This publication was published more than 5 years ago. The state of knowledge may have changed.
Myalgic encephalomyelitis and Chronic Fatigue Syndrome (ME/CFS)
A systematic review
Aim
The aim of this report was to investigate the available body of evidence for the treatment and prognosis of ME/CFS as well as a review of the health care experiences of patients.
Background
Myalgic encephalomyelitis, also called Chronic Fatigue syndrome (ME/CFS), was first described 70 years ago. The disorder often is preceded by an infection but the pathology and mechanisms behind ME/CFS are still unknown. People with ME/CFS can suffer from a broad spectrum of symptoms, e.g. prolonged fatigue, pain and post-exertional malaise (PEM). Individuals with ME/CFS have decreased activity levels and can have difficulty handling their everyday day duties, work, or studies and maintaining social relationships. For some, the symptoms can be so severe that they are home- or bedbound.
There are no bio markers for ME/CFS that can be used for diagnosis. The criteria for diagnosis have therefore developed over the years and are consensus-based sets of core symptoms. All the criteria include newly-onset severe and persistent fatigue and stipulate that core symptoms must have persisted for at least 6 months. The newer Canadian Consensus Criteria differs from previous criteria in that PEM lasting at least 24 hours after physical or mental exertion is required for a diagnosis. By applying the Canadian Consensus Criteria, the prevalence of ME/CFS is estimated to be about 0,1% of the population.
Differentiating between ME/CFS and other diseases with long lasting fatigue, e.g. stress related exhaustion disorder, can be difficult. Studies show that half of patients referred to specialist clinics for suspicion of ME/CFS were shown to have other diseases after closer examination, mostly sleep or psychiatric disorders.
There is no curative treatment for ME/CFS. Health care therefore aims at relieving symptoms and supporting the patients in the management of their everyday lives.
Content of the report
This report is made up of four systematic reviews, conducted according to international guidelines. The first systematic review focuses on treatments and their effects on fatigue and PEM for persons with ME/CFS diagnosed with the Canadian Consensus Criteria. Treatments that aimed at relieving other symptoms, e.g. sleep problems or pain, or psychological therapies aimed at helping patients manage their disease were not included. Included studies were controlled clinical trials, with or without randomisation.
The second systematic review assesses prognosis for recovery and return to work, while the third investigates whether there are any prognostic factors for improvement and return to work. In the fourth systematic review, we explore how patients experience their health care by reviewing studies that used qualitative methods, such as interviews, to address this question.
The report only includes studies on adults.
Main results
A major finding was that the effects of treatments for patients diagnosed with the Canadian Consensus Criteria on fatigue or PEM cannot be estimated. Most studies used older criteria, mainly the Fukuda criteria, meaning there is a risk that the participants in the studies had other conditions, such as stress related exhaustion disorder or depression. Whether these results are valid for persons diagnosed according to the Canadian Consensus Criteria is therefore unclear.
A small number of studies, most investigating pharmaceutical treatments, used the Canadian Consensus Criteria. None of these studies reported that the drug reduced fatigue.
The prognostic studies identified applied older criteria. Two studies conducted in Scandinavian countries reported that a substantial proportion of the participants had not recovered at follow-up, around 10 years after symptom onset. One English and one Norwegian study found that many patients who had been diagnosed in specialist clinics after several years of disease and unemployment, had not yet returned to work or study at follow-ups conducted many years later. Prognostic factors for recovery or return to work could not be evaluated as there were few studies, which were small and had substantial methodological limitations.
The qualitative studies mostly described patient experiences in primary care. Many perceived that getting a diagnosis was a milestone and that individually tailored support was crucial for them to move on with their lives. They experienced the process of obtaining a diagnosis as burdensome and frustrating and felt that they were met with ignorance and lack of understanding.
Discussion
This report shows that there are many scientific evidence gaps regarding ME/CFS. Many gaps, such as methods for diagnosis and efficacy of curative or disease modifying treatments, are related to the lack of understanding of the aetiology behind ME/CFS.
This report also indicates that a thorough diagnostic work-up is crucial. Multidisciplinary specialist competences are necessary to reliably exclude other disorders.
Finally, the absence of evidence for effect of ME/CFS treatments does not mean that the treatments lack effect, but rather indicates that research is needed to clarify the effects of current treatments for people diagnosed with ME/CFS according to the Canadian Consensus Criteria. Meanwhile, it is important to support people with ME/CFS so they can attain the best quality of life, levels of function and participation in society as is possible. Since ME/CFS is relatively uncommon compared to other similar disorders, e.g. stress related exhaustion disorder or chronic pain, specialist clinics for ME/CFS would probably be advantageous, as they would be most likely to be able to closely follow the research and quickly implement new developments into clinical practice.
The full report in Swedish
The full resport in Swedish "Myalgisk encefalomyelit och kroniskt trötthetssyndrom (ME/CFS)"
Project group
Experts
- Per Julin, MD, PhD, Karolinska Institutet, Stockholm, and the ME/CFS-clinic, Stora Sköndal
- Per Lytsy, MD, Assistant Professor, SBU
- Marie Åsberg, Professor, Karolinska Institutet and Danderyd Hospital, Stockholm (advisory role in assessing differential diagnoses)
SBU
- Agneta Pettersson (Project Manager)
- Susanne Gustafsson (Information Specialist)
- Caroline Jungner (Project Administrator)
- Lina Leander (Assistant Project Manager)
- Hanna Olofsson (Information Specialist)
Flow charts
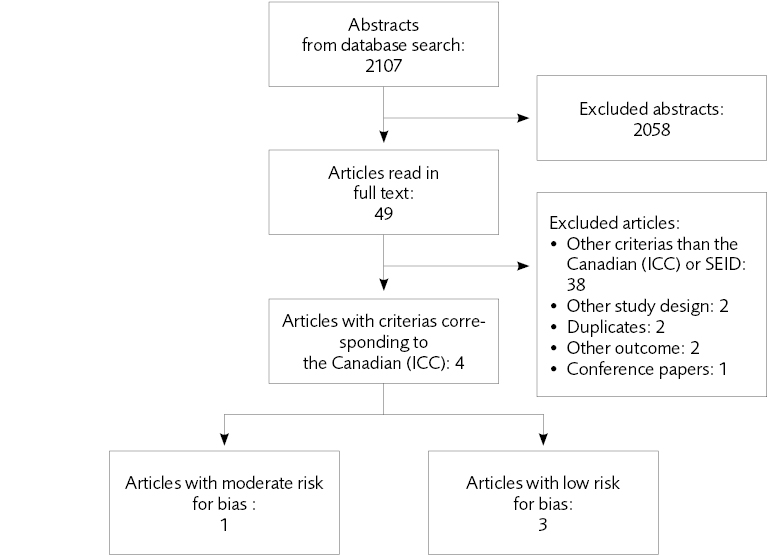
Figure 4.1 Flow chart of the literature review regarding the effect of treatments
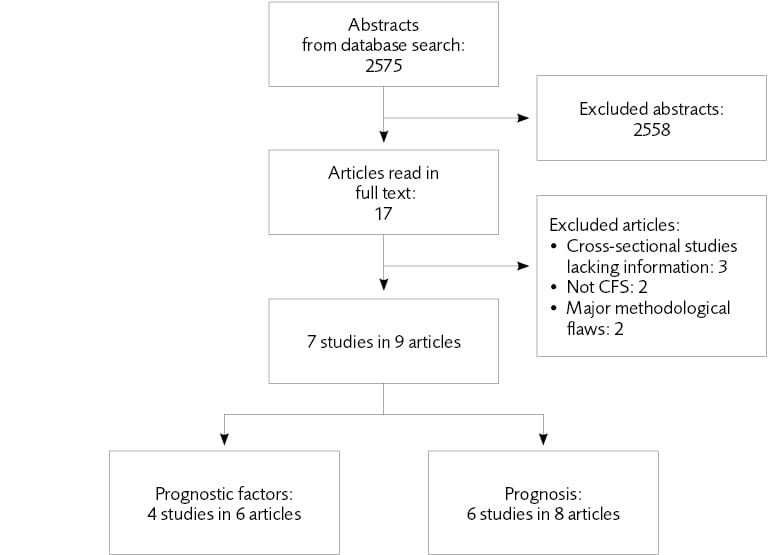
Figure 5.1 Flow chart of the literature review regarding prognosis and prognostic factors
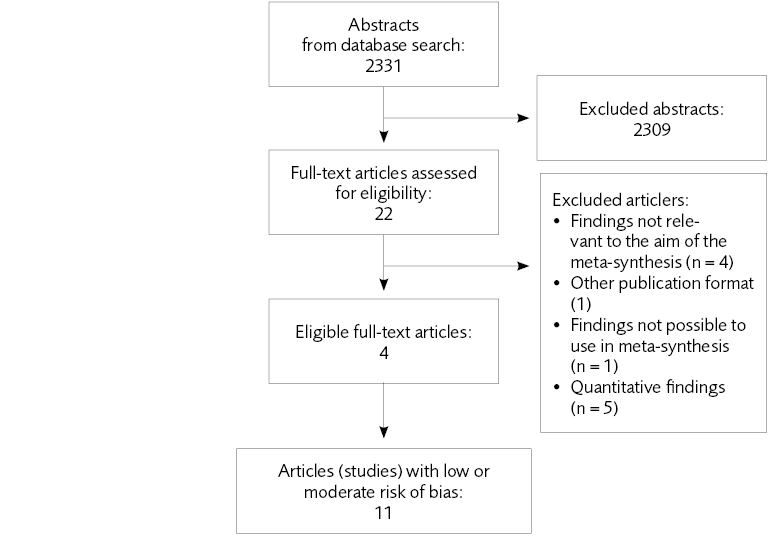
Figure 6.1 Flow chart of the literature review regarding experience and perceptions of care
Reference list of full report
- Acheson ED. Benign myalgic encephalomyelitis. Lancet 1957;272:834-5.
- Galpine JF, Brady C. Benign myalgicencephalomyelitis. Lancet 1957;272:757-8.
- Holmes GP, Kaplan JE, Gantz NM,Komaroff AL, Schonberger LB, StrausSE et al. Chronic Fatigue Syndrome: aworking case definition. Ann Intern Med1988:387-9.
- Committee on the Diagnostic Criteriafor Myalgic Encephalomyelitis/ChronicFatigue Syndrome; Board on the Healthof Select Populations; Institute of Medicine. Beyond myalgic encephalomyelitis/chronic fatigue syndrome: Redefining anillness. Washington, DC: The NationalAcademies; 2015.
- White P. What causes prolonged fatigueafter infectious mononucleosis: and doesit tell us anything about chronic fatiguesyndrome? J Infect Dis 2007;196:4-5.
- Borsini A HN, Mondelli V, Chalder T,Pariante CM. Childhood stressors inthe development of fatigue syndromes:a review of the past 20 years of research.Psychol Med 2014;44:1809-23.
- Leone SS, Wessely S, Huibers MJ,Knottnerus JA, Kant I. Two sides of thesame coin? On the history and phenomenology of chronic fatigue and burnout.Psychol Health 2011;26:449-64.
- Stormorken E JL, Kirkevold M.Factors impacting the illness trajectoryof post-infectious fatigue syndrome: aqualitative study of adults’ experiences.BMC Public Health 2017;17:952.
- Engel G. The need for a new medicalmodel: A challenge for biomedicine.Science 1977;196:129-36.
- Geraghty KJ, Blease C. Myalgic encephalomyelitis/chronic fatigue syndrome andthe biopsychosocial model: a review ofpatient harm and distress in the medicalencounter. Disabil Rehabil 2018:1-10.
- Blomberg J, Gottfries CG, Elfaitouri A,Rizwan M, Rosen A. Infection elicitedautoimmunity and myalgic encephalomyelitis/chronic fatigue syndrome:An explanatory model. Front Immunol2018;9:229.
- Schutzer SE, Angel TE, Liu T,Schepmoes AA, Clauss TR, Adkins JNet al. Distinct cerebrospinal fluid proteomes differentiate post-treatment lyme disease from chronic fatigue syndrome. In: PLoS One; 2011.
- Moneghetti KJ, Skhiri M, Contrepois K, Kobayashi Y, Maecker H, Davis M, et al. Value of circulating cytokine profiling during submaximal exercise testing in myalgic encephalomyelitis/chronic fatigue syndrome. Sci Rep 2018;8:2779.
- Fluge O, Mella O, Bruland O, Risa K, Dyrstad SE, Alme K, et al. Metabolic profiling indicates impaired pyruvate dehydrogenase function in myalgic encephalopathy/chronic fatigue syndrome. JCI Insight 2016;1:e89376.
- Siessmeier T NW, Hardt J, Schreckenberger M, Egle UT, Bartenstein P. Observer independent analysis of cerebral glucose metabolism in patients with chronic fatigue syndrome. J Neurol Neurosurg Psychiatry 2003;74:922-8.
- Nakatomi Y MK, Ishii A, Wada Y, Tanaka M, Tazawa S, Onoe K et al. Neuroinflammation in patients with chronic fatigue syndrome/myalgic encephalomyelitis: An ¹¹C-(R)-PK11195 PET Study. J Nucl Med 2014;55:945-50.
- Elfaitouri A HB, Bölin-Wiener A, Wang Y, Gottfries CG, Zachrisson O, Pipkorn R et al. Epitopes of microbial and human heat shock protein 60 and their recognition in myalgic encephalomyelitis. PLoS One 2013;8.
- Loebel M GP, Heidecke H, Bauer S, Hanitsch LG, Wittke K, et al. Antibodies to beta adrener-gic and muscarinic cholinergic receptors in patients with Chronic Fatigue Syndrome. Brain Behav Immun 2016;52:32-9.
- Scheibenbogen C LM, Freitag H, Krueger A, Bauer S, Antelmann M, et al. Immunoadsorption to remove ß2 adrenergic receptor antibodies in Chronic Fatigue Syndrome CFS/ME. PLoS ONE 2018;13.
- Stevens S, Snell C, Stevens J, Keller B, VanNess JM. Cardiopulmonary exercise test methodology for assessing exertion intolerance in myalgic encephalomyelitis/chronic fatigue syndrome. Front Pediatr 2018;6:242.
- Hodges LD, Nielsen T, Baken D. Physiological measures in participants with chronic fatigue syndrome, multiple sclerosis and healthy controls following repeated exercise: a pilot study. Clin Physiol Funct Imaging 2018;38:639-44.
- National Institute of Health. NIH ME/CFS Clinical Study. https://www.nih.gov/mecfs/nih-me-cfs-clinical-study; 2018.
- National Institute of Health. NIH announces centers for myalgic encephalomyelitis/chronic fatigue syndrome research. nih-announces-centers-myalgic-encephalomyelitis-chronic-fatigue-syndrome-research; 2018.
- Hardcastle SL, Brenu EW, Johnston S, Staines D, Marshall-Gradisnik S. Severity Scales for Use in Primary Health Care to Assess Chronic Fatigue Syndrome/Myalgic Encephalomyelitis. Health Care Women Int 2016;37:671-86.
- Castro-Marrero J, Faro M, Aliste L, Sáez-Francàs N, Calvo N, Martínez-Martínez A, et al. Comorbidity in chronic fatigue syndrome/myalgic encephalomyelitis: A nationwide population-based cohort study. Psychosomatics 2017;58:533-43.
- Nørregaard J BP, Prescott E, Jacobsen S, Danneskiold-Samsøe B. A four-year follow-up study in fibromyalgia. Relationship to chronic fatigue syndrome. Scand J Rheumatol 1993;22:35-8.
- Donnachie E, Schneider A, Mehring M, Enck P. Incidence of irritable bowel syndrome and chronic fatigue following GI infection: a population-level study using routinely collected claims data. Gut 2018;67:1078-86.
- Persson R WK, Hanevik K, Eide GE, Langeland N, Rortveit G. . The relationship between irritable bowel syndrome, functional dyspepsia, chronic fatigue and overactive bladder syndrome: a controlled study 6 years after acute gastrointestinal infection. BMC Gastroenterol 2015;10:66.
- Maes M LJ, Geffard M, Berk M. vidence for the existence of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) with and without abdominal discomfort (irritable bowel) syndrome. Neuro Endocrinol Lett 2014;35:445-53.
- Mariman A, Delesie L, Tobback E, Hanoulle I, Sermijn E, Vermeir P, et al. Undiagnosed and comorbid disorders in patients with presumed chronic fatigue syndrome. J Psychosom Res 2013;75:491-6.
- Carruthers BM, van de Sande MI, De Meirleir KL, Klimas NG, Broderick G, Mitchell T, et al. Myalgic encephalomyelitis: International Consensus Criteria. J Intern Med 2011;270:327-38.
- Social Security Administration. Providing medical evidence for individuals with myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). USA; 2018.
- Brurberg KG, Fonhus MS, Larun L, Flottorp S, Malterud K. Case definitions for chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME): a systematic review. BMJ Open 2014;4:e003973.
- Fukuda K, Straus SE, Hickie I, Sharpe MC, Dobbins JG, Komaroff A. The chronic fatigue syndrome: a comprehensive approach to its definition and study. International Chronic Fatigue Syndrome Study Group. Ann Intern Med 1994;121:953-9.
- Carruthers BM JA, de Meirleir KL, Peterson DL, Klimas NG, Lerner AM, Bested AC, et al. Myalgic encephalomyelitis/chronic fatigue syndrome: Clinical working case definition, diagnostic and treatment protocols. J Chronic Fatigue Syndrome 2003;11.
- Jason LA, Sunnquist M, Brown A, Newton JL, Strand EB, Vernon SD. Chronic Fatigue Syndrome versus Systemic Exertion Intolerance Disease. Fatigue 2015;3:127-41.
- Brown AA, Jason LA. Validating a measure of myalgic encephalomyelitis/chronic fatigue syndrome symptomatology. Fatigue 2014;2:132-52.
- Nacul LC, Lacerda EM, Pheby D, Campion P, Molokhia M, Fayyaz S, et al. Prevalence of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) in three regions of England: a repeated cross-sectional study in primary care. BMC Med 2011;9:91.
- Johnston SC, Staines DR, Marshall-Gradisnik SM. Epidemiological characteristics of chronic fatigue syndrome/myalgic encephalomyelitis in Australian patients. Clin Epidemiol 2016;8:97-107.
- Newton JL MH, Scott A, Hoad A, Spickett G. The Newcastle NHS Chronic Fatigue Syndrome Service: not all fatigue is the same. J R Coll Physicians Edinb 2010;40:304-7.
- Devasahayam A, Lawn T, Murphy M, White PD. Alternative diagnoses to chronic fatigue syndrome in referrals to a specialist service: service evaluation survey. JRSM Short Rep 2012;3:4.
- Socialstyrelsen. Utmattningssyndrom – Stressrelaterad psykisk ohälsa; 2003.
- Grossi G, Perski A, Osika W, Savic I. Stress-related exhaustion disorder--clinical manifestation of burnout? A review of assessment methods, sleep impairments, cognitive disturbances, and neuro-biological and physiological changes in clinical burnout. Scand J Psychol 2015;56:626-36.
- Besèr A SK, Wahlberg K, Peterson U, Nygren A, Asberg M. Construction and evaluation of a self rating scale for stress-induced exhaustion disorder, the Karolinska Exhaustion Disorder Scale. Scand J Psychol 2014;55:72-82.
- Wallensten J, Asberg M, Nygren A, Szulkin R, Wallen H, Mobarrez F, et al. Possible Biomarkers of Chronic Stress Induced Exhaustion – A Longitudinal Study. PLoS One 2016;11:e0153924.
- Wolfe F, Smythe HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum 1990;33:160-72.
- Wolfe F, Clauw DJ, Fitzcharles MA, Goldenberg DL, Hauser W, Katz RL, et al. 2016 Revisions to the 2010/2011 fibromyalgia diagnostic criteria. Semin Arthritis Rheum 2016;46:319-29.
- Sharpe MC, Archard LC, Banatvala JE, Borysiewicz LK, Clare AW, David A, et al. A report--chronic fatigue syndrome: guidelines for research. J R Soc Med 1991;84:118-21.
- Furberg H, Olarte M, Afari N, Goldberg J, Buchwald D, Sullivan PF. The prevalence of self-reported chronic fatigue in a U.S. twin registry. J Psychosom Res 2005;59:283-90.
- Rusu C, Gee ME, Lagace C, Parlor M. Chronic fatigue syndrome and fibromyalgia in Canada: prevalence and associations with six health status indicators. Health Promot Chronic Dis Prev Can 2015;35:3-11.
- Socialstyrelsen. Internationell statistisk klassifikation av sjukdomar och relaterade hälsoproblem. Systematisk förteckning Svensk version 2016. Del 1 (3). Svensk version av International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10). http://apps.who.int/iris/bitstream/handle/10665/246208/9789175553801-V1-part1-swe.pdf;jsessionid=0AE99E57D5CFA82F4BDE0AFD017A2440?sequence=11; 2016.
- Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 2010;8:336-41.
- Tong A, Flemming K, McInnes E, Oliver S, Craig J. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012;12:181.
- Statens beredning för medicinsk och social utvärdering (SBU). SBU:s handbok: Utvärdering av metoder i hälso-och sjukvården och insatser i socialtjänsten. Stockholm; 2017.
- Sterne JA, Hernan MA, Reeves BC, Savovic J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8:45.
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 2011;64:383-94.
- Lewin S GC, Munthe-Kaas H, Carlsen B, Colvin CJ, Gulmezoglu M, Noves J, et al. Using qualitative evidence in decision making for health and social interventions: an approach to assess confidence in findings from qualitative evidence syntheses. PLoS Med 2015;12.
- Munthe-Kaas H, Bohren MA, Glenton C, Lewin S, Noyes J, Tuncalp O, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings-paper 3: how to assess methodological limitations. Implement Sci 2018;13:9.
- Colvin CJ, Garside R, Wainwright M, Munthe-Kaas H, Glenton C, Bohren MA, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings-paper 4: how to assess coherence. Implement Sci 2018;13:13.
