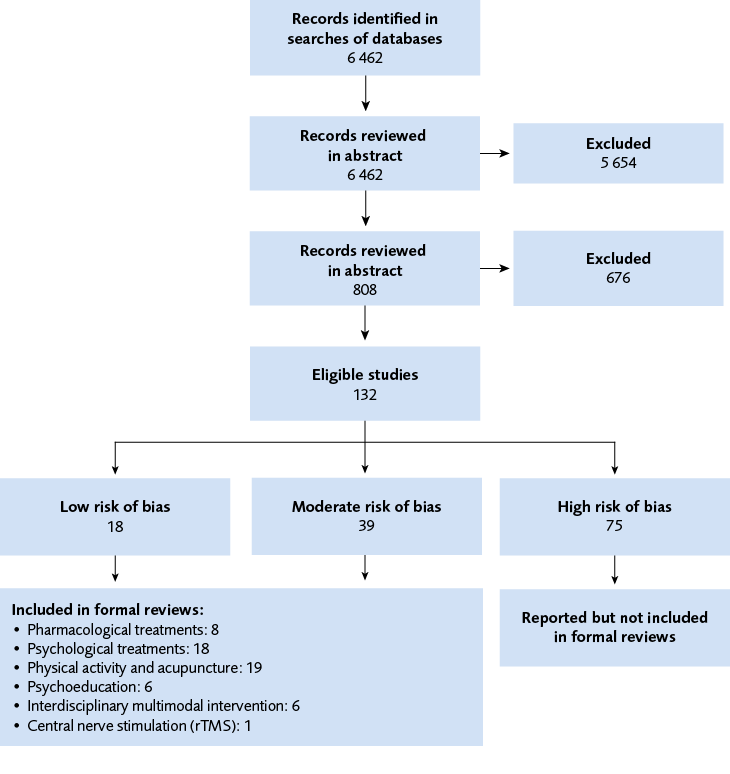
Figure 1 Flow chart.
References
- Jensen TS, Baron R, Haanpää M, Kalso E, Loeser JD, Rice ASC, et al. A new definition of neuropathic pain. Pain. 2011;152(10):2204-5. Available from: https://doi.org/10.1016/j.pain.2011.06.017.
- (IASP) TIAftSoP. IASP Terminology.
- Läkemedelsverket. Läkemedelsbehandling av långvarig smärta hos barn och vuxna – behandlingsrekommendation. Information från läkemedelsverket. 2017(3).
- Bellato E, Marini E, Castoldi F, Barbasetti N, Mattei L, Bonasia DE, et al. Fibromyalgia syndrome: etiology, pathogenesis, diagnosis, and treatment. Pain Res Treat. 2012;2012:426130. Available from: https://doi.org/10.1155/2012/426130.
- Kosek E, Lampa J, Nisell R, editors. Smärta och inflammation vid reumatiska sjukdomar och vanliga smärttillstånd i rörelseapparaten: Studentlitteratur; 2014.
- Arnold LM, Bennett RM, Crofford LJ, Dean LE, Clauw DJ, Goldenberg DL, et al. AAPT Diagnostic Criteria for Fibromyalgia. J Pain. 2019;20(6):611-28. Available from: https://doi.org/10.1016/j.jpain.2018.10.008.
- Theoharides TC, Tsilioni I, Arbetman L, Panagiotidou S, Stewart JM, Gleason RM, et al. Fibromyalgia syndrome in need of effective treatments. J Pharmacol Exp Ther. 2015;355(2):255-63. Available from: https://doi.org/10.1124/jpet.115.227298.
- Galvez-Sánchez CM, Duschek S, Reyes Del Paso GA. Psychological impact of fibromyalgia: current perspectives. Psychol Res Behav Manag. 2019;12:117-27. Available from: https://doi.org/10.2147/prbm.S178240.
- Palstam A, Mannerkorpi K. Work Ability in Fibromyalgia: An Update in the 21st Century. Curr Rheumatol Rev. 2017;13(3):180-7. Available from: https://doi.org/10.2174/1573397113666170502152955.
- Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis and rheumatism. 1990;33(2):160-72.
- Quintner J. Why Are Women with Fibromyalgia so Stigmatized? Pain Med. 2020;21(5):882-8. Available from: https://doi.org/10.1093/pm/pnz350.
- Creed F. A review of the incidence and risk factors for fibromyalgia and chronic widespread pain in population-based studies. Pain. 2020;161(6):1169-76. Available from: https://doi.org/10.1097/j.pain.0000000000001819.
- Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Katz RS, Mease P, et al. The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res (Hoboken). 2010;62(5):600-10. Available from: https://doi.org/10.1002/acr.20140.
- Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Hauser W, Katz RL, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Seminars in arthritis and rheumatism. 2016;46(3):319-29. Available from: https://doi.org/10.1016/j.semarthrit.2016.08.012.
- Rheumatology ACo. ACR-Endorsed Criteria: Fibromyalgia. [Available from: https://www.rheumatology.org/Practice-Quality/Clinical-Support/Criteria.
- Kosek E, Lampa J, Nisell R. Smärta och inflammation: vid reumatiska sjukdomar och vanliga smärttillstånd i rörelseapparaten: Studentlitteratur; 2019.
- Borchers AT, Gershwin ME. Fibromyalgia: A Critical and Comprehensive Review. Clin Rev Allergy Immunol. 2015;49(2):100-51. Available from: https://doi.org/10.1007/s12016-015-8509-4.
- Lichtenstein A, Tiosano S, Amital H. The complexities of fibromyalgia and its comorbidities. Curr Opin Rheumatol. 2018;30(1):94-100. Available from: https://doi.org/10.1097/bor.0000000000000464.
- Verbunt JA, Pernot DH, Smeets RJ. Disability and quality of life in patients with fibromyalgia. Health Qual Life Outcomes. 2008;6:8. Available from: https://doi.org/10.1186/1477-7525-6-8.
- Ofluoglu D, Berker N, Güven Z, Canbulat N, Yilmaz IT, Kayhan O. Quality of life in patients with fibromyalgia syndrome and rheumatoid arthritis. Clin Rheumatol. 2005;24(5):490-2. Available from: https://doi.org/10.1007/s10067-004-1068-3.
- Lee JW, Lee KE, Park DJ, Kim SH, Nah SS, Lee JH, et al. Determinants of quality of life in patients with fibromyalgia: A structural equation modeling approach. PLoS One. 2017;12(2):e0171186. Available from: https://doi.org/10.1371/journal.pone.0171186.
- Mascarenhas RO, Souza MB, Oliveira MX, Lacerda AC, Mendonça VA, Henschke N, et al. Association of Therapies With Reduced Pain and Improved Quality of Life in Patients With Fibromyalgia: A Systematic Review and Meta-analysis. JAMA Intern Med. 2021;181(1):104-12. Available from: https://doi.org/10.1001/jamainternmed.2020.5651.
- Knight T, Schaefer C, Chandran A, Zlateva G, Winkelmann A, Perrot S. Health-resource use and costs associated with fibromyalgia in France, Germany, and the United States. Clinicoecon Outcomes Res. 2013;5:171-80. Available from: https://doi.org/10.2147/ceor.S41111.
- White KP, Speechley M, Harth M, Ostbye T. The London Fibromyalgia Epidemiology Study: direct health care costs of fibromyalgia syndrome in London, Canada. J Rheumatol. 1999;26(4):885-9.
- Doron Y, Peleg R, Peleg A, Neumann L, Buskila D. The clinical and economic burden of fibromyalgia compared with diabetes mellitus and hypertension among Bedouin women in the Negev. Fam Pract. 2004;21(4):415-9. Available from: https://doi.org/10.1093/fampra/cmh411.
- Winkelmann A, Perrot S, Schaefer C, Ryan K, Chandran A, Sadosky A, et al. Impact of fibromyalgia severity on health economic costs: results from a European cross-sectional study. Appl Health Econ Health Policy. 2011;9(2):125-36. Available from: https://doi.org/10.2165/11535250-000000000-00000.
- Engel GL. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980;137(5):535-44. Available from: https://doi.org/10.1176/ajp.137.5.535.
- Macfarlane GJ, Kronisch C, Dean LE, Atzeni F, Häuser W, Fluß E, et al. EULAR revised recommendations for the management of fibromyalgia. Ann Rheum Dis. 2017;76(2):318-28. Available from: https://doi.org/10.1136/annrheumdis-2016-209724.
- Arnold LM, Clauw DJ, Dunegan LJ, Turk DC. A framework for fibromyalgia management for primary care providers. Mayo Clin Proc. 2012;87(5):488-96. Available from: https://doi.org/10.1016/j.mayocp.2012.02.010.
- Kerns RD, Sellinger J, Goodin BR. Psychological treatment of chronic pain. Annu Rev Clin Psychol. 2011;7:411-34. Available from: https://doi.org/10.1146/annurev-clinpsy-090310-120430.
- Hofmann SG, Asnaani A, Vonk IJ, Sawyer AT, Fang A. The Efficacy of Cognitive Behavioral Therapy: A Review of Meta-analyses. Cognit Ther Res. 2012;36(5):427-40. Available from: https://doi.org/10.1007/s10608-012-9476-1.
- Sturgeon JA. Psychological therapies for the management of chronic pain. Psychol Res Behav Manag. 2014;7:115-24. Available from: https://doi.org/10.2147/prbm.S44762.
- Hayes S, Strosahl K, Wilson K. Acceptance and commitment therapy: An experiential approach to behavior change.: Guilford Press; 1999.
- Hughes LS, Clark J, Colclough JA, Dale E, McMillan D. Acceptance and Commitment Therapy (ACT) for Chronic Pain: A Systematic Review and Meta-Analyses. Clin J Pain. 2017;33(6):552-68. Available from: https://doi.org/10.1097/ajp.0000000000000425.
- Kabat-Zinn J. Full catastrophe living: Using the wisdom of your body and mind to face stress, pain and illness. New York, NY: Delacorte; 1990. 512 p.
- Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, et al. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-analysis. Annals of Behavioral Medicine. 2016;51(2):199-213. Available from: https://doi.org/10.1007/s12160-016-9844-2.
- Csaszar N, Bagdi P, Stoll D, Szoke H. Pain and Psychotherapy, in the Light of Evidence of Psychological Treatment Methods of Chronic Pain Based on Evidence. J Psychol Psychother. 2014;4(3). Available from: https://doi.org/DOI: 10.4172/2161-0487.1000145.
- WHO. Physical activity fact sheet. Geneva: World Health Organization; 2021. Available from: https://apps.who.int/iris/handle/10665/346252.
- YFA. Fysisk aktivitet vid långvariga utbredda smärttillstånd; 2016. Fysisk aktivitet vid långvariga utbredda smärttillstånd Available from: http://www.fyss.se/wp-content/uploads/2018/01/Sm%C3%A4rttillst%C3%A5nd-l%C3%A5ngvariga-utbredda.pdf.
- Aarsland D, Sardahaee FS, Anderssen S, Ballard C. Is physical activity a potential preventive factor for vascular dementia? A systematic review. Aging Ment Health. 2010;14(4):386-95. Available from: https://doi.org/10.1080/13607860903586136.
- Pedersen BK, Saltin B. Exercise as medicine - evidence for prescribing exercise as therapy in 26 different chronic diseases. Scand J Med Sci Sports. 2015;25 Suppl 3:1-72. Available from: https://doi.org/10.1111/sms.12581.
- Ambrose KR, Golightly YM. Physical exercise as non-pharmacological treatment of chronic pain: Why and when. Best Pract Res Clin Rheumatol. 2015;29(1):120-30. Available from: https://doi.org/10.1016/j.berh.2015.04.022.
- Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2(2):1143-211. Available from: https://doi.org/10.1002/cphy.c110025.
- Häuser W, Klose P, Langhorst J, Moradi B, Steinbach M, Schiltenwolf M, et al. Efficacy of different types of aerobic exercise in fibromyalgia syndrome: a systematic review and meta-analysis of randomised controlled trials. Arthritis Res Ther. 2010;12(3):R79. Available from: https://doi.org/10.1186/ar3002.
- Mannerkorpi K, Nordeman L, Cider A, Jonsson G. Does moderate-to-high intensity Nordic walking improve functional capacity and pain in fibromyalgia? A prospective randomized controlled trial. Arthritis Res Ther. 2010;12(5):R189. Available from: https://doi.org/10.1186/ar3159.
- SBU. Metoder för behandling av långvarig smärta. En systematisk litteraturöversikt.; 2006 ISBN 91-85413-08-9; ISSN 1400-1403. Available from: https://www.sbu.se/sv/publikationer/SBU-utvarderar/metoder-for-behandling-av-langvarig-smarta/.
- SBU. Rehabilitering vid långvarig smärta. En systematisk litteraturöversikt. . SBU; 2010.
- SBU. Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten: en metodbok. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2020. [accessed May 20 2021]. Available from: https://www.sbu.se/metodbok.
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. Available from: https://doi.org/10.1371/journal.pmed.1000097.
- McGuinness LA, Higgins JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Synth Methods. 2021;12(1):55-61. Available from: https://doi.org/10.1002/jrsm.1411.
- WHO. International classification of functioning, disability and health : ICF. World Health Organization2001
- Socialstyrelsen. Internationell klassifikation av funktionstillstånd, funktionshinder och hälsa (ICF). Svensk version 2021 av International Classification of Functioning, Disability and Health (ICF). Socialstyrelsen; 2021.
