Psychological and psychosocial interventions in forensic psychiatric care
A systematic review and assessment of medical, economic, social and ethical aspects
Aim
The conditions for psychological and psychosocial interventions within forensic psychiatric care differ in many ways from non-compulsory psychiatry. This project focuses on the benefits and risks of interventions used in forensic psychiatry, including their health economic and ethical aspects, and the experiences of patients who have been remitted to forensic psychiatric care. The assignment to evaluate interventions in forensic psychiatric care came from The Ministry of Health and Social Affairs. An earlier mapping of systematic reviews pertaining to interventions used in forensic psychiatry (SBU 2017) indicate a substantial need for well conducted research.
Conclusions
- The effects of psychological and psychosocial interventions used in forensic psychiatric settings need to be explored. Only a few studies of psychological interventions that had been adjusted for forensic psychiatric settings were identified. The studies were heterogenous, examining various interventions and providing different outcomes. There is insufficient data to draw any conclusions about the effects of the interventions. No studies on psychosocial interventions were identified. Many of the interventions currently being used in forensic psychiatry were developed for other care settings, but their usability and efficacity may be influenced by the fact that, in contrast to treatment in open psychiatry, forensic psychiatric care is compulsory and that patients treated in forensic psychiatric care are more likely to have multiple concurrent diagnoses.
- The costs associated with psychological interventions are very low compared to the total cost of care. Therefore, interventions which shorten the time spent in forensic psychiatric care would very likely be cost effective.
- Obtaining more understanding is urgent from an ethical point of view. Forensic psychiatric care is an extensive and often prolonged encroachment on an individual’s life and autonomy. That we do not know if the treatments being provided are effective creates a particularly problematic ethical dilemma.
- Increased coordination of research in this field could provide more reliable information by permitting larger studies with more homogeneous interventions and outcomes to be conducted. In the last few years, some studies have been conducted on interventions adapted for patients in forensic psychiatric settings.
- There is a need for research that can support the development of healthcare in forensic psychiatric care. Interview studies from Swedish forensic psychiatric care settings indicate that patients often feel exposed and vulnerable.
- The goals defined in healthcare legislation about care on equal terms points to the need for a more uniform forensic psychiatric care. Interventions must be based on a scientific evidence.
- Forensic psychiatric care varies considerably throughout Sweden. An inventory of current practices shows that clinics differ substantially in which interventions they provide. Many of the interventions were locally developed and lack scientific ground and systematic follow-up. The ability to offer alternative treatments also varies.
What are the implications?
These results demonstrate that there is a large need for research that can support the development of psychological and psychosocial interventions, as well as general healthcare and nursing, and help to improve how patients are met in forensic psychiatric care. The results also indicate that the way forensic psychiatry is conducted varies throughout Sweden.
Background
Severe psychiatric illness is a legal term rather than a medical term. In Sweden, a person who commits a crime when they have an active severe psychiatric illness can be sentenced to receive forensic psychiatric care rather than incarceration. Approximately 300 individuals are remitted to forensic psychiatric care each year.
Forensic psychiatric care is regulated in part by the same laws that regulate all Swedish healthcare and in part by penal laws. Patients remitted to forensic psychiatric care have diverse diagnoses and the most common diagnosis is psychosis. Autism and personality disorders are also common. These patients often have a substantial need for healthcare. The care provided by forensic psychiatry resembles the care provided by other psychiatric care providers, often using the same treatments.
Method
The project was conducted in accordance to the methods of SBU. This assessment consists of three systematic reviews. The first assessed the effects of psychological treatments and psychosocial interventions examined in controlled studies that were conducted in forensic psychiatric settings and considered transferable to the Swedish system. The second assessed the qualitative evidence regarding the experiences of patients remitted to forensic psychiatric care in Sweden. The third was a systematic review of health economic assessments; this was complemented with cost information associated with interventions, the over-all care and the legal process in the Swedish system. The systematic reviews were complemented with a survey of current clinical practices used in Swedish forensic psychiatric care and an ethical evaluation.
Main results
Five studies of effects of treatment met the inclusion criteria for the systematic review on psychological treatments and psychosocial interventions. All were cognitive behavioral therapies that had been adapted for use in forensic psychiatric settings. The studies were too heterogenous in treatment and outcome to allow meta-analysis. No studies on psychosocial interventions were identified.
Four qualitative studies on patient experiences from Swedish forensic psychiatry were identified. The studies suggest that these patients often feel vulnerable, that they lack autonomy and adequate influence over their care.
No economic evaluations which meet the inclusion criteria for the project were identified. The systematic review was complemented with an assessment of the related costs in Sweden that showed that the costs of interventions are very low in relation to the total cost of forensic psychiatric care.
Discussion
Our assessment of psychological treatments and psychosocial interventions clearly indicates a lack of research in forensic psychiatric care; there are few effect studies in the field. It is promising that more interventions have been adapted for this population in the last few years, and that research into their efficacity has begun.
It should be noted that the lack of research does not imply that an intervention lacks effect, but rather that its effect has not been sufficiently researched.
Other aspects of care and how patients are treated in forensic psychiatry are also important for patient recovery. Initiatives to develop this work should be encouraged. Psychological treatments, psychosocial interventions, and general healthcare together with pharmacological treatment are all important elements of forensic psychiatric care; they depend on each other to achieve the best results.
The full report in Swedish
The full report in Swedish Psykologiska behandlingar och psykosociala insatser i rättspsykiatrisk vård
Project group
Experts
- Malin Lotterberg (literature review, analysis and report)
- Björn Hofvander (literature review, analysis and report)
- Ulf Axberg (analysis and report)
- Susanna Radovic (ethics)
SBU
- Alexandra Snellman (Project Manager)
- Mikael Nilsson (Assistant Project Manager)
- Nathalie Peira (Assistant Project Manager)
- Emin Hoxha Ekström (Health Economist)
- Kickan Håkanson (Project Administrator)
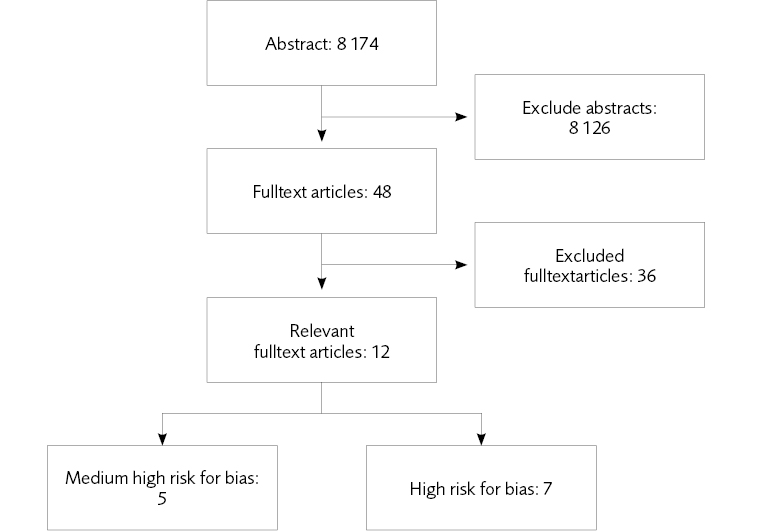
Flow charts
References
- SBU. Behandling och bedömning i rättspsykiatrisk vård. En kartläggningav systematiska översikter. Stockholm:Statens beredning för medicinskoch social utvärdering (SBU); 2017.SBU-rapport nr 264. ISBN 978-9188437-06-8.
- SBU. Läkemedelsbehandling inom rättspsykiatrisk vård. