Prioritized research questions regarding pregnancy-related pelvic girdle pain
Based on the James Lind Alliance method
Aim
The aim of this project is to provide a top-10 list of the most important research questions, according to patients with pregnancy-related pelvic girdle pain, carers and clinicians.
The project has been conducted by SBU on commission of the Government.
The herein published report (in Swedish) is directed to the Government, researchers, research funding bodies and caregivers. Other relevant target groups for this report are decision makers within health care, patients and their families.
Background
Pregnancy-related pelvic girdle pain affects up to 50 % of pregnant women and for 10 % the pain persist after the child is born. The condition is characterized by pain in the pelvis and a reduced function capacity, foremost during the pregnancy, but also following childbirth. In severe cases, women with pregnancy-related pelvic girdle pain experience high levels of discomfort due to which they require help with their daily activities.
The diagnosis of pelvic girdle pain is set following a standardized examination protocol where lower back pain has been ruled out, and pelvic girdle pain has been provoked by specific tests. Treatments includes information, ergonomic advice, a pelvic support belt, acupuncture, crutches, exercises to strengthen the muscles and part- or full-time sick leave.
There is an obvious need for more research within this field. An evidence map published in 2021 (in Swedish) points out the need for both primary studies and systematic reviews.
Method
The project used the James Lind Alliance (JLA) method (https://www.jla.nihr.ac.uk/). This is a method that brings participants i.e., patients, carers and clinicians together to identify and prioritize unanswered questions or evidence uncertainties that they agree are the most important. The participants in this project were recruited through a declaration of interest that could be found on SBU: s website. Information about the project was spread through social media (Facebook, Twitter, LinkedIn), SBU´s newsletter as well as via e-mails to various organizations.
The project consisted of two parts: one inventory part where the research questions were identified and a second part where the identified research questions were prioritized, resulting in a top-10 list of prioritized research questions ranked from 1 to 10 (Figure 1).
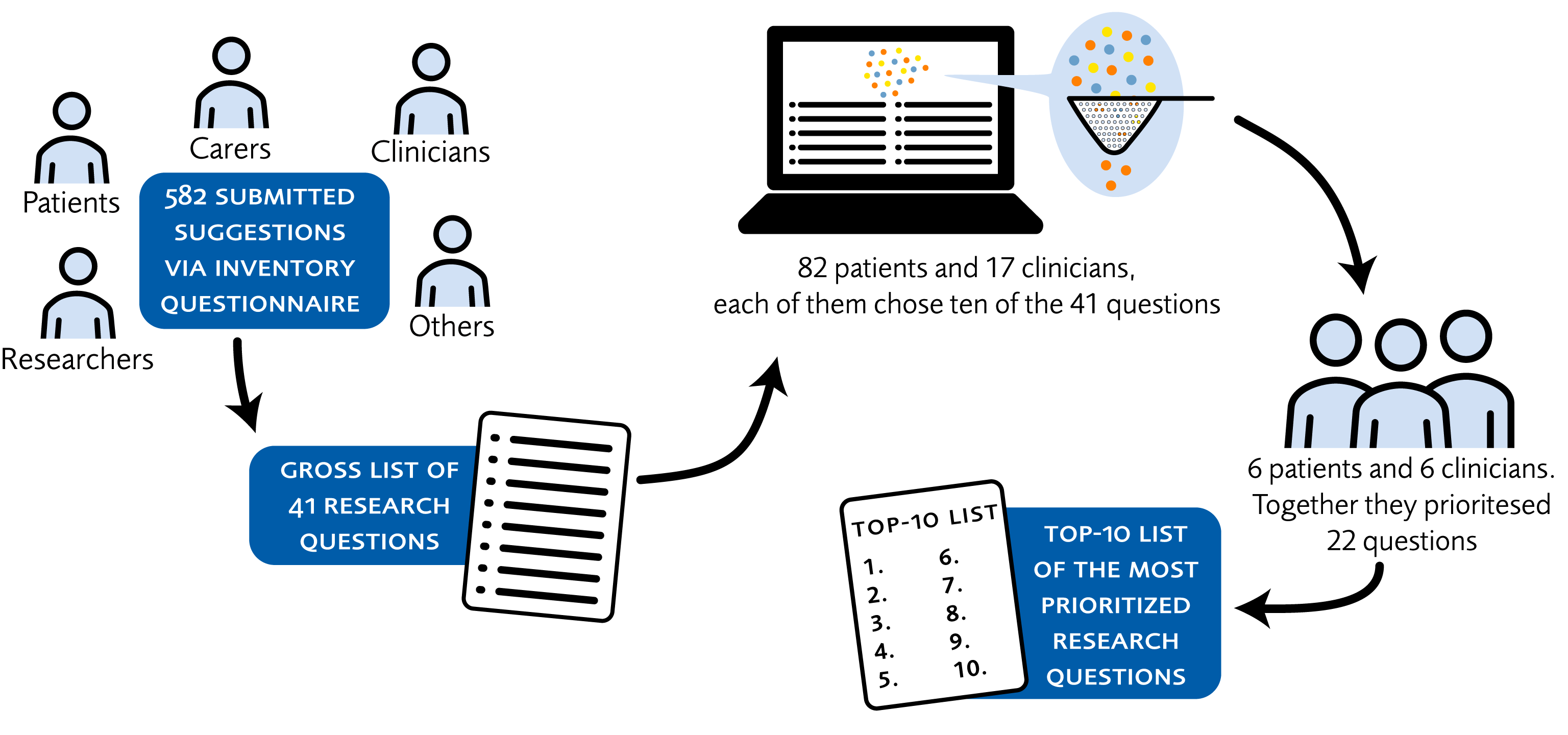
Figure 1. The different steps resulting in a top 10-list
Results
| 1. | What is the effect of coherent course of care where various professions collaborate to rehabilitate women with pregnancy-related pelvic girdle pain? |
| 2. | What are the economic consequences for the society related to pregnancy-related pelvic girdle pain, when the patients and carers must be on sick leave or work with reduced capacity as well as when the patient has to retrain to a different profession due to persistent complications? |