- Bennett RM, Bushmakin AG, Cappelleri JC, Zlateva G, Sadosky AB. Minimal clinically important difference in the fibromyalgia impact questionnaire. J Rheumatol. 2009;36(6):1304-11. Available from: https://doi.org/10.3899/jrheum.081090.
- Murakami M, Osada K, Mizuno H, Ochiai T, Alev L, Nishioka K. A randomized, double-blind, placebo-controlled phase III trial of duloxetine in Japanese fibromyalgia patients. Arthritis Res Ther. 2015;17(1):224. Available from: https://doi.org/10.1186/s13075-015-0718-y.
- Arnold LM, Zhang S, Pangallo BA. Efficacy and safety of duloxetine 30 mg/d in patients with fibromyalgia: a randomized, double-blind, placebo-controlled study. Clin J Pain. 2012;28(9):775-81. Available from: https://doi.org/10.1097/AJP.0b013e3182510295.
- Arnold LM, Clauw D, Wang F, Ahl J, Gaynor PJ, Wohlreich MM. Flexible dosed duloxetine in the treatment of fibromyalgia: a randomized, double-blind, placebo-controlled trial. J Rheumatol. 2010;37(12):2578-86. Available from: https://doi.org/10.3899/jrheum.100365.
- Ohta H, Oka H, Usui C, Ohkura M, Suzuki M, Nishioka K. A randomized, double-blind, multicenter, placebo-controlled phase III trial to evaluate the efficacy and safety of pregabalin in Japanese patients with fibromyalgia. Arthritis Res Ther. 2012;14(5):R217. Available from: https://doi.org/10.1186/ar4056.
- Arnold LM, Russell IJ, Diri EW, Duan WR, Young JP, Jr., Sharma U, et al. A 14-week, randomized, double-blinded, placebo-controlled monotherapy trial of pregabalin in patients with fibromyalgia. J Pain. 2008;9(9):792-805. Available from: https://doi.org/10.1016/j.jpain.2008.03.013.
- Pauer L, Winkelmann A, Arsenault P, Jespersen A, Whelan L, Atkinson G, et al. An international, randomized, double-blind, placebo-controlled, phase III trial of pregabalin monotherapy in treatment of patients with fibromyalgia. J Rheumatol. 2011;38(12):2643-52. Available from: https://doi.org/10.3899/jrheum.110569.
- Ohta H, Oka H, Usui C, Ohkura M, Suzuki M, Nishioka K. An open-label long-term phase III extension trial to evaluate the safety and efficacy of pregabalin in Japanese patients with fibromyalgia. Mod Rheumatol. 2013;23(6):1108-15. Available from: https://doi.org/10.1007/s10165-012-0803-x.
- Vallejo MA, Ortega J, Rivera J, Comeche MI, Vallejo-Slocker L. Internet versus face-to-face group cognitive-behavioral therapy for fibromyalgia: A randomized control trial. J Psychiatr Res. 2015;68:106-13. Available from: https://doi.org/10.1016/j.jpsychires.2015.06.006.
- Woolfolk RL, Allen LA, Apter JT. Affective-cognitive behavioral therapy for fibromyalgia: a randomized controlled trial. Pain Res Treat. 2012;2012:937873. Available from: https://doi.org/10.1155/2012/937873.
- Karlsson B, Burell G, Anderberg UM, Svärdsudd K. Cognitive behaviour therapy in women with fibromyalgia: A randomized clinical trial. Scand J Pain. 2015;9(1):11-21. Available from: https://doi.org/10.1016/j.sjpain.2015.04.027.
- McCrae CS, Williams J, Roditi D, Anderson R, Mundt JM, Miller MB, et al. Cognitive behavioral treatments for insomnia and pain in adults with comorbid chronic insomnia and fibromyalgia: clinical outcomes from the SPIN randomized controlled trial. Sleep. 2019;42(3). Available from: https://doi.org/10.1093/sleep/zsy234.
- Alda M, Luciano JV, Andrés E, Serrano-Blanco A, Rodero B, del Hoyo YL, et al. Effectiveness of cognitive behaviour therapy for the treatment of catastrophisation in patients with fibromyalgia: a randomised controlled trial. Arthritis Res Ther. 2011;13(5):R173. Available from: https://doi.org/10.1186/ar3496.
- Castel A, Cascón R, Padrol A, Sala J, Rull M. Multicomponent cognitive-behavioral group therapy with hypnosis for the treatment of fibromyalgia: long-term outcome. J Pain. 2012;13(3):255-65. Available from: https://doi.org/10.1016/j.jpain.2011.11.005.
- Falcao D, Sales L, Leite J, Feldman D, Valim V, Natour J. Cognitive behavioral therapy for the treatment of fibromyalgia syndrome: a randomized controlled trial. Journal of Musculoskeletal Pain. 2008;16(3):133-40.
- Lumley MA, Schubiner H, Lockhart NA, Kidwell KM, Harte SE, Clauw DJ, et al. Emotional awareness and expression therapy, cognitive behavioral therapy, and education for fibromyalgia: a cluster-randomized controlled trial. Pain. 2017;158(12):2354-63. Available from: https://doi.org/10.1097/j.pain.0000000000001036.
- Luciano JV, Guallar JA, Aguado J, López-Del-Hoyo Y, Olivan B, Magallón R, et al. Effectiveness of group acceptance and commitment therapy for fibromyalgia: a 6-month randomized controlled trial (EFFIGACT study). Pain. 2014;155(4):693-702. Available from: https://doi.org/10.1016/j.pain.2013.12.029.
- Simister HD, Tkachuk GA, Shay BL, Vincent N, Pear JJ, Skrabek RQ. Randomized Controlled Trial of Online Acceptance and Commitment Therapy for Fibromyalgia. J Pain. 2018;19(7):741-53. Available from: https://doi.org/10.1016/j.jpain.2018.02.004.
- Sharma M, Rush SE. Mindfulness-based stress reduction as a stress management intervention for healthy individuals: a systematic review. J Evid Based Complementary Altern Med. 2014;19(4):271-86. Available from: https://doi.org/10.1177/2156587214543143.
- Bohlmeijer E, Prenger R, Taal E, Cuijpers P. The effects of mindfulness-based stress reduction therapy on mental health of adults with a chronic medical disease: a meta-analysis. J Psychosom Res. 2010;68(6):539-44. Available from: https://doi.org/10.1016/j.jpsychores.2009.10.005.
- Sephton SE, Salmon P, Weissbecker I, Ulmer C, Floyd A, Hoover K, et al. Mindfulness meditation alleviates depressive symptoms in women with fibromyalgia: results of a randomized clinical trial. Arthritis and rheumatism. 2007;57(1):77-85. Available from: https://doi.org/10.1002/art.22478.
- Schmidt S, Grossman P, Schwarzer B, Jena S, Naumann J, Walach H. Treating fibromyalgia with mindfulness-based stress reduction: results from a 3-armed randomized controlled trial. Pain. 2011;152(2):361-9. Available from: https://doi.org/10.1016/j.pain.2010.10.043.
- Pérez-Aranda A, Feliu-Soler A, Montero-Marín J, García-Campayo J, Andrés-Rodríguez L, Borràs X, et al. A randomized controlled efficacy trial of mindfulness-based stress reduction compared with an active control group and usual care for fibromyalgia: the EUDAIMON study. Pain. 2019;160(11):2508-23. Available from: https://doi.org/10.1097/j.pain.0000000000001655.
- Cejudo J, García-Castillo FJ, Luna P, Rodrigo-Ruiz D, Feltrero R, Moreno-Gómez A. Using a Mindfulness-Based Intervention to Promote Subjective Well-Being, Trait Emotional Intelligence, Mental Health, and Resilience in Women With Fibromyalgia. Front Psychol. 2019;10:2541. Available from: https://doi.org/10.3389/fpsyg.2019.02541.
- Van Gordon W, Shonin E, Dunn TJ, Garcia-Campayo J, Griffiths MD. Meditation awareness training for the treatment of fibromyalgia syndrome: A randomized controlled trial. Br J Health Psychol. 2017;22(1):186-206. Available from: https://doi.org/10.1111/bjhp.12224.
- Paolucci T, Baldari C, Di Franco M, Didona D, Reis V, Vetrano M, et al. A New Rehabilitation Tool in Fibromyalgia: The Effects of Perceptive Rehabilitation on Pain and Function in a Clinical Randomized Controlled Trial. Evid Based Complement Alternat Med. 2016;2016:7574589. Available from: https://doi.org/10.1155/2016/7574589.
- Carson JW, Carson KM, Jones KD, Bennett RM, Wright CL, Mist SD. A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain. 2010;151(2):530-9. Available from: https://doi.org/10.1016/j.pain.2010.08.020.
- Fontaine KR, Conn L, Clauw DJ. Effects of lifestyle physical activity on perceived symptoms and physical function in adults with fibromyalgia: results of a randomized trial. Arthritis Res Ther. 2010;12(2):R55. Available from: https://doi.org/10.1186/ar2967.
