Diagnostics and treatment of provoked vestibulodynia
A Systematic Review
Conclusions
- It is not possible to estimate the effects of pharmacological treatment for provoked vestibulodynia from scientific studies, as the certainty of evidence is very low. For the same reason, it is not possible to estimate the effects of psychological treatments (various forms of cognitive behavioral therapy and mindfulness) or surgery.
- Multi modal physiotherapy (manual treatment, patient education, pelvic floor treatment and home exercises) may significantly reduce dyspareunia and improve sexual function, compared with topical treatment with lidocaine gel (low certainty of evidence).
- There are no well-conducted studies on diagnostic methods for provoked vestibulodynia.
- There is a need for well-conducted studies on treatment of provoked vestibulodynia. In particular, there is a need for studies on the effect of combined and multi professional treatments. To facilitate evidence synthesis and effect estimates, it is desirable to establish a core outcome set (an agreed set of outcomes that should be measured and reported in all clinical trials).
Several different treatments with diverse mechanisms of action were identified in the review but in most cases only one small or medium-sized study was found. This limited the possibilities to synthesize results and reach reliable conclusions about effects. Lack of evidence does not imply, however, that an intervention lacks effect, but rather that its effect has not been sufficiently researched.
The lack of evidence regarding diagnostic methods is regarded as less problematic, while a patient’s anamnesis in addition to the clinical investigation often is sufficient for an experienced clinician to confirm diagnosis.
Background
Provoked vestibulodynia (localised provoked vulvodynia) is a condition characterised by pain in the vestibular region of the vulva, present in sexual and nonsexual situations. The prevalence is highest among young women. Provoked vestibulodynia has a negative impact on the women’s sexual relations, wellbeing and quality of life.
Aim
The aim was to assess the scientific evidence for methods of diagnosing and treating provoked vestibulodynia through a systematic review. In addition, social and ethical aspects were addressed.
Method
A systematic review was conducted in accordance with the PRISMA statement. The certainty of evidence was assessed with GRADE.
Inclusion criteria:
PICO for treatment studies
Population: Women with provoked vestibulodynia in premenopausal age (study populations with up to 25% postmenopausal women were accepted).
Interventions:
- Pharmaceutical treatment
- Surgery
- Physiotherapy
- Psychological and psychosocial treatment or counselling
- Team based/multiprofessional treatment
- Multimodal/combined treatment
- Other treatments
Control: No treatment, wait-list, placebo or other defined treatment.
Outcome:
- Dyspareunia
- Pain upon pressure or touch
- Sexual function or satisfaction
- Quality of life
- Anxiety and depression
- Adverse effects and complications
Study design: Randomised controlled trials (RCT) and non-randomised studies of interventions (NRSI) with a comparison group.
PIRO for diagnostic studies
Population: Women with provoked vestibulodynia in premenopausal age.
Intervention: All diagnostic tests and methods.
Reference test: Clinical diagnosis.
Outcome: Sensitivity and specificity.
PICO for diagnostic studies
Population: Women with provoked vestibulodynia in premenopausal age.
Intervention: All diagnostic tests and methods.
Control: No diagnostic test or another diagnostic test.
Outcome: Positive and negative effects of the test.
Language:
English, Swedish, Norwegian or Danish.
Search period:
From 1990 to 2021. Final search January 2021.
Databases searched:
CINAHL (EBSCO), Cochrane Library (Wiley), Embase (Elsevier), Ovid (MEDLINE), PsycINFO (EBSCO) and Scopus (Elsevier).
In addition, the following sources were searched for systematic reviews used for information:
International HTA database, CRD Database (including HTA Database, DARE, NHS EED), Epistemonikos, Evidence search (NICE), KSR Evidence and PROSPERO.
Client/patient involvement:
Yes.
Results
No eligible studies on diagnostic methods with low or moderate risk of bias were identified in the assessment.
Regarding treatment methods, 24 studies with low or moderate risk of bias were identified that investigated 26 unique comparisons of interventions (Table 1).
| CBT = Cognitive Behavioral Therapy; NRSI = Non-Randomised Studies of Interventions; RCT = Randomised Controlled Study; TENS = Transcutaneous Electric Nerve Stimulation | ||||||||||||||
| Treatment form | Intervention | Comparison | Number of studies, study design | Number of study participants | ||||||||||
| Pharmacological treatment, oral | Gabapentin | Placebo | 1 RCT | 89 | ||||||||||
| Desipramine | Placebo | 1 RCT | 65 | |||||||||||
| Desipramine + lidocaine | Placebo | 1 RCT | 67 | |||||||||||
| Palmitoylethanolamide+ transpolydatine | Placebo | 1 RCT | 20 | |||||||||||
| Pharmacological treatment, topical | Nifedinpine | Placebo | 1 NRSI | 50 | ||||||||||
| Fibroblast lysate | Placebo | 1 RCT | 30 | |||||||||||
| Lidocaine | Placebo | 1 RCT | 66 | |||||||||||
| Estrogen | Placebo | 1 RCT | 20 | |||||||||||
| Diazepam | Placebo | 1 RCT | 42 | |||||||||||
| Cromolyn | Placebo | 1 RCT | 34 | |||||||||||
| Pharmacological treatment, injection | Botulinum toxin | Placebo | 3 RCT | 174 | ||||||||||
| Enoxaparin | Placebo | 1 RCT | 38 | |||||||||||
| Physiotherapy | EMG biofeedback | Lidocaine | 1 RCT | 46 | ||||||||||
| Traditional acupuncture | Non-traditional acupuncture | 1 RCT | 19 | |||||||||||
| Multimodal physiotherapy | Lidocaine | 1 RCT | 212 | |||||||||||
| TENS | Sham treatment | 1 RCT | 20 | |||||||||||
| Psychological treatment | Group CBT | Hydrocortisone | 1 RCT | 87 | ||||||||||
| Group CBT | Biofeedback or vestibulectomy (3-arm) | 1 RCT | 97 | |||||||||||
| Mindfulness-based cognitive therapy | CBT | 1 NRSI | 47 | |||||||||||
| CBT | Physiotherapy | 1 RCT | 20 | |||||||||||
| Mindfulness-based CBT | Education support | 1 RCT | 31 | |||||||||||
| Other treatments | Low-level laser therapy | Sham treatment | 1 RCT | 34 | ||||||||||
| Transcranial direct-current stimulation | Sham treatment | 1 RCT | 40 | |||||||||||
| Shock wave therapy | Sham treatment | 1 RCT | 34 | |||||||||||
Ethical and Social Aspects
The uncertainty regarding the effects of treatments for provoked vestibulodynia makes it difficult to help affected patients. This is unfortunate as the condition not only causes pain but also has psychosocial consequences. According to a previous Swedish report, patients have experienced difficulties in gaining access to investigation and treatment, and they do not always feel that they are taken seriously by the care staff. It is therefore important to improve the knowledge about provoked vulvodynia for healthcare professionals who meet women with the condition.
Conflicts of Interest
In accordance with SBU’s requirements, the experts and scientific reviewers participating in this project have submitted statements about conflicts of interest. These documents are available at SBU’s secretariat. SBU has determined that the conditions described in the submissions are compatible with the experts’ participation in the project.
The full report in Swedish
The full report in Swedish Diagnostik och behandling av provocerad vulvodyni
Scientific article
Bohm-Starke N, Ramsay KW, Lytsy P, Nordgren B, Sjöberg I, Moberg K, et al. Treatment of Provoked Vulvodynia: A Systematic Review. The Journal of Sexual Medicine. Available from: https://doi.org/10.1016/j.jsxm.2022.02.008.
Project group
Experts
- Nina Bohm Starke
- Ida Flink
- Birgitta Nordgren
- Inga Sjöberg
SBU
- Karin Wilbe Ramsay (Project Manager)
- Per Lytsy
- Maria Ahlberg
- Klas Moberg
Flow Chart
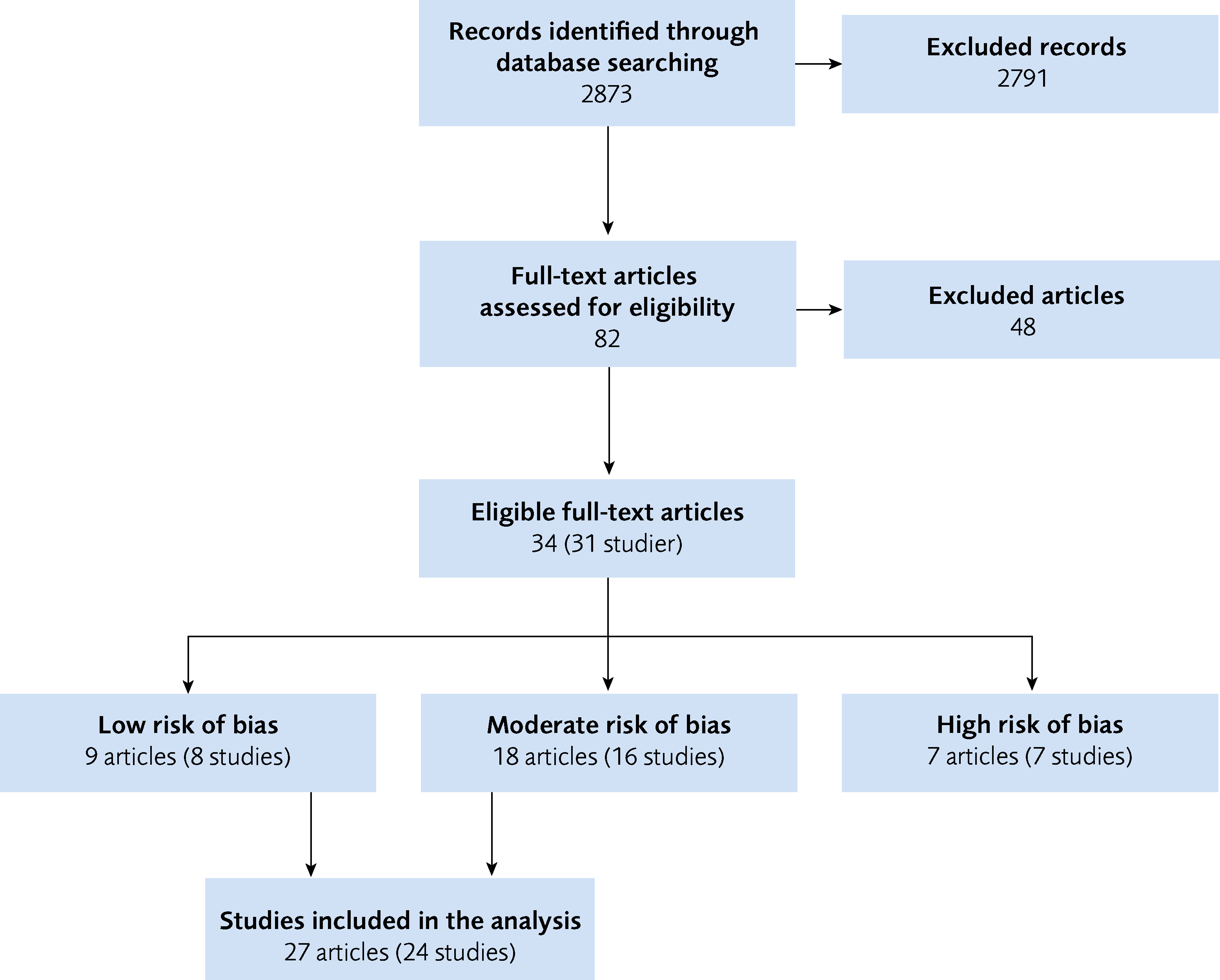
Figure 1 Flow Chart
References
- SBU. Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten: en metodbok. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2020. [accessed April 27 2021]. Available from: https://www.sbu.se/metodbok.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. Available from: https://doi.org/10.1136/bmj.n71.
- SBU. Etiska aspekter på insatser inom hälso- och sjukvården. En vägledning för att identifiera relevanta etiska aspekter. In: Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten: en metodbok. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2020. [accessed 27 April 2021]. Available from: https://www.sbu.se/globalassets/ebm/etiska_aspekter_halso_sjukvarden.pdf.
- Brown CS, Bachmann GA, Wan J, Foster DC, Gabapentin Study G. Gabapentin for the Treatment of Vulvodynia: A Randomized Controlled Trial. Obstet Gynecol. 2018;131(6):1000-07. Available from: https://doi.org/10.1097/AOG.0000000000002617.
- Bachmann GA, Brown CS, Phillips NA, Rawlinson LA, Yu X, Wood R, et al. Effect of gabapentin on sexual function in Vulvodynia: A randomized, placebo-controlled trial. Obstet Gynecol Surv. 2019;74(2):82-83. Available from: https://doi.org/10.1016/j.ajog.2018.10.021.
- Foster DC, Kotok MB, Huang LS, Watts A, Oakes D, Howard FM, et al. Oral desipramine and topical lidocaine for vulvodynia: a randomized controlled trial. Obstet Gynecol. 2010;116(3):583-93. Available from: https://doi.org/10.1097/AOG.0b013e3181e9e0ab.
- Murina F, Graziottin A, Felice R, Radici G, Tognocchi C. Vestibulodynia: synergy between palmitoylethanolamide + transpolydatin and transcutaneous electrical nerve stimulation. J Low Genit Tract Dis. 2013;17(2):111-16. Available from: https://doi.org/10.1097/LGT.0b013e3182652316.
- Bornstein J, Tuma R, Farajun Y, Azran A, Zarfati D. Topical nifedipine for the treatment of localized provoked vulvodynia: a placebo-controlled study. J Pain. 2010;11(12):1403-09. Available from: https://doi.org/10.1016/j.jpain.2010.03.016.
- Donders GG, Bellen G. Cream with cutaneous fibroblast lysate for the treatment of provoked vestibulodynia: a double-blind randomized placebo-controlled crossover study. J Low Genit Tract Dis. 2012;16(4):427-36. Available from: https://doi.org/10.1097/LGT.0b013e31825a2274.
- Langlais EL, Lefebvre J, Maheux-Lacroix S, Bujold E, Fortier M, Bouchard C. Treatment of Secondary Vestibulodynia with Conjugated Estrogen Cream: A Pilot, Double-Blind, Randomized Placebo-Controlled Trial. Journal of Obstetrics & Gynaecology Canada: JOGC. 2017;39(6):453-58. Available from: https://doi.org/10.1016/j.jogc.2016.10.011.
- Murina F, Felice R, Di Francesco S, Oneda S. Vaginal diazepam plus transcutaneous electrical nerve stimulation to treat vestibulodynia: A randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2018;228:148-53. Available from: https://doi.org/10.1016/j.ejogrb.2018.06.026.
- Nyirjesy P, Sobel JD, Weitz MV, Leaman DJ, Small MJ, Gelone SP. Cromolyn cream for recalcitrant idiopathic vulvar vestibulitis: results of a placebo controlled study. Sex Transm Infect. 2001;77(1):53-57. Available from: https://doi.org/10.1136/sti.77.1.53.
- Diomande I, Gabriel N, Kashiwagi M, Ghisu GP, Welter J, Fink D, et al. Subcutaneous botulinum toxin type A injections for provoked vestibulodynia: a randomized placebo-controlled trial and exploratory subanalysis. Arch Gynecol Obstet. 2019;299(4):993-1000. Available from: https://doi.org/10.1007/s00404-019-05043-w.
- Haraldson P, Muhlrad H, Heddini U, Nilsson K, Bohm-Starke N. Botulinum Toxin A as a Treatment for Provoked Vestibulodynia: A Randomized Controlled Trial. Obstet Gynecol. 2020;136(3):524-32. Available from: https://doi.org/10.1097/AOG.0000000000004008.
- Petersen CD, Giraldi A, Lundvall L, Kristensen E. Botulinum toxin type A-a novel treatment for provoked vestibulodynia? Results from a randomized, placebo controlled, double blinded study. J Sex Med. 2009;6(9):2523-37. Available from: https://doi.org/10.1111/j.1743-6109.2009.01378.x.
- Farajun Y, Zarfati D, Abramov L, Livoff A, Bornstein J. Enoxaparin treatment for vulvodynia: a randomized controlled trial. Obstet Gynecol. 2012;120(3):565-72. Available from: https://doi.org/10.1097/AOG.0b013e3182657de6.
- Danielsson I, Torstensson T, Brodda-Jansen G, Bohm-Starke N. EMG biofeedback versus topical lidocaine gel: a randomized study for the treatment of women with vulvar vestibulitis. Acta Obstet Gynecol Scand. 2006;85(11):1360-67. Available from: https://doi.org/10.1080/00016340600883401.
- Hullender Rubin LE, Mist SD, Schnyer RN, Chao MT, Leclair CM. Acupuncture Augmentation of Lidocaine for Provoked, Localized Vulvodynia: A Feasibility and Acceptability Study. J Low Genit Tract Dis. 2019;23(4):279-86. Available from: https://doi.org/10.1097/LGT.0000000000000489.
- Morin M, Dumoulin C, Bergeron S, Mayrand MH, Khalife S, Waddell G, et al. Multimodal physical therapy versus topical lidocaine for provoked vestibulodynia: a prospective, multicenter, randomized trial. Am J Obstet Gynecol. 2020;18:18. Available from: https://doi.org/https://dx.doi.org/10.1016/j.ajog.2020.08.038.
- Murina F, Bianco V, Radici G, Felice R, Di Martino M, Nicolini U. Transcutaneous electrical nerve stimulation to treat vestibulodynia: a randomised controlled trial. BJOG. 2008;115(9):1165-70. Available from: https://doi.org/10.1111/j.1471-0528.2008.01803.x.
- Bergeron S, Khalife S, Dupuis MJ, McDuff P. A randomized clinical trial comparing group cognitive-behavioral therapy and a topical steroid for women with dyspareunia. J Consult Clin Psychol. 2016;84(3):259-68. Available from: https://doi.org/10.1037/ccp0000072.
- Bergeron S, Binik YM, Khalife S, Pagidas K, Glazer HI, Meana M, et al. A randomized comparison of group cognitive--behavioral therapy, surface electromyographic biofeedback, and vestibulectomy in the treatment of dyspareunia resulting from vulvar vestibulitis. Pain. 2001;91(3):297-306.
- Bergeron S, Khalife S, Glazer HI, Binik YM. Surgical and behavioral treatments for vestibulodynia: two-and-one-half year follow-up and predictors of outcome. Obstet Gynecol. 2008;111(1):159-66. Available from: https://doi.org/10.1097/01.AOG.0000295864.76032.a7.
- Brotto LA, Bergeron S, Zdaniuk B, Basson R. Mindfulness and cognitive behavior therapy for provoked vestibulodynia: Mediators of treatment outcome and long-term effects. J Consult Clin Psychol. 2020;88(1):48-64.
- Brotto LA, Bergeron S, Zdaniuk B, Driscoll M, Grabovac A, Sadownik LA, et al. A Comparison of Mindfulness-Based Cognitive Therapy Vs Cognitive Behavioral Therapy for the Treatment of Provoked Vestibulodynia in a Hospital Clinic Setting. J Sex Med. 2019;16(6):909-23. Available from: https://doi.org/10.1016/j.jsxm.2019.04.002.
- Goldfinger C, Pukall CF, Thibault-Gagnon S, McLean L, Chamberlain S. Effectiveness of Cognitive-Behavioral Therapy and Physical Therapy for Provoked Vestibulodynia: A Randomized Pilot Study. J Sex Med. 2016;13(1):88-94. Available from: https://doi.org/10.1016/j.jsxm.2015.12.003.
- Guillet AD, Cirino NH, Hart KD, Leclair CM. Mindfulness-Based Group Cognitive Behavior Therapy for Provoked Localized Vulvodynia: A Randomized Controlled Trial. J Low Genit Tract Dis. 2019;23(2):170-75. Available from: https://doi.org/10.1097/LGT.0000000000000456.
- Lev-Sagie A, Kopitman A, Brzezinski A. Low-Level Laser Therapy for the Treatment of Provoked Vestibulodynia-A Randomized, Placebo-Controlled Pilot Trial. J Sex Med. 2017;14(11):1403-11. Available from: https://doi.org/10.1016/j.jsxm.2017.09.004.
- Morin A, Leonard G, Gougeon V, Cyr MP, Waddell G, Bureau YA, et al. Efficacy of transcranial direct-current stimulation in women with provoked vestibulodynia. Am J Obstet Gynecol. 2017;216(6):584.e81-84.e11.
- Gruenwald I, Gutzeit O, Petruseva A, Gartman I, Lowenstein L. Low-Intensity Shockwave for Treatment of Vestibulodynia: A Randomized Controlled Therapy Trial. J Sex Med. 2021;05:05. Available from: https://doi.org/https://dx.doi.org/10.1016/j.jsxm.2020.11.006.
- Regeringen. Regleringsbrev för budgetåret 2020 avseende Statens beredning för medicinsk och social utvärdering. Socialdepartementet. S2019/05315/RS. Stockholm. [accessed 27 April 2021]. Available from: https://www.sbu.se/contentassets/27d2ce03efaa439b8f3484405eaeb96b/regleringsbrev-for-bp-2020-avseende-sbu-s2019_05315_rs-delvis.pdf.
- Bornstein J, Goldstein AT, Stockdale CK, Bergeron S, Pukall C, Zolnoun D, et al. 2015 ISSVD, ISSWSH and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia. Obstet Gynecol. 2016;127(4):745-51. Available from: https://doi.org/10.1097/AOG.0000000000001359.
- Friedrich EG, Jr. Vulvar vestibulitis syndrome. J Reprod Med. 1987;32(2):110-4.
- SFOG. Diagnoshandbok för kvinnosjukvården 2020. Stockholm: Svensk förening för Obstetrik och Gynekologi; 2020. [accessed 27 April 2021]. Available from: https://www.sfog.se/natupplaga/NY_Diagnob1251a05-6ff5-4f49-b4c8-a6f9271bae9d.pdf.
- Harlow BL, Stewart EG. A population-based assessment of chronic unexplained vulvar pain: have we underestimated the prevalence of vulvodynia? J Am Med Womens Assoc (1972). 2003;58(2):82-8.
- Harlow BL, Kunitz CG, Nguyen RH, Rydell SA, Turner RM, MacLehose RF. Prevalence of symptoms consistent with a diagnosis of vulvodynia: population-based estimates from 2 geographic regions. Am J Obstet Gynecol. 2014;210(1):40 e1-8. Available from: https://doi.org/10.1016/j.ajog.2013.09.033.
- Danielsson I, Sjoberg I, Stenlund H, Wikman M. Prevalence and incidence of prolonged and severe dyspareunia in women: results from a population study. Scand J Public Health. 2003;31(2):113-8. Available from: https://doi.org/10.1080/14034940210134040.
- Ekdahl J, Flink I, Engman L, Linton SJ. Vulvovaginal Pain from a Fear-Avoidance Perspective: A Prospective Study Among Female University Students in Sweden. International Journal of Sexual Health. 2018;30(1):49-59. Available from: https://doi.org/10.1080/19317611.2017.1404543.
- Elmerstig E, Wijma B, Swahnberg K. Young Swedish women's experience of pain and discomfort during sexual intercourse. Acta Obstet Gynecol Scand. 2009;88(1):98-103. Available from: https://doi.org/10.1080/00016340802620999.
- Folkhälsomyndigheten. Sexuell reproduktiv hälsa och rättigheter i Sverige från 2017. Stockholm: Folkhälsomyndigheten; 2017. [accessed 27 April 2021]. Available from: https://www.folkhalsomyndigheten.se/publicerat-material/publikationsarkiv/s/sexuell-och-reproduktiv-halsa-och-rattigheter-i-sverige-2017/?pub=60999.
- Socialstyrelsen. Kartläggning av vestibulit. Förekomst och behandling av flickor och kvinnor med vestibulit samt behov av kunskapsstöd. Stockholm: Socialstyrelsen; 2018. [accessed 27 April 2021]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2018-6-16.pdf.
- Arnold LD, Bachmann GA, Rosen R, Rhoads GG. Assessment of vulvodynia symptoms in a sample of US women: a prevalence survey with a nested case control study. Am J Obstet Gynecol. 2007;196(2):128 e1-6. Available from: https://doi.org/10.1016/j.ajog.2006.07.047.
- Bergeron S, Reed BD, Wesselmann U, Bohm-Starke N. Vulvodynia. Nat Rev Dis Primers. 2020;6(1):36. Available from: https://doi.org/10.1038/s41572-020-0164-2.
- Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull. 2007;133(4):581-624. Available from: https://doi.org/10.1037/0033-2909.133.4.581.
- Thomten J, Linton SJ. When sex hurts: Female genital pain with sexual consequences deserves attention: A position paper. Scand J Pain. 2014;5(3):202-05. Available from: https://doi.org/10.1016/j.sjpain.2014.04.001.
- Bohm-Starke N, Hilliges M, Brodda-Jansen G, Rylander E, Torebjork E. Psychophysical evidence of nociceptor sensitization in vulvar vestibulitis syndrome. Pain. 2001;94(2):177-83. Available from: https://doi.org/10.1016/S0304-3959(01)00352-9.
- Bohm-Starke N, Hilliges M, Falconer C, Rylander E. Increased intraepithelial innervation in women with vulvar vestibulitis syndrome. Gynecol Obstet Invest. 1998;46(4):256-60. Available from: https://doi.org/10.1159/000010045.
- Pukall CF, Goldstein AT, Bergeron S, Foster D, Stein A, Kellogg-Spadt S, et al. Vulvodynia: Definition, Prevalence, Impact, and Pathophysiological Factors. J Sex Med. 2016;13(3):291-304. Available from: https://doi.org/10.1016/j.jsxm.2015.12.021.
- Wesselmann U, Bonham A, Foster D. Vulvodynia: Current state of the biological science. Pain. 2014;155(9):1696-701. Available from: https://doi.org/10.1016/j.pain.2014.05.010.
- Reed BD, Harlow SD, Sen A, Edwards RM, Chen D, Haefner HK. Relationship between vulvodynia and chronic comorbid pain conditions. Obstet Gynecol. 2012;120(1):145-51. Available from: https://doi.org/10.1097/AOG.0b013e31825957cf.
- Harlow BL, Caron RE, Parker SE, Chatterjea D, Fox MP, Nguyen RHN. Recurrent Yeast Infections and Vulvodynia: Can We Believe Associations Based on Self-Reported Data? J Womens Health (Larchmt). 2017;26(10):1069-76. Available from: https://doi.org/10.1089/jwh.2016.5777.
- Falsetta ML, Foster DC, Woeller CF, Pollock SJ, Bonham AD, Haidaris CG, et al. Identification of novel mechanisms involved in generating localized vulvodynia pain. Am J Obstet Gynecol. 2015;213(1):38 e1-38 e12. Available from: https://doi.org/10.1016/j.ajog.2015.02.002.
- Farmer MA, Taylor AM, Bailey AL, Tuttle AH, MacIntyre LC, Milagrosa ZE, et al. Repeated vulvovaginal fungal infections cause persistent pain in a mouse model of vulvodynia. Sci Transl Med. 2011;3(101):101ra91. Available from: https://doi.org/10.1126/scitranslmed.3002613.
- Harlow BL, Vitonis AF, Stewart EG. Influence of oral contraceptive use on the risk of adult-onset vulvodynia. J Reprod Med. 2008;53(2):102-10.
- Reed BD, Harlow SD, Legocki LJ, Helmuth ME, Haefner HK, Gillespie BW, et al. Oral contraceptive use and risk of vulvodynia: a population-based longitudinal study. BJOG. 2013;120(13):1678-84. Available from: https://doi.org/10.1111/1471-0528.12407.
- Morin M, Bergeron S, Khalife S, Mayrand MH, Binik YM. Morphometry of the pelvic floor muscles in women with and without provoked vestibulodynia using 4D ultrasound. J Sex Med. 2014;11(3):776-85. Available from: https://doi.org/10.1111/jsm.12367.
- Arnold LD, Bachmann GA, Rosen R, Kelly S, Rhoads GG. Vulvodynia: characteristics and associations with comorbidities and quality of life. Obstet Gynecol. 2006;107(3):617-24. Available from: https://doi.org/10.1097/01.AOG.0000199951.26822.27.
- Harlow BL, Stewart EG. Adult-onset vulvodynia in relation to childhood violence victimization. Am J Epidemiol. 2005;161(9):871-80. Available from: https://doi.org/10.1093/aje/kwi108.
- Landry T, Bergeron S. Biopsychosocial factors associated with dyspareunia in a community sample of adolescent girls. Arch Sex Behav. 2011;40(5):877-89. Available from: https://doi.org/10.1007/s10508-010-9637-9.
- Leclerc B, Bergeron S, Binik YM, Khalife S. History of sexual and physical abuse in women with dyspareunia: association with pain, psychosocial adjustment, and sexual functioning. J Sex Med. 2010;7(2 Pt 2):971-80. Available from: https://doi.org/10.1111/j.1743-6109.2009.01581.x.
- Bois K, Bergeron S, Rosen N, Mayrand MH, Brassard A, Sadikaj G. Intimacy, sexual satisfaction, and sexual distress in vulvodynia couples: An observational study. Health Psychol. 2016;35(6):531-40. Available from: https://doi.org/10.1037/hea0000289.
- Rosen NO, Bois K, Mayrand MH, Vannier S, Bergeron S. Observed and Perceived Disclosure and Empathy Are Associated With Better Relationship Adjustment and Quality of Life in Couples Coping With Vulvodynia. Arch Sex Behav. 2016;45(8):1945-56. Available from: https://doi.org/10.1007/s10508-016-0739-x.
- Desrochers G, Bergeron S, Khalife S, Dupuis MJ, Jodoin M. Fear avoidance and self-efficacy in relation to pain and sexual impairment in women with provoked vestibulodynia. Clin J Pain. 2009;25(6):520-7. Available from: https://doi.org/10.1097/AJP.0b013e31819976e3.
- Engman L, Flink IK, Ekdahl J, Boersma K, Linton SJ. Avoiding or enduring painful sex? A prospective study of coping and psychosexual function in vulvovaginal pain. Eur J Pain. 2018. Available from: https://doi.org/10.1002/ejp.1227.
- Charbonneau-Lefebvre V, Vaillancourt-Morel MP, Brassard A, Steben M, Bergeron S. Self-Efficacy Mediates the Attachment-Pain Association in Couples with Provoked Vestibulodynia: A Prospective Study. J Sex Med. 2019;16(11):1803-13. Available from: https://doi.org/10.1016/j.jsxm.2019.08.012.
- Flink I, Engman L, Thomtén J, Linton SJ. The role of catastrophizing in vulvovaginal pain: Impact on pain and partner responses over time. e12093. J Appl Biobehav Res. 2017;22(1). Available from: https://doi.org/https://doi.org/10.1111/jabr.12093.
- Davis SN, Bergeron S, Bois K, Sadikaj G, Binik YM, Steben M. A prospective 2-year examination of cognitive and behavioral correlates of provoked vestibulodynia outcomes. Clin J Pain. 2015;31(4):333-41. Available from: https://doi.org/10.1097/AJP.0000000000000128.
- Tribo MJ, Canal C, Banos JE, Robleda G. Pain, Anxiety, Depression, and Quality of Life in Patients with Vulvodynia. Dermatology. 2020;236(3):255-61. Available from: https://doi.org/10.1159/000503321.
- Paquet M, Rosen NO, Steben M, Mayrand MH, Santerre-Baillargeon M, Bergeron S. Daily Anxiety and Depressive Symptoms in Couples Coping With Vulvodynia: Associations With Women's Pain, Women's Sexual Function, and Both Partners' Sexual Distress. J Pain. 2018;19(5):552-61. Available from: https://doi.org/10.1016/j.jpain.2017.12.264.
- SFOG. Vulvovaginala sjukdomar. Stockholm: Svensk förening för Obstetrik och Gynekologi; 2013 rapport nr 71. [accessed 27 April 2021]. Available from: https://www.sfog.se/media/141501/info71_web.pdf.
- Dargie EE, Chamberlain SM, Pukall CF. Provoked Vestibulodynia: Diagnosis, Self-Reported Pain, and Presentation During Gynaecological Examinations. J Obstet Gynaecol Can. 2017;39(3):145-51. Available from: https://doi.org/10.1016/j.jogc.2017.01.001.
- Stenson AL. Vulvodynia: Diagnosis and Management. Obstet Gynecol Clin North Am. 2017;44(3):493-508. Available from: https://doi.org/10.1016/j.ogc.2017.05.008.
- Bortolami A, Vanti C, Banchelli F, Guccione AA, Pillastrini P. Relationship between female pelvic floor dysfunction and sexual dysfunction: an observational study. J Sex Med. 2015;12(5):1233-41. Available from: https://doi.org/10.1111/jsm.12882.
- Rosen NO, Dawson SJ, Brooks M, Kellogg-Spadt S. Treatment of Vulvodynia: Pharmacological and Non-Pharmacological Approaches. Drugs. 2019;79(5):483-93. Available from: https://doi.org/10.1007/s40265-019-01085-1.
- Pukall CF, Bergeron S, Brown C, Bachmann G, Wesselmann U, Vulvodynia Collaborative Research G. Recommendations for Self-Report Outcome Measures in Vulvodynia Clinical Trials. Clin J Pain. 2017;33(8):756-65. Available from: https://doi.org/10.1097/AJP.0000000000000453.
- Shallcross R, Dickson JM, Nunns D, Mackenzie C, Kiemle G. Women's Subjective Experiences of Living with Vulvodynia: A Systematic Review and Meta-Ethnography. Arch Sex Behav. 2018;47(3):577-95. Available from: https://doi.org/10.1007/s10508-017-1026-1.
- Heddini U, Bohm-Starke N, Nilsson KW, Johannesson U. Provoked vestibulodynia--medical factors and comorbidity associated with treatment outcome. J Sex Med. 2012;9(5):1400-6. Available from: https://doi.org/10.1111/j.1743-6109.2012.02665.x.
- Xie Y, Shi L, Xiong X, Wu E, Veasley C, Dade C. Economic burden and quality of life of vulvodynia in the United States. Curr Med Res Opin. 2012;28(4):601-8. Available from: https://doi.org/10.1185/03007995.2012.666963.
- Johnson NS, Harwood EM, Nguyen RH. "You have to go through it and have your children": reproductive experiences among women with vulvodynia. BMC Pregnancy Childbirth. 2015;15:114. Available from: https://doi.org/10.1186/s12884-015-0544-x.
- Moller L, Josefsson A, Bladh M, Lilliecreutz C, Sydsjo G. Reproduction and mode of delivery in women with vaginismus or localised provoked vestibulodynia: a Swedish register-based study. BJOG. 2015;122(3):329-34. Available from: https://doi.org/10.1111/1471-0528.12946.
- GRADE. The GRADE working group. [accessed April 27 2021]. Available from: https://www.gradeworkinggroup.org/.
- Bornstein J, Goldschmid N, Sabo E. Hyperinnervation and mast cell activation may be used as histopathologic diagnostic criteria for vulvar vestibulitis. Gynecol Obstet Invest. 2004;58(3):171-78. Available from: https://doi.org/10.1159/000079663.
- Bergeron S, Binik YM, Khalife S, Pagidas K, Glazer HI. Vulvar vestibulitis syndrome: reliability of diagnosis and evaluation of current diagnostic criteria. Obstet Gynecol. 2001;98(1):45-51. Available from: https://doi.org/10.1016/s0029-7844(01)01389-8.
- Brotto LA, Zdaniuk B, Rietchel L, Basson R, Bergeron S. Moderators of Improvement From Mindfulness-Based vs Traditional Cognitive Behavioral Therapy for the Treatment of Provoked Vestibulodynia. J Sex Med. 2020;17(11):2247-59. Available from: https://doi.org/https://dx.doi.org/10.1016/j.jsxm.2020.07.080.
- FASS. Stockholm: FASS. [accessed April 27 2012]. Available from: https://www.fass.se/LIF/startpage.
- Tympanidis P, Terenghi G, Dowd P. Increased innervation of the vulval vestibule in patients with vulvodynia. Br J Dermatol. 2003;148(5):1021-27. Available from: https://doi.org/10.1046/j.1365-2133.2003.05308.x.
- De Andres J, Sanchis-Lopez N, Asensio-Samper JM, Fabregat-Cid G, Villanueva-Perez VL, Monsalve Dolz V, et al. Vulvodynia--An Evidence-Based Literature Review and Proposed Treatment Algorithm. Pain Practice. 2016;16(2):204-36. Available from: https://doi.org/10.1111/papr.12274.
- Loflin BJ, Westmoreland K, Williams NT. Vulvodynia: A Review of the Literature. J Pharm Technol. 2019;35(1):11-24.
- David A, Bornstein J. Evaluation of Long-Term Surgical Success and Satisfaction of Patients After Vestibulectomy. J Low Genit Tract Dis. 2020;24(4):399-404. Available from: https://doi.org/https://dx.doi.org/10.1097/LGT.0000000000000552.
- Davenport RB, Voutier CR, Veysey EC. Outcome Measurement Instruments for Provoked Vulvodynia: A Systematic Review. J Low Genit Tract Dis. 2018;22(4):396-404. Available from: https://doi.org/10.1097/LGT.0000000000000418.
- Sadownik LA, Yong PJ, Smith KB. Systematic Review of Treatment Outcome Measures for Vulvodynia. J Low Genit Tract Dis. 2018;22(3):251-59. Available from: https://doi.org/10.1097/LGT.0000000000000406.
- SBU. Rehabilitering vid långvarig smärta. En systematisk litteraturöversikt. Stockholm: Statens beredning för medicinsk utvärdering (SBU); 2010. SBU-rapport nr 198. ISBN 978-91-85413-34-8. https://www.sbu.se/sv/publikationer/SBU-utvarderar/rehabilitering-vid-langvarig-smarta/

 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services
 Share on Facebook
Share on Facebook
 Share on LinkedIn
Share on LinkedIn
 Share via Email
Share via Email