| 3. | What is the effect of interventions aiming to increase the clinicians´ knowledge of diagnostic, course, and treatment of pregnancy-related pelvic girdle pain on the care given for this condition? |
| 4. | Are there any measures that can be taken to avoid being affected by pregnancy-related pelvic girdle pain during or after a pregnancy, and if so, what are the risk- and protective factors, respectively? |
| 5. | Following childbirth, when and how should women with pregnancy-related pelvic girdle pain be followed up to prevent long-term persistent pelvic girdle pain? |
| 6. | How is the woman’s quality of life, including function, social- and professional life, affected by pregnancy-related pelvic girdle pain? |
| 7. | What is the societal attitude to pregnancy-related pelvic girdle pain and how does it influence the possibility for the women to receive treatment, support and help? |
| 8. | What is the effect of personalized training to strengthen the muscles through pregnancy-related pelvic girdle pain, during and after the pregnancy? |
| 9. | What are the economic consequences for the patient regarding costs related to pregnancy-related pelvic girdle pain, such as costs for health care and sick leave as well as costs for reduced working capacity and retraining to a different profession due to persistent complications? |
| 10 | What are the effects of being on sick leave for women with pregnancy-related pelvic girdle pain? |
Discussion
The top 10 research questions that were considered the most prioritized in this project included treatment of pelvic girdle pain and effects on the patient’s daily life. The most prioritized research question focused on the effects of a coherent course of care. In addition, socioeconomically effects, knowledge-raising measures for clinicians, effects of preventive- and treatment interventions, follow up after childbirth, attitudes in the society, as well as effects on the quality of life for the woman and her family, were included in the top 10 research questions.
Many of the prioritized research questions are wide and future research needs to formulate several specific research questions, followed by studies that should aim to answer each of the prioritized questions. However, before starting such research projects, search for any existing evidence should be performed, if not within the field of pelvic girdle pain, then perhaps within a similar area for which the results could be applicable to the area of pregnancy-related pelvic girdle pain. It is thus of importance that the researchers first conduct a systematic review of potentially already existing data and determine if new research is needed or whether implementation of evidence should be facilitated.