- Fontaine KR, Conn L, Clauw DJ. Effects of lifestyle physical activity in adults with fibromyalgia: results at follow-up. J Clin Rheumatol. 2011;17(2):64-8. Available from: https://doi.org/10.1097/RHU.0b013e31820e7ea7.
- Carson JW, Carson KM, Jones KD, Mist SD, Bennett RM. Follow-up of yoga of awareness for fibromyalgia: results at 3 months and replication in the wait-list group. Clin J Pain. 2012;28(9):804-13. Available from: https://doi.org/10.1097/AJP.0b013e31824549b5.
- Da Costa D, Abrahamowicz M, Lowensteyn I, Bernatsky S, Dritsa M, Fitzcharles MA, et al. A randomized clinical trial of an individualized home-based exercise programme for women with fibromyalgia. Rheumatology (Oxford). 2005;44(11):1422-7. Available from: https://doi.org/10.1093/rheumatology/kei032.
- Haak T, Scott B. The effect of Qigong on fibromyalgia (FMS): a controlled randomized study. Disabil Rehabil. 2008;30(8):625-33. Available from: https://doi.org/10.1080/09638280701400540.
- Baptista AS, Villela AL, Jones A, Natour J. Effectiveness of dance in patients with fibromyalgia: a randomized, single-blind, controlled study. Clin Exp Rheumatol. 2012;30(6 Suppl 74):18-23.
- Assefi NP, Sherman KJ, Jacobsen C, Goldberg J, Smith WR, Buchwald D. A randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgia. Ann Intern Med. 2005;143(1):10-9. Available from: https://doi.org/10.7326/0003-4819-143-1-200507050-00005.
- Vas J, Santos-Rey K, Navarro-Pablo R, Modesto M, Aguilar I, Campos M, et al. Acupuncture for fibromyalgia in primary care: a randomised controlled trial. Acupunct Med. 2016;34(4):257-66. Available from: https://doi.org/10.1136/acupmed-2015-010950.
- Targino RA, Imamura M, Kaziyama HH, Souza LP, Hsing WT, Furlan AD, et al. A randomized controlled trial of acupuncture added to usual treatment for fibromyalgia. J Rehabil Med. 2008;40(7):582-8. Available from: https://doi.org/10.2340/16501977-0216.
- Baez S, Hoch MC, Hoch JM. Evaluation of Cognitive Behavioral Interventions and Psychoeducation Implemented by Rehabilitation Specialists to Treat Fear-Avoidance Beliefs in Patients With Low Back Pain: A Systematic Review. Arch Phys Med Rehabil. 2018;99(11):2287-98. Available from: https://doi.org/10.1016/j.apmr.2017.11.003.
- Scascighini L, Toma V, Dober-Spielmann S, Sprott H. Multidisciplinary treatment for chronic pain: a systematic review of interventions and outcomes. Rheumatology (Oxford). 2008;47(5):670-8. Available from: https://doi.org/10.1093/rheumatology/ken021.
- Luciano JV, Martínez N, Peñarrubia-María MT, Fernández-Vergel R, García-Campayo J, Verduras C, et al. Effectiveness of a psychoeducational treatment program implemented in general practice for fibromyalgia patients: a randomized controlled trial. Clin J Pain. 2011;27(5):383-91. Available from: https://doi.org/10.1097/AJP.0b013e31820b131c.
- Musekamp G, Gerlich C, Ehlebracht-Kï Nig I, Dorn M, A HF, Tomiak C, et al. Evaluation of a self-management patient education programme for fibromyalgia-results of a cluster-RCT in inpatient rehabilitation. Health Educ Res. 2019;34(2):209-22. Available from: https://doi.org/10.1093/her/cyy055.
- Luciano JV, Sabes-Figuera R, Cardeñosa E, M TP-M, Fernández-Vergel R, García-Campayo J, et al. Cost-utility of a psychoeducational intervention in fibromyalgia patients compared with usual care: an economic evaluation alongside a 12-month randomized controlled trial. Clin J Pain. 2013;29(8):702-11. Available from: https://doi.org/10.1097/AJP.0b013e318270f99a.
- Barrenengoa-Cuadra MJ, Muñoa-Capron-Manieux M, Fernández-Luco M, Angón-Puras L, Romón-Gómez AJ, Azkuenaga M, et al. Effectiveness of a structured group intervention based on pain neuroscience education for patients with fibromyalgia in primary care: A multicentre randomized open-label controlled trial. Eur J Pain. 2021;25(5):1137-49. Available from: https://doi.org/10.1002/ejp.1738.