- Noyes J, Booth A, Lewin S, Carlsen B, Glenton C, Colvin CJ, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings-paper 6: how to assess relevance of the data. Implement Sci 2018;13:4.
- Glenton C, Carlsen B, Lewin S, Munthe-Kaas H, Colvin CJ, Tuncalp O, et al. Applying GRADE-CERQual to qualitative evidence synthesis findings-paper 5: how to assess adequacy of data. Implement Sci 2018;13:14.
- Montoya JG, Kogelnik AM, Bhangoo M, Lunn MR, Flamand L, Merrihew LE, et al. Randomized clinical trial to evaluate the efficacy and safety of valganciclovir in a subset of patients with chronic fatigue syndrome. J Med Virol 2013;85:2101-9.
- Nilsson MKL, Zachrisson O, Gottfries CG, Matousek M, Peilot B, Forsmark S, et al. A randomised controlled trial of the monoaminergic stabiliser (−)-OSU6162 in treatment of myalgic encephalomyelitis/chronic fatigue syndrome. Acta Neuropsychiatrica 2017:1-10.
- Pinxsterhuis I, Sandvik L, Strand EB, Bautz-Holter E, Sveen U. Effectiveness of a group-based self-management program for people with chronic fatigue syndrome: a randomized controlled trial. Clin Rehabil 2017;31:93-103.
- Witham MD, Adams F, McSwiggan S, Kennedy G, Kabir G, Belch JJF, et al. Effect of intermittent vitamin D3 on vascular function and symptoms in chronic fatigue syndrome--a randomised controlled trial. Nutr Metab Cardiovasc Dis 2015;25:287-94.
- Friedberg F, Adamowicz J, Caikauskaite I, Seva V, Napoli A. Efficacy of two delivery modes of behavioral self-management in severe chronic fatigue syndrome. Fatigue 2016;4:158-74.
- Hall DL, Lattie EG, Milrad SF, Czaja S, Fletcher MA, Klimas N, et al. Telephone-administered versus live group cognitive behavioral stress management for adults with CFS. J Psychosom Res 2017;93:41-7.
- Nunez M F-SJ, Nunez E, Fernandez-Huerta JM, Godas-Sieso T, Gomez-Gil E. Health-related quality of life in patients with chronic fatigue syndrome: group cognitive behavioural therapy and graded exercise versus usual treatment. A randomised controlled trial with 1 year of follow-up. Clin Rheumatol 2011;30:381-9.
- Clark LV, Pesola F, Thomas JM, Vergara-Williamson M, Beynon M, White PD. Guided graded exercise self-help plus specialist medical care versus specialist medical care alone for chronic fatigue syndrome (GETSET): a pragmatic randomised controlled trial. Lancet (London, England) 2017;390:363-73.
- Fernie BA, Murphy G, Wells A, Nikcevic AV, Spada MM. Treatment outcome and metacognitive change in CBT and GET for chronic fatigue syndrome. Behav Cogn Psychother 2016;44:397-409.
- Kos D, van Eupen I, Meirte J, Van Cauwenbergh D, Moorkens G, Meeus M, et al. Activity pacing self-management in chronic fatigue syndrome: A randomized controlled trial. Am J Occup Ther 2015;69:6905290020.
- Marques MM, de Gucht V, Leal I, Maes S. Efficacy of a randomized controlled self-regulation based physical activity intervention for chronic fatigue: Mediation effects of physical activity progress and self-regulation skills. J Psychosom Res 2017;94:24-31.
- Moss-Morris R, Sharon C, Tobin R, Baldi JC. A randomized controlled graded exercise trial for chronic fatigue syndrome: outcomes and mechanisms of change. J Health Psychol 2005;10:245-59.
- Wallman KE, Morton AR, Goodman C, Grove R, Guilfoyle AM. Randomised controlled trial of graded exercise in chronic fatigue syndrome. Med J Aust 2004;180:444-8.
- White P, Chalder T, Sharpe M. The PACE trial: Results of a large trial of nonpharmacological treatments. J Psychosom Res 2011;70:622.
- Burgess M, Andiappan M, Chalder T. Cognitive behaviour therapy for chronic fatigue syndrome in adults: face to face versus telephone treatment: a randomized controlled trial. Behav Cogn Psychother 2012;40:175-91.
- Friedberg F, Napoli A, Coronel J, Adamowicz J, Seva V, Caikauskaite I, et al. Chronic fatigue self-manage-ment in primary care: a randomized trial. Psychosom Med 2013;75:650-7.
- Hlavaty LE, Brown MM, Jason LA. The effect of homework compliance on treatment outcomes for participants with myalgic encephalomyelitis/chronic fatigue syndrome. Rehabil Psychol 2011;56:212-8.
- Janse A, Worm-Smeitink M, Bleijenberg G, Donders R, Knoop H. Efficacy of web-based cognitive-behavioural therapy for chronic fatigue syndrome: randomised controlled trial. Br J Psychiatry 2018;212:112-8.
- Knoop H, Van Der Meer JWM, Bleijenberg G. Guided self-instructions for people with chronic fatigue syndrome: Randomised controlled trial. Br J Psychiatry 2008;193:340-1.
- O’Dowd H, Gladwell P, Rogers CA, Hollinghurst S, Gregory A. Cognitive behavioural therapy in chronic fatigue syndrome: A ramdomised controlled trial of an outpatient group programme. Health Technology Assessment 2006;10:iii-51.
- Rimes K, Wingrove J. Mindfulness-based cognitive therapy for people with chronic fatigue syndrome still experiencing excessive fatigue after cognitive behaviour therapy: a pilot randomized study. In: Clin Psychol Psychother 2013;20:107-17.