Project group
Experts
- Helen Elden, Reg. Midwife, Professor, University of Gothenburg
- Annelie Gutke, Physiotherapist, Lecturer, University of Gothenburg
- Elin Naurin, Professor, University of Gothenburg
SBU
- Helena Domeij, Project Manager
- Karin Rydin, Assistant Project Manager
- Irini Åberg, Project Administrator
- Jenny Kärrholm, Head of department
References
- SBU. Kartläggning av metoder för diagnostik och behandling av graviditetskomplikationen graviditetsrelaterad bäckensmärta – Identifiering av evidens och vetenskapliga kunskapsluckor utifrån systematiska översikter. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2021. SBU Kartlägger 320_1. [accessed Jan 18 2022]. Available from: https://www.sbu.se/320_1
- Gutke A, Ostgaard HC, Oberg B. Pelvic girdle pain and lumbar pain in pregnancy: a cohort study of the consequences in terms of health and functioning. Spine (Phila Pa 1976). 2006;31(5):E149-55. Available from: https://doi.org/10.1097/01.brs.0000201259.63363.e1.
- Remus A, Smith V, Gutke A, Mena JJS, Morkved S, Wikmar LN, et al. A core outcome set for research and clinical practice in women with pelvic girdle pain: PGP-COS. PLoS One. 2021;16(2):e0247466. Available from: https://doi.org/10.1371/journal.pone.0247466.
- Liddle SD, Pennick V. Interventions for preventing and treating low-back and pelvic pain during pregnancy. Cochrane Database Syst Rev. 2015(9):CD001139. Available from: https://doi.org/10.1002/14651858.CD001139.pub4.
- Albert HB, Godskesen M, Westergaard JG. Incidence of four syndromes of pregnancy-related pelvic joint pain. Spine (Phila Pa 1976). 2002;27(24):2831-4. Available from: https://doi.org/10.1097/00007632-200212150-00020.
- Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J. 2008;17(6):794-819. Available from: https://doi.org/10.1007/s00586-008-0602-4.
- Elden H, Lundgren I, Robertson E. Life's pregnant pause of pain: pregnant women's experiences of pelvic girdle pain related to daily life: a Swedish interview study. Sex Reprod Healthc. 2013;4(1):29-34. Available from: https://doi.org/10.1016/j.srhc.2012.11.003.
- Mackenzie J, Murray E, Lusher J. Women's experiences of pregnancy related pelvic girdle pain: A systematic review. Midwifery. 2018;56:102-11. Available from: https://doi.org/10.1016/j.midw.2017.10.011.
- Albert H, Godskesen M, Westergaard J. Prognosis in four syndromes of pregnancy-related pelvic pain. Acta Obstet Gynecol Scand. 2001;80(6):505-10.
- Elden H, Gutke A, Kjellby-Wendt G, Fagevik-Olsen M, Ostgaard HC. Predictors and consequences of long-term pregnancy-related pelvic girdle pain: a longitudinal follow-up study. BMC Musculoskelet Disord. 2016;17:276. Available from: https://doi.org/10.1186/s12891-016-1154-0.
- Gutke A, Lundberg M, Ostgaard HC, Oberg B. Impact of postpartum lumbopelvic pain on disability, pain intensity, health-related quality of life, activity level, kinesiophobia, and depressive symptoms. Eur Spine J. 2011;20(3):440-8. Available from: https://doi.org/10.1007/s00586-010-1487-6.
- Leadbetter RE, Mawer D, Lindow SW. Symphysis pubis dysfunction: a review of the literature. J Matern Fetal Neonatal Med. 2004;16(6):349-54. Available from: https://doi.org/10.1080/jmf.16.6.349.354.
- Wuytack F, Begley C, Daly D. Risk factors for pregnancy-related pelvic girdle pain: a scoping review. BMC Pregnancy Childbirth. 2020;20(1):739. Available from: https://doi.org/10.1186/s12884-020-03442-5.
- Gutke A, Boissonnault J, Brook G, Stuge B. The Severity and Impact of Pelvic Girdle Pain and Low-Back Pain in Pregnancy: A Multinational Study. J Womens Health (Larchmt). 2018;27(4):510-7. Available from: https://doi.org/10.1089/jwh.2017.6342.

 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services
 Share on Facebook
Share on Facebook
 Share on LinkedIn
Share on LinkedIn
 Share via Email
Share via Email