Interventions for Behaviour Change Aimed at Promoting Health in Older Adults
An Evidence Map
Main message and conclusions
A number of systematic reviews evaluating the effects of interventions to increase physical activity in older adults have been published in recent years, as have reviews on interventions for self-care in age-related health conditions. Fewer reviews have focused on other lifestyle behaviours.
Behaviour change interventions are often complex, comprising multiple components. A key challenge in synthesising studies of such interventions is providing enough detail to compare them effectively. Few reviews have used reporting tools like [69] to guide data extraction. Incorporating such tools could improve transparency and synthesis quality.
Only a minority of reviews applied a theoretical model of behaviour change. More consistent use of these models could clarify which intervention components influence behaviour and support shared knowledge development.
Aim
To map and present the current state of knowledge regarding:
- systematically compiled research on interventions for behaviour change aimed at promoting health in older adults (Figure 1), and
- the evidence concerning the effects of these interventions on behavioural and health outcomes, and the evidence gaps identified in the available research.
Background
With life expectancy continuing to rise, a growing proportion of the population is living well into old age. Although many older adults remain healthy and independent, the risk of illness and functional decline increases with age. Behaviour change interventions that promote healthy lifestyles in later life have the potential to enhance quality of life, delay the onset of disease, and reduce the need for care. These benefits make such interventions a key area for research and policy development.
Methods
We searched for, and included systematic reviews published between 2020 and October 2024 that evaluated behaviour change interventions and examined their effects on behaviour and/or health (including function and quality of life). The interventions also had to have been evaluated for older adults over the age of 65 and be feasible to offer within the framework of Swedish primary care.
The reliability of the reviews was assessed, and the risk that the results presented may have been affected by bias was rated as low, moderate, or high. Results reflecting the review authors’ conclusions about the effects of the interventions are reported for the subset of reviews assessed as having low or moderate risk of bias. Results describing the content of the interventions are reported for all included reviews.
Inclusion criteria
- Population: Older adults, aged 65 or more.
- Intervention: Interventions for behaviour change aimed at health promotion, where recipients are able to maintain the behavioural change independently after the intervention ends. In addition, the interventions had to be feasible to offer within the framework of Swedish primary care or elderly care services.
- Control: Any other or no intervention, or single group with measurements before and after the intervention.
- Outcomes: Behaviour change, physical or psychological health, function, quality of life
- Study design: Systematic reviews of controlled clinical studies
Publication languages
English, Swedish, Norwegian, Danish
Databases searched
- APA PsycInfo (EBSCO)
- CINAHL (EBSCO)
- Epistemonikos
- International HTA Database
- Ovd MEDLINE® ALL
- Scopus (Elsevier)
Results
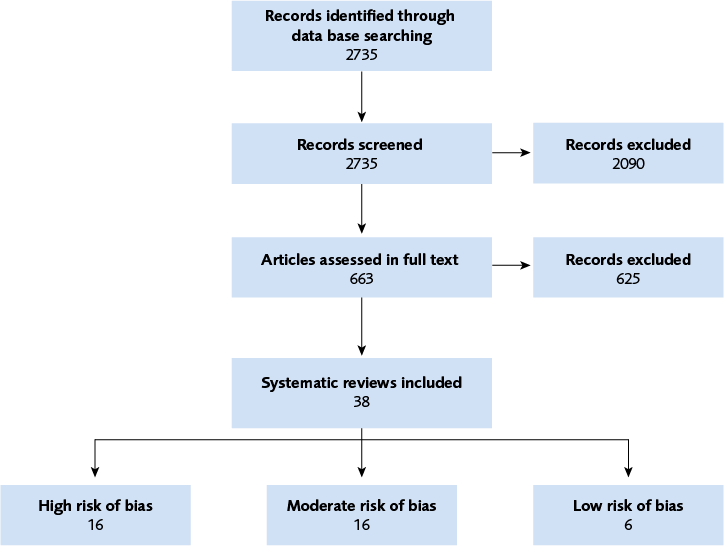
A total of thirty-eight systematic reviews are included in the evidence map (Figure 2). Most of these reviews investigated interventions aimed at increasing physical activity to improve strength, cardiorespiratory fitness, or balance in older adults. Another substantial group focused on interventions designed to support self-care in age-related health conditions, such as diabetes or cardiovascular and pulmonary diseases. A smaller number of reviews evaluated interventions targeting other healthy lifestyle behaviours [The Evidence Map].
Of the 22 reviews assessed as sufficiently reliable (i.e., with low or moderate risk of bias), 7 reported positive effects on behaviour and/or health – 4 of these evaluated self-care interventions, and 3 focused on physical activity. One review found no effect, specifically assessing remote interventions intended to promote cognition. In the remaining 14 reviews, the authors concluded that the scientific evidence was insufficient to determine whether the interventions had any effect.
The evaluated interventions were often complex, typically comprising multiple components intended to facilitate behaviour change. Within individual reviews, the interventions varied in number and type of components included – or were described so sparsely that this variability was difficult to assess. This variability and lack of detail limited the authors’ ability to synthesise findings and draw firm conclusions about the interventions’ overall effectiveness. Only a minority of the reviews used a theoretical model for behaviour change to guide their evaluation.
Conflicts of Interest
In accordance with SBU’s requirements, the experts and scientific reviewers participating in this project have submitted statements about conflicts of interest. These documents are available at SBU’s secretariat. SBU has determined that the conditions described in the submissions are compatible with SBU’s requirements for objectivity and impartiality.
The full report in Swedish
Insatser för beteendeförändring som syftar till att främja hälsa hos äldre personer
Interactive map of Interventions for Behaviour Change Aimed at Promoting Health in Older Adults
Project group
Experts
- Petra von Heideken Wågert, Licensed Physiotherapist, Professor, Mälardalen University
- Staffan Karlsson, Registered Nurse, Professor, Kristianstad University
- Johnny Pellas, Licensed Psychologist, PhD (Med), Uppsala University
SBU
- Anna Christensson, Project Director
- Annika Bring, Assistant Project Director (until January 2025)
- Liv Thalén, Assistant Project Director
- Sara Fundell, Project Administrator
- Sofia Carlsson, Project Administrator (from Mars 2025)
- Klas Moberg, Information Specialist
- Jenny Odeberg, Head of department
Flow chart
Appendices
References
- SCB. Sverige framtida befolkning 2021–2070. Statistiska centralbyrån (SCB); 2021. Demografiska rapporter 2021:1. [accessed Mar 25 2025]. Available from: https://www.scb.se/hitta-statistik/statistik-efter-amne/befolkning-och-levnadsforhallanden/befolkningens-sammansattning-och-utveckling/befolkningsframskrivningar/pong/publikationer/sveriges-framtida-befolkning-2021-2070/
- SCB. Sveriges framtida befolkning 2022–2070. Statistiska centralbyrån (SCB); 2022. Demografiska rapporter 2022:4. [accessed Mar 25 2025]. Available from: https://www.scb.se/hitta-statistik/statistik-efter-amne/befolkning-och-levnadsforhallanden/befolkningens-sammansattning-och-utveckling/befolkningsframskrivningar/pong/publikationer/sveriges-framtida-befolkning-2022-2070/
- Diehl M, Smyer MA, Mehrotra CM. Optimizing aging: A call for a new narrative. Am Psychol. 2020;75(4):577-89. Available from: https://doi.org/10.1037/amp0000598
- Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752-62. Available from: https://doi.org/10.1016/S0140-6736(12)62167-9
- Maresova P, Javanmardi E, Barakovic S, Barakovic Husic J, Tomsone S, Krejcar O, et al. Consequences of chronic diseases and other limitations associated with old age - a scoping review. BMC Public Health. 2019;19(1):1431. Available from: https://doi.org/10.1186/s12889-019-7762-5
- Bloom DE, Chatterji S, Kowal P, Lloyd-Sherlock P, McKee M, Rechel B, et al. Macroeconomic implications of population ageing and selected policy responses. Lancet. 2015;385(9968):649-57. Available from: https://doi.org/10.1016/S0140-6736(14)61464-1
- WHO. World report on ageing and health. Luxembourg: World Health Organization (WHO); 2015. [accessed Mar 25 2025]. Available from: https://www.who.int/publications/i/item/9789241565042/
- Klimova B, Ivana S, Petra P, Zuzana T, and Kuca K. Older people and their attitude to the use of information and communication technologies – A review study with special focus on the Czech Republic (older people and their attitude to ICT). Educational Gerontology. 2016;42(5):361-9.
- Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel JP, et al. The World report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145-54. Available from: https://doi.org/10.1016/S0140-6736(15)00516-4
- Socialstyrelsen. Nationella riktlinjer 2024: Vård vid ohälsosamma levnadsvanor. Prioriteringsstöd till dig som beslutar om resurser för sjukdomsprevention och behandling. Stockholm: Socialstyrelsen; 2024. Nationella riktlinjer. [accessed Mar 26 2025]. Available from: https://www.socialstyrelsen.se/kunskapsstod-och-regler/regler-och-riktlinjer/nationella-riktlinjer/riktlinjer-och-utvarderingar/levnadsvanor/
- Bolin K. Preventionens betydelse för finansieringen av framtidens vård och omsorg. Stockholm: SNS Förlag; 2024.
- Monitor. Closing the NHS funding gap: how to get better value health care for patients. London: National health service (NHS); 2013. IRREP 22/13. [updated Oct 10 2013; accessed Mar 25 2025]. Available from: https://www.gov.uk/government/publications/closing-the-nhs-funding-gap-how-to-get-better-value-healthcare-for-patients
- WHO. Health promotion. World Health Organisation (WHO). [accessed Mar 25 2025]. Available from: https://www.who.int/health-topics/health-promotion#tab=tab_1
- WHO. Health promotion (Questions and answers). World Health Organisation (WHO). [accessed Mar 25 2025]. Available from: https://www.who.int/news-room/questions-and-answers/item/health-promotion
- Socialstyrelsens termbank. Socialstyrelsen. [accessed Mar 27 2025]. Available from: https://termbank.socialstyrelsen.se/
- SFS 2017:30. Hälso- och sjukvårdslag. Svensk författningssamling. Stockholm: Riksdagen. [accessed 27 Mar 2025]. Available from: https://www.riksdagen.se/sv/dokument-och-lagar/dokument/svensk-forfattningssamling/halso-och-sjukvardslag-201730_sfs-2017-30/#K13
- SFS 2025:400. Socialtjänstlag. Svensk författningssamling. Stockholm: Riksdagen. [accessed 4 Jun 2025]. Available from: https://www.riksdagen.se/sv/dokument-och-lagar/dokument/svensk-forfattningssamling/socialtjanstlag-2025400_sfs-2025-400/
- NPO levnadsvanor. Slutrapport avseende systematisk kunskapsgenomgång av den svenska modellen för Riktade hälsosamtal. Stockholm: Nationellt system för kunskapsstyrning. Hälso- och sjukvård. Sveriges regioner i samverkan.; 2022. [accessed Jun 11 2025]. Available from: https://kunskapsstyrningvard.se/kunskapsstyrningvard/kunskapsstod/publiceradekunskapsstod/levnadsvanor/svenskamodellenforriktadehalsosamtal.88067.html
- Region Skåne. Uppföljning av Riktade hälsosamtal för 70-åringar i Region Skåne. Region Skåne: Avdelningen för hälso- och sjukvårdsstyrning; 2024. [accessed Mar 27 2025]. Available from: https://vardgivare.skane.se/vardriktlinjer/levnadsvanor/riktade-halsosamtal-i-skane/#303229
- Välkommen till Fallprevention för vuxna som är 65 år och äldre! Eskilstuna: FoU i Sörmland,. [accessed Mar 28 2025]. Available from: https://www.fou.sormland.se/kunskapsportal/kunskapsstod-for-fallprevention/fallprevention-for-vuxna-65plus/
- Informationsmaterial för att förhindra fallolyckor. Stockholm: Socialstyrelsen; 2019. [updated May 15 2025; accessed Jun 11 2025]. Available from: https://www.socialstyrelsen.se/kunskapsstod-och-regler/omraden/aldre/stod-i-arbetet--vard-och-omsorg-for-aldre-personer--utifran-amnesomraden/fallolyckor/balanseramera/
- Davis R, Campbell R, Hildon Z, Hobbs L, Michie S. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev. 2015;9(3):323-44. Available from: https://doi.org/10.1080/17437199.2014.941722
- Michie S, West R, Campbell R, Brown J, Gainforth H. ABC of behaviour change theories. Great Britain: Silverback Publishing; 2014.
- Michie S, Atkins L, West R. The behaviour change wheel : a guide to designing interventions. [Sutton]: Silverback Publishing; 2014.
- Thomas J, Graziosi S, Brunton J, Ghouze Z, O’Driscoll P, Bond M, et al. EPPI-Reviewer: advanced software for systematic reviews, maps and evidence synthesis. EPPI Centre, UCL Social Research Institute: University College London; 2023.
- Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81-95. Available from: https://doi.org/10.1007/s12160-013-9486-6
- Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. Available from: https://doi.org/10.1186/1748-5908-6-42
- Borissov N, Haas Q, Minder B, Kopp-Heim D, von Gernler M, Janka H, et al. Reducing systematic review burden using Deduklick: a novel, automated, reliable, and explainable deduplication algorithm to foster medical research. Syst Rev. 2022;11(1):172. Available from: https://doi.org/10.1186/s13643-022-02045-9
- Norwegian Register for Scientific Journals, Series and Publishers. Bergen: The Norwegian Directorate for Higher Education and Skills. [updated March 6 2024; accessed Apr 23 2025]. Available from: https://kanalregister.hkdir.no/en/informasjonsartikler/search-in-the-register
- SBU. Bedömning av systematiska översikter (ROBIS). Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2020. Granskningsmall. [accessed Juni 11 2025]. Available from: https://www.sbu.se/sv/granskningsmallar/#granskningsmall
- Akinrolie O, Barclay R, Strachan S, Gupta A, Jasper US, Jumbo SU, et al. The effect of motivational interviewing on physical activity level among older adults: a systematic review and meta-analysis. Phys Occup Ther Geriatr. 2020;38(3):250-63. Available from: https://doi.org/10.1080/02703181.2020.1725217
- Alliston P, Jovkovic M, Khalid S, Fitzpatrick-Lewis D, Ali MU, Sherifali D. The effects of diabetes self-management programs on clinical and patient reported outcomes in older adults: a systematic review and meta-analysis. Front Clin Diabetes Healthc. 2024;5:1348104. Available from: https://doi.org/10.3389/fcdhc.2024.1348104
- Chastin S, Gardiner PA, Harvey JA, Leask CF, Jerez-Roig J, Rosenberg D, et al. Interventions for reducing sedentary behaviour in community-dwelling older adults. Cochrane Database Syst Rev. 2021;6(6):CD012784. Available from: https://doi.org/10.1002/14651858.CD012784.pub2
- Clark IN, Taylor NF, Peiris CL. Music listening interventions for physical activity: a systematic review and meta-analysis of randomised controlled trials. Disabil Rehabil. 2024;46(1):13-20. Available from: https://doi.org/10.1080/09638288.2022.2155715
- Creighton RM, Paradis KF, Blackburn NE, Tully MA. Group-Based Physical Activity Interventions Targeting Enjoyment in Older Adults: A Systematic Review. J Ageing Longev. 2022;2(2):113-29. Available from: https://doi.org/10.3390/jal2020011
- D’Amore C, Reid JC, Chan M, Fan S, Huang A, Louie J, et al. Interventions Including Smart Technology Compared With Face-to-face Physical Activity Interventions in Older Adults: Systematic Review and Meta-analysis. J Med Internet Res. 2022;24(10):e36134. Available from: https://doi.org/10.2196/36134
- E JY, Li T, McInally L, Thomson K, Shahani U, Gray L, et al. Environmental and behavioural interventions for reducing physical activity limitation and preventing falls in older people with visual impairment. Cochrane Database Syst Rev. 2020;9(9):CD009233. Available from: https://doi.org/10.1002/14651858.CD009233.pub3
- Geohagen O, Hamer L, Lowton A, Guerra S, Milton-Cole R, Ellery P, et al. The effectiveness of rehabilitation interventions including outdoor mobility on older adults’ physical activity, endurance, outdoor mobility and falls-related self-efficacy: systematic review and meta-analysis. Age Ageing. 2022;51(6):01. Available from: https://doi.org/10.1093/ageing/afac120
- Grande GD, Oliveira CB, Morelhao PK, Sherrington C, Tiedemann A, Pinto RZ, et al. Interventions Promoting Physical Activity Among Older Adults: A Systematic Review and Meta-Analysis. Gerontologist. 2020;60(8):583-99. Available from: https://doi.org/10.1093/geront/gnz167
- Jagroep W, Cramm JM, Denktas S, Nieboer AP. Behaviour change interventions to promote health and well-being among older migrants: A systematic review. PLoS One. 2022;17(6):e0269778. Available from: https://doi.org/10.1371/journal.pone.0269778
- Lenouvel E, Ullrich P, Siemens W, Dallmeier D, Denkinger M, Kienle G, et al. Cognitive behavioural therapy (CBT) with and without exercise to reduce fear of falling in older people living in the community. Cochrane Database Syst Rev. 2023;11(11):CD014666. Available from: https://doi.org/10.1002/14651858.CD014666.pub2
- Manifield J, Chaudhry Y, Singh SJ, Ward TJC, Whelan ME, Orme MW. Changes in physical activity, sedentary behaviour and sleep following pulmonary rehabilitation: a systematic review and network meta-analysis. Eur Respir Rev. 2024;33(172):30. Available from: https://doi.org/10.1183/16000617.0225-2023
- Nick JM, Roberts LR, Petersen AB. Effectiveness of telemonitoring on self-care behaviors among community-dwelling adults with heart failure: a quantitative systematic review. JBI Evid Synth. 2021;19(10):2659-94. Available from: https://doi.org/10.11124/JBIES-20-00329
- O’Hoski S, Chauvin S, Vrkljan B, Beauchamp MK. The Effect of Lifestyle Interventions on the International Classification of Functioning, Disability and Health Participation Domain in Older Adults: A Systematic Review and Meta-Analysis. Gerontologist. 2022;62(6):e304-e16. Available from: https://doi.org/10.1093/geront/gnab004
- Oliveira JS, Sherrington C, E RYZ, Franco MR, Tiedemann A. Effect of interventions using physical activity trackers on physical activity in people aged 60 years and over: a systematic review and meta-analysis. Br J Sports Med. 2020;54(20):1188-94. Available from: https://doi.org/10.1136/bjsports-2018-100324
- Sammut M, Fini N, Haracz K, Nilsson M, English C, Janssen H. Increasing time spent engaging in moderate-to-vigorous physical activity by community-dwelling adults following a transient ischemic attack or non-disabling stroke: a systematic review. Disabil Rehabil. 2022;44(3):337-52. Available from: https://doi.org/10.1080/09638288.2020.1768599
- Schrijver J, Lenferink A, Brusse-Keizer M, Zwerink M, van der Valk PD, van der Palen J, et al. Self-management interventions for people with chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2022;1(1):CD002990. Available from: https://doi.org/10.1002/14651858.CD002990.pub4
- Teggart K, Ganann R, Sihota D, Moore C, Keller H, Senson C, et al. Group-based nutrition interventions to promote healthy eating and mobility in community-dwelling older adults: a systematic review. Public Health Nutr. 2022;25(10):1-32. Available from: https://doi.org/10.1017/S136898002200115X
- Van Truong P, Wulan Apriliyasari R, Lin MY, Chiu HY, Tsai PS. Effects of self-management programs on blood pressure, self-efficacy, medication adherence and body mass index in older adults with hypertension: Meta-analysis of randomized controlled trials. Int J Nurs Pract. 2021;27(2):e12920. Available from: https://doi.org/10.1111/ijn.12920
- Werts SJ, Robles-Morales R, Bea JW, Thomson CA. Characterization and efficacy of lifestyle behavior change interventions among adult rural cancer survivors: a systematic review. J Cancer Surviv. 2023;19(1):253-69. Available from: https://doi.org/10.1007/s11764-023-01464-4
- Whitfield T, McConnell B, Renouf P, Mansour H, Zabihi S, Aguirre E, et al. The effect of remotely delivered lifestyle interventions on cognition in older adults without dementia: A systematic review and meta-analysis. Ageing Res Rev. 2021;72:101505. Available from: https://doi.org/10.1016/j.arr.2021.101505
- Wu S, Li G, Du L, Chen S, Zhang X, He Q. The effectiveness of wearable activity trackers for increasing physical activity and reducing sedentary time in older adults: A systematic review and meta-analysis. Digit Health. 2023;9:20552076231176705. Available from: https://doi.org/10.1177/20552076231176705
- Gilchrist H, Oliveira JS, Kwok WS, Sherrington C, Pinheiro MB, Bauman A, et al. Use of behavior change techniques in physical activity programs and services for older adults: findings from a rapid review. Ann Behav Med. 2024;58(3):216-26. Available from: https://doi.org/10.1093/abm/kaad074
- Hanrahan C, Broderick J, O’Connor TM, McVeigh JG. Behaviour change interventions for physical activity in adults with chronic obstructive pulmonary disease; A systematic review and meta-analysis. Respir Med Res. 2024;85:101068. Available from: https://doi.org/10.1016/j.resmer.2023.101068
- Otmanowski JA, Chase JD. Systematic Review and Meta-Analysis of Primary Care-Based Physical Activity Interventions Among Older Adults. J Aging Phys Act. 2022;30(5):842-56. Available from: https://doi.org/10.1123/japa.2021-0111
- Wu S, Li G, Shi B, Ge H, Chen S, Zhang X, et al. Comparative effectiveness of interventions on promoting physical activity in older adults: A systematic review and network meta-analysis. Digit Health. 2024;10:20552076241239182. Available from: https://doi.org/10.1177/20552076241239182
- Buyle M, Jung Y, Pavlou M, Gonzalez SC, Bamiou DE. The role of motivation factors in exergame interventions for fall prevention in older adults: A systematic review and meta-analysis. Front Neurol. 2022;13:903673. Available from: https://doi.org/10.3389/fneur.2022.903673
- Ong MF, Soh KL, Saimon R, Wai MW, Mortell M, Soh KG. Fall prevention education to reduce fall risk among community-dwelling older persons: A systematic review. J Nurs Manag. 2021;29(8):2674-88. Available from: https://doi.org/10.1111/jonm.13434
- Teng B, Gomersall SR, Hatton A, Brauer SG. Combined group and home exercise programmes in community-dwelling falls-risk older adults: Systematic review and meta-analysis. Physiother Res Int. 2020;25(3):e1839. Available from: https://doi.org/10.1002/pri.1839
- Chase JD, Otmanowski J, Rowland S, Cooper PS. A systematic review and meta-analysis of interventions to reduce sedentary behavior among older adults. Transl Behav Med. 2020;10(5):1078-85. Available from: https://doi.org/10.1093/tbm/ibz189
- Chau RCW, Thu KM, Chaurasia A, Hsung RTC, Lam WY. A Systematic Review of the Use of mHealth in Oral Health Education among Older Adults. Dent J (Basel). 2023;11(8):08. Available from: https://doi.org/10.3390/dj11080189
- Hawke LJ, Shields N, Dowsey MM, Choong PFM, Taylor NF. Effectiveness of behavioural interventions on physical activity levels after hip or knee joint replacement: a systematic review. Disabil Rehabil. 2020;42(25):3573-80. Available from: https://doi.org/10.1080/09638288.2019.1603328
- Seah SJ, Zheng H, Lim RBT. Efficacy of community-based self-care interventions to improve biophysical, psychosocial or behavioural outcomes among community-dwelling older adults with type 2 diabetes: A systematic review and meta-analysis. Diabetes Res Clin Pract. 2020;169:108411. Available from: https://doi.org/10.1016/j.diabres.2020.108411
- Purser GL, Lemieux CM. Brief alcohol interventions with older adults: a systematic review of literature. J Soc Work Pract Addict. 2021;22(2):120-36. Available from: https://doi.org/10.1080/1533256x.2021.1935146
- Bevilacqua R, Casaccia S, Cortellessa G, Astell A, Lattanzio F, Corsonello A, et al. Coaching Through Technology: A Systematic Review into Efficacy and Effectiveness for the Ageing Population. Int J Environ Res Public Health. 2020;17(16):15. Available from: https://doi.org/10.3390/ijerph17165930
- Barras L, Neuhaus M, Cyarto EV, Reid N. Effectiveness of Peer-Led Wellbeing Interventions in Retirement Living: A Systematic Review. Int J Environ Res Public Health. 2021;18(21). Available from: https://doi.org/10.3390/ijerph182111557
- Bashirian S, Khoshravesh S, Ayubi E, Karimi-Shahanjarini A, Shirahmadi S, Solaymani PF. The impact of health education interventions on oral health promotion among older people: a systematic review. BMC Geriatr. 2023;23(1):548. Available from: https://doi.org/10.1186/s12877-023-04259-5
- Papadimitriou A, Perry M. Systematic Review of the Effects of Cognitive and Behavioural Interventions on Fall-Related Psychological Concerns in Older Adults. J Aging Phys Act. 2020;28(1):155-68. Available from: https://doi.org/10.1123/japa.2017-0408
- TIDierR (Template for Intervention Description and Replication). Institute for Evidence-Based Healthcare Bond University. [accessed Juni 16 2025]. Available from: https://tidierguide.org/#

 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services
 Share on Facebook
Share on Facebook
 Share on LinkedIn
Share on LinkedIn
 Share via Email
Share via Email