- Wearden AJ, Dowrick C, Chew-Graham C, Bentall RP, Morriss RK, Peters S, et al. Nurse led, home based self help treatment for patients in primary care with chronic fatigue syndrome: Randomised controlled trial. BMJ (Online) 2010;340:959.
- Wiborg JF, van Bussel J, van Dijk A, Bleijenberg G, Knoop H. Randomised controlled trial of cognitive behaviour therapy delivered in groups of patients with chronic fatigue syndrome. Psychother Psychosom 2015;84:368-76.
- Windthorst P, Mazurak N, Kuske M, Hipp A, Giel KE, Enck P, et al. Heart rate variability biofeedback therapy and graded exercise training in management of chronic fatigue syndrome: An exploratory pilot study. J Psychosom Res 2017;93:6-13.
- Vos-Vromans DCWM, Smeets RJEM, Huijnen IPJ, Köke AJA, Hitters WMGC, Rijnders LJM, et al. Multidisciplinary rehabilitation treatment versus cognitive behavioural therapy for patients with chronic fatigue syndrome: A randomized controlled trial. J Intern Med 2016;279:268-82.
- Tummers M, Knoop H, Bleijenberg G. Effectiveness of stepped care for chronic fatigue syndrome: a randomized noninferiority trial. J Consult Clin Psychol 2010;78:724-31.
- Arnold LM, Blom TJ, Welge JA, Mariutto E, Heller A. A randomized, placebo-controlled, double-blinded trial of duloxetine in the treatment of general fatigue in patients with chronic fatigue syndrome. Psychosomatics 2015;56:242-53.
- Fluge O, Bruland O, Risa K, Storstein A, Kristoffersen EK, Sapkota D, et al. Benefit from B-lymphocyte depletion using the anti-CD20 antibody rituximab in chronic fatigue syndrome. A double-blind and placebo-controlled study. PloS one 2011;6:e26358.
- Montoya JG, Anderson JN, Adolphs DL, Bateman L, Klimas N, Levine SM, et al. KPAX002 as a treatment for myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS): A prospective, randomized trial. Int J Clin Exp Med 2018;11:2890-900.
- Pardini M, Guida S, Primavera A, Krueger F, Cocito L, Gialloreti LE. Amisulpride vs. fluoxetine treatment of Chronic Fatigue Syndrome: A pilot study. Eur Neuropsychopharmacol 2011;21:282-6.
- Roerink ME, Bredie SJH, Heijnen M, Dinarello CA, Knoop H, Van der Meer JWM. Cytokine Inhibition in Patients With Chronic Fatigue Syndrome: A Randomized Trial. Ann Intern Med 2017;166:557-64.
- Strayer DR, Carter WA, Stouch BC, Stevens SR, Bateman L, Cimoch PJ, et al. A double-blind, placebo-controlled, randomized, clinical trial of the TLR-3 agonist rintatolimod in severe cases of chronic fatigue syndrome. PloS one 2012;7:e31334.
- The GK, Bleijenberg G, Buitelaar JK, van der Meer JW. The effect of ondansetron, a 5-HT3 receptor antagonist, in chronic fatigue syndrome: a randomized controlled trial. J Clin Psychiatry 2010;71:528-33.
- Castro-Marrero J, Cordero MD, Segundo MJ, Sáez-Francàs N, Calvo N, Román-Malo L, et al. Does oral coenzyme Q10 plus NADH supplementation improve fatigue and biochemical parameters in chronic fatigue syndrome? Antioxid Redox Signal 2015;22:679-85.
- Fukuda S, Nojima J, Kajimoto O, Yamaguti K, Nakatomi Y, Kuratsune H, et al. Ubiquinol-10 supplementation improves autonomic nervous function and cognitive function in chronic fatigue syndrome. BioFactors 2016;42:431-40.
- Ostojic SM, Stojanovic M, Drid P, Hoffman JR, Sekulic D, Zenic N. Supplementation with guanidinoacetic acid in women with Chronic Fatigue Syndrome. Nutrients 2016;8:72.
- Chan JSM, Ho RTH, Wang C-W, Yuen LP, Sham JST, Chan CLW. Effects of qigong exercise on fatigue, anxiety, and depressive symptoms of patients with chronic fatigue syndrome-like illness: a randomized controlled trial. Evid Based Complement Alternat Med 2013;2013:485341.
- Kim HG, Cho JH, Yoo SR, Lee JS, Han JM, Lee NH, et al. Antifatigue Effects of Panax ginseng C.A. Meyer: A randomised, double-blind, placebo-controlled Trial. PLoS ONE 2013;8.
- Kim J-E, Seo B-K, Choi J-B, Kim H-J, Kim T-H, Lee M-H, et al. Acupuncture for chronic fatigue syndrome and idiopathic chronic fatigue: a multicenter, nonblinded, randomized controlled trial. Trials 2015;16:314.
- Li D, Li Z, Dai Z. Selective serotonin reuptake inhibitor combined with dengzhanshengmai capsule improves the fatigue symptoms: a 12-week open-label pilot study. Int J Clin Exp Med 2015;8:11811-7.
- Ng SM, Yiu YM. Acupuncture for chronic fatigue syndrome: a randomized, sham-controlled trial with single-blinded design. Altern Ther Health Med 2013;19:21-6.
- Jason LA, Roesner N, Porter N, Parenti B, Mortensen J, Till L. Provision of social support to individuals with chronic fatigue syndrome. J Clin Psychol 2010;66:249-58.
- Huibers MJH, Beurskens AJHM, Van Schayck CP, Bazelmans E, Metsemakers JFM, Knottnerus JA, et al. Efficacy of cognitive-behavioural therapy by general practitioners for unexplained fatigue among employees: Randomised controlled trial. Br J Psychiatry 2004;184:240-6.
- Huibers MJH, Bultmann U, Kasl SV, Kant I, van Amelsvoort LGPM, van Schayck CP, et al. Predicting the two-year course of unexplained fatigue and the onset of long-term sickness absence in fatigued employees: results from the Maastricht Cohort Study. J Occup Environ Med 2004;46:1041-7.
- Collin SM, Crawley E, May MT, Sterne JAC, Hollingworth W, Database UCMNO. The impact of CFS/ME on employment and productivity in the UK: a cross-sectional study based on the CFS/ME national outcomes database. BMC Health Serv Res 2011;11:217.
- Tritt K, Nickel M, Mitterlehner F, Nickel C, Forthuber P, Leiberich P, et al. Chronic fatigue and indicators of long-term employment disability in psychosomatic inpatients. Wien Klin Wochenschr 2004;116:182-9.
- Roche R TR. Coping and occupational participation in chronic fatigue syndrome. OTJR (Thorofare N J) 2005;25.
- Houlton A, Christie MM, Smith B, Gardiner E. Long-term follow-up of multi-disciplinary outpatient treatment for chronic fatigue syndrome/myalgic encephalopathy. Fatigue 2015;3:47-58.
- Meeus M, Nijs J, Van Mol E, Truijen S, De Meirleir K. Role of psychological aspects in both chronic pain and in daily functioning in chronic fatigue syndrome: a prospective longitudinal study. Clin Rheumatol 2012;31:921-9.
- Flo E, Chalder T. Prevalence and predictors of recovery from chronic fatigue syndrome in a routine clinical practice. Behav Res The 2014;63:1-8.
- Crawley E, Collin SM, White PD, Rimes K, Sterne JAC, May MT, et al. Treatment outcome in adults with chronic fatigue syndrome: a prospective study in England based on the CFS/ME National Outcomes Database. QJM 2013;106:555-65.
- Huibers MJH, Bleijenberg G, van Amelsvoort LGPM, Beurskens AJHM, van Schayck CP, Bazelmans E, et al. Predictors of outcome in fatigued employees on sick leave: results from a randomised trial. J Psychosom Res 2004;57:443-9.
- Huibers MJH, Leone SS, Kant IJ, Knottnerus JA. Chronic fatigue syndrome-like caseness as a predictor of work status in fatigued employees on sick leave: four year follow up study. Occup Environ Med 2006;63:570-2.
- Leone SS, Huibers MJH, Kant I, Van Schayck CP, Bleijenberg G, Knottnerus JA. Long-term predictors of outcome in fatigued employees on sick leave: A 4-year follow-up study. Psychol Med 2006;36:1293-1300.
- Nyland M, Naess H, Birkeland JS, Nyland H. Longitudinal follow-up of employment status in patients with chronic fatigue syndrome after mononucleosis. BMJ open 2014;4:e005798.
- Jason LA, Porter N, Hunnell J, Rademaker A, Richman JA. CFS prevalence and risk factors over time. J Health Psychol 2011;16:445-56.
- Andersen MM, Permin H, Albrecht F. Illness and disability in Danish Chronic Fatigue Syndrome patients at diagnosis and 5-year follow-up. J Psychosom Res 2004;56:217-29.
- Brown MM, Bell DS, Jason LA, Christos C, Bell DE. Understanding long‐term outcomes of chronic fatigue syndrome. J Clin Psychol 2012;68:1028-35.
- McDermott C, Richards SCM, Ankers S, Selby M, Harmer J, Moran CJ. An evaluation of a chronic fatigue lifestyle management programme focusing on the outcome of return to work or training. Br J Occup Ther 2004;67:269-73.
- Cairns R, Hotopf M. A systematic review describing the prognosis of chronic fatigue syndrome. Occup Med (Lond) 2005;55:20-31.
- Bombardier CH, Buchwald D. Outcome and prognosis of patients with chronic fatigue vs chronic fatigue syndrome. Arch Intern Med 1995;155:2105-10.
- Tiersky LA DJ, Hill N, Dhar SK, Johnson SK, Lange G, Rappolt G, Natelson BH. Longitudinal assessment of neuropsychological functioning, psychiatric status, functional disability and employment status in chronic fatigue syndrome. Appl Neuropsychol 2001;8:41-50.
- Arroll MA, Senior V. Individuals’ experience of chronic fatigue syndrome/myalgic encephalomyelitis: an interpretative phenomenological analysis. Psychol Health 2008;23:443-58.
- Brooks J, King N, Wearden A. Couples’ experiences of interacting with outside others in chronic fatigue syndrome: a qualitative study. Chronic Illn 2014;10:5-17.
- Broughton J, Harris S, Beasant L, Crawley E, Collin SM. Adult patients’ experiences of NHS specialist services for chronic fatigue syndrome (CFS/ME): a qualitative study in England. BMC Health Serv Res 2017;17:384.
- de Carvalho Leite JC, de L Drachler M, Killett A, Kale S, Nacul L, McArthur M, et al. Social support needs for equity in health and social care: a thematic analysis of experiences of people with chronic fatigue syndrome/myalgic encephalomyelitis. Int J Equity Health 2011;10:46.
- Edwards CR, Thompson AR, Blair A. An ‘overwhelming illness’: women’s experiences of learning to live with chronic fatigue syndrome/myalgic encephalomyelitis. J Health Psychol 2007;12:203-14.
- Gilje AM, Soderlund A, Malterud K. Obstructions for quality care experienced by patients with chronic fatigue syndrome (CFS)--a case study. Patient Educ Couns 2008;73:36-41.
- Hannon K, Peters S, Fisher L, Riste L, Wearden A, Lovell K, et al. Developing resources to support the diagnosis and management of Chronic Fatigue Syndrome/Myalgic Encephalitis (CFS/ME) in primary care: a qualitative study. BMC Fam Pract 2012;13:93.
- Larun L, Malterud K. Finding the right balance of physical activity: a focus group study about experiences among patients with chronic fatigue syndrome. Patient Educ Couns 2011;83:222-6.
- McDermott C, Lynch J, Leydon GM. Patients’ hopes and expectations of a specialist chronic fatigue syndrome/ME service: a qualitative study. Fam Pract 2011;28:572-8.
- Ryckeghem H, Delesie L, Tobback E, Lievens S, Vogelaers D, Mariman A. Exploring the potential role of the advanced nurse practitioner within a care path for patients with chronic fatigue syndrome. J Adv Nurs 2017;73:1610-9.
- Stormorken E, Jason LA, Kirkevold M. Factors impacting the illness trajectory of post-infectious fatigue syndrome: a qualitative study of adults’ experiences. BMC Public Health 2017;17:952.
- Picariello F, Ali S, Foubister C, Chalder T. ‘It feels sometimes like my house has burnt down, but I can see the sky’: A qualitative study exploring patients’ views of cognitive behavioural therapy for chronic fatigue syndrome. Br J Health Psychol 2017;22:383-413.
- Pemberton S, Cox DL. Experiences of daily activity in chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME) and their implications for rehabilitation programmes. Disabil Rehabil 2014;36:1790-7.
- Son H-M, Park EY, Kim DH, Kim E, Shin M-S, Kim T-H. Experiences with, perceptions of and attitudes towards traditional Korean medicine (TKM) in patients with chronic fatigue: a qualitative, one-on-one, in-depth interview study. BMJ Open 2015;5:e006178.
- Cornes O. Chronic fatigue syndrome: a patient’s perspective. Br J Gen Pract 2013;63:648.
- Childs N, Robinson L, Chowdhury S, Ogden C, Newton JL. Consulting patients in setting priorities in Myalgic Encephalomyelitis (M.E.) research: findings from a national on-line survey. Res Involv Engagem 2015;1:11.
- Guise J, McVittie C, McKinlay A. A discourse analytic study of ME/CFS (Chronic Fatigue Syndrome) sufferers’ experiences of interactions with doctors. J Health Psychol 2010;15:426-35.
- Hansen AH, Lian OS. Experiences of general practitioner continuity among women with chronic fatigue syndrome/myalgic encephalomyelitis: a cross-sectional study. BMC Health Serv Res 2016;16:650.
- Hansen AH, Lian OS. How do women with chronic fatigue syndrome/myalgic encephalomyelitis rate quality and coordination of healthcare services? A cross-sectional study. BMJ Open 2016;6:e010277.
- Lian OS, Hansen AH. Factors facilitating patient satisfaction among women with medically unexplained long-term fatigue: A relational perspective. Health (London, England : 1997) 2016;20:308-26.
- Lian OS, Robson C. “It’s incredible how much I’ve had to fight.” Negotiating medical uncertainty in clinical encounters. Int J Qual Stud Health Well-being 2017;12:1392219.
- Van Hoof E. The doctor-patient relationship in chronic fatigue syndrome: survey of patient perspectives. Qual Prim Care 2009;17:263-70.
- Malterud K. Systematic text condensation: a strategy for qualitative analysis. Scand J Public Health 2012;40:795-805.
- Zachrisson O, Regland B, Jahreskog M, Jonsson M, Kron M, Gottfries CG. Treatment with staphylococcus toxoid in fibromyalgia/chronic fatigue syndrome--a randomised controlled trial. Eur J Pain 2002;6:455-66.
- Kaslow JE, Rucker L, Onishi R. Liver extract-folic acid-cyanocobalamin vs placebo for chronic fatigue syndrome. Arch Intern Med 1989;149:2501-3.
- Regland B, Forsmark S, Halaouate L, Matousek M, Peilot B, Zachrisson O, et al. Response to vitamin B12 and folic acid in myalgic encephalomyelitis and fibromyalgia. PloS One 2015;10:e0124648.
- Ljungar I, Hagman S, Wernegren H. Slutrapport av ME/CFS-projektet (Myalgisk Encefalomyelit/Chronic Fatigue Syndrom) Stockholm: Rehabiliteringsmedicinska Universitetskliniken Stockholm. 2013.
- Drachler Mde L, Leite JC, Hooper L, Hong CS, Pheby D, Nacul L, et al. The expressed needs of people with chronic fatigue syndrome/myalgic encephalomyelitis: a systematic review. BMC Public Health 2009;9:458.
- Larsson J, Lilliebjörk A. Chronic Fatigue Syndrome – the patients experiences of their health condition and multidisciplinary treatment. Karolinska Institutet. Avdelningen för neurobiologi, vårdvetenskap och samhälle. Stockholm; 2012.
- Bayliss K, Goodall M, Chisholm A, Fordham B, Chew-Graham C, Riste L, et al. Overcoming the barriers to the diagnosis and management of chronic fatigue syndrome/ME in primary care: a meta synthesis of qualitative studies. BMC Fam Pract 2014;15:44.
- Asbring P, Narvanen AL. Ideal versus reality: physicians perspectives on patients with chronic fatigue syndrome (CFS) and fibromyalgia. Soc Sci Med 2003;57:711-20.

 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services
 Share on Facebook
Share on Facebook
 Share on LinkedIn
Share on LinkedIn
 Share via Email
Share via Email