- Ramzy EA. Comparative Efficacy of Newer Antidepressants in Combination with Pregabalin for Fibromyalgia Syndrome: A Controlled, Randomized Study. Pain Pract. 2017;17(1):32-40. Available from: https://doi.org/10.1111/papr.12409.
- Miki K, Murakami M, Oka H, Onozawa K, Yoshida S, Osada K. Efficacy of mirtazapine for the treatment of fibromyalgia without concomitant depression: a randomized, double-blind, placebo-controlled phase IIa study in Japan. Pain. 2016;157(9):2089-96. Available from: https://doi.org/10.1097/j.pain.0000000000000622.
- Arnold LM, Goldenberg DL, Stanford SB, Lalonde JK, Sandhu HS, Keck PE, Jr., et al. Gabapentin in the treatment of fibromyalgia: a randomized, double-blind, placebo-controlled, multicenter trial. Arthritis and rheumatism. 2007;56(4):1336-44. Available from: https://doi.org/10.1002/art.22457.
- Martínez MP, Miró E, Sánchez AI, Díaz-Piedra C, Cáliz R, Vlaeyen JW, et al. Cognitive-behavioral therapy for insomnia and sleep hygiene in fibromyalgia: a randomized controlled trial. J Behav Med. 2014;37(4):683-97. Available from: https://doi.org/10.1007/s10865-013-9520-y.
- Broderick JE, Junghaenel DU, Schwartz JE. Written emotional expression produces health benefits in fibromyalgia patients. Psychosom Med. 2005;67(2):326-34. Available from: https://doi.org/10.1097/01.psy.0000156933.04566.bd.
- Scheidt CE, Waller E, Endorf K, Schmidt S, König R, Zeeck A, et al. Is brief psychodynamic psychotherapy in primary fibromyalgia syndrome with concurrent depression an effective treatment? A randomized controlled trial. Gen Hosp Psychiatry. 2013;35(2):160-7. Available from: https://doi.org/10.1016/j.genhosppsych.2012.10.013.
- Hammond A, Freeman K. Community patient education and exercise for people with fibromyalgia: a parallel group randomized controlled trial. Clin Rehabil. 2006;20(10):835-46. Available from: https://doi.org/10.1177/0269215506072173.
- Hsu MC, Schubiner H, Lumley MA, Stracks JS, Clauw DJ, Williams DA. Sustained pain reduction through affective self-awareness in fibromyalgia: a randomized controlled trial. J Gen Intern Med. 2010;25(10):1064-70. Available from: https://doi.org/10.1007/s11606-010-1418-6.
- Stuifbergen AK, Blozis SA, Becker H, Phillips L, Timmerman G, Kullberg V, et al. A randomized controlled trial of a wellness intervention for women with fibromyalgia syndrome. Clin Rehabil. 2010;24(4):305-18. Available from: https://doi.org/10.1177/0269215509343247.
- Wang C, Schmid CH, Fielding RA, Harvey WF, Reid KF, Price LL, et al. Effect of tai chi versus aerobic exercise for fibromyalgia: comparative effectiveness randomized controlled trial. Bmj. 2018;360:k851. Available from: https://doi.org/10.1136/bmj.k851.
- Calandre EP, Rodriguez-Claro ML, Rico-Villademoros F, Vilchez JS, Hidalgo J, Delgado-Rodriguez A. Effects of pool-based exercise in fibromyalgia symptomatology and sleep quality: a prospective randomised comparison between stretching and Ai Chi. Clin Exp Rheumatol. 2009;27(5 Suppl 56):S21-8.
- Wang C, Schmid CH, Rones R, Kalish R, Yinh J, Goldenberg DL, et al. A randomized trial of tai chi for fibromyalgia. N Engl J Med. 2010;363(8):743-54. Available from: https://doi.org/10.1056/NEJMoa0912611.
- Altan L, Korkmaz N, Bingol U, Gunay B. Effect of pilates training on people with fibromyalgia syndrome: a pilot study. Arch Phys Med Rehabil. 2009;90(12):1983-8. Available from: https://doi.org/10.1016/j.apmr.2009.06.021.
- Kayo AH, Peccin MS, Sanches CM, Trevisani VF. Effectiveness of physical activity in reducing pain in patients with fibromyalgia: a blinded randomized clinical trial. Rheumatol Int. 2012;32(8):2285-92. Available from: https://doi.org/10.1007/s00296-011-1958-z.
- Richards SC, Scott DL. Prescribed exercise in people with fibromyalgia: parallel group randomised controlled trial. Bmj. 2002;325(7357):185. Available from: https://doi.org/10.1136/bmj.325.7357.185.
- Castro-Sánchez AM, Matarán-Peñarrocha GA, Granero-Molina J, Aguilera-Manrique G, Quesada-Rubio JM, Moreno-Lorenzo C. Benefits of massage-myofascial release therapy on pain, anxiety, quality of sleep, depression, and quality of life in patients with fibromyalgia. Evid Based Complement Alternat Med. 2011;2011a:561753. Available from: https://doi.org/10.1155/2011/561753.
- Castro-Sánchez AM, Matarán-Peñarrocha GA, Arroyo-Morales M, Saavedra-Hernández M, Fernández-Sola C, Moreno-Lorenzo C. Effects of myofascial release techniques on pain, physical function, and postural stability in patients with fibromyalgia: a randomized controlled trial. Clin Rehabil. 2011;25(9):800-13. Available from: https://doi.org/10.1177/0269215511399476.
- Ang DC, Kaleth AS, Bigatti S, Mazzuca SA, Jensen MP, Hilligoss J, et al. Research to encourage exercise for fibromyalgia (REEF): use of motivational interviewing, outcomes from a randomized-controlled trial. Clin J Pain. 2013;29(4):296-304. Available from: https://doi.org/10.1097/AJP.0b013e318254ac76.
- Mhalla A, Baudic S, de Andrade DC, Gautron M, Perrot S, Teixeira MJ, et al. Long-term maintenance of the analgesic effects of transcranial magnetic stimulation in fibromyalgia. Pain. 2011;152(7):1478-85. Available from: https://doi.org/10.1016/j.pain.2011.01.034.
- Bernardy K, Klose P, Welsch P, Häuser W. Efficacy, acceptability and safety of cognitive behavioural therapies in fibromyalgia syndrome - A systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2018;22(2):242-60. Available from: https://doi.org/10.1002/ejp.1121.
- Bernardy K, Klose P, Welsch P, Häuser W. Efficacy, acceptability and safety of Internet-delivered psychological therapies for fibromyalgia syndrome: A systematic review and meta-analysis of randomized controlled trials. Eur J Pain. 2019;23(1):3-14. Available from: https://doi.org/10.1002/ejp.1284.
- Haugmark T, Hagen KB, Smedslund G, Zangi HA. Mindfulness- and acceptance-based interventions for patients with fibromyalgia - A systematic review and meta-analyses. PLoS One. 2019;14(9):e0221897. Available from: https://doi.org/10.1371/journal.pone.0221897.
- Busch AJ, Barber KA, Overend TJ, Peloso PM, Schachter CL. Exercise for treating fibromyalgia syndrome. Cochrane Database Syst Rev. 2007(4):Cd003786. Available from: https://doi.org/10.1002/14651858.CD003786.pub2.
- Bidonde J, Busch AJ, Webber SC, Schachter CL, Danyliw A, Overend TJ, et al. Aquatic exercise training for fibromyalgia. Cochrane Database Syst Rev. 2014(10):Cd011336. Available from: https://doi.org/10.1002/14651858.Cd011336.
- Gómez-de-Regil L. Psychoeducation for Patients with Fibromyalgia: A Systematic Review. Healthcare (Basel). 2021;9(6). Available from: https://doi.org/10.3390/healthcare9060737.
- Keogh E. The gender context of pain. Health Psychol Rev. 2020:1-28. Available from: https://doi.org/10.1080/17437199.2020.1813602.
- Samulowitz A, Gremyr I, Eriksson E, Hensing G. "Brave Men" and "Emotional Women": A Theory-Guided Literature Review on Gender Bias in Health Care and Gendered Norms towards Patients with Chronic Pain. Pain Res Manag. 2018;2018:6358624. Available from: https://doi.org/10.1155/2018/6358624.
- Dworkin RH, Turk DC, Farrar JT, Haythornthwaite JA, Jensen MP, Katz NP, et al. Core outcome measures for chronic pain clinical trials: IMMPACT recommendations. Pain. 2005;113(1-2):9-19. Available from: https://doi.org/10.1016/j.pain.2004.09.012.
- Mease P, Arnold LM, Choy EH, Clauw DJ, Crofford LJ, Glass JM, et al. Fibromyalgia syndrome module at OMERACT 9: domain construct. J Rheumatol. 2009;36(10):2318-29. Available from: https://doi.org/10.3899/jrheum.090367.

 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services
 Share on Facebook
Share on Facebook
 Share on LinkedIn
Share on LinkedIn
 Share via Email
Share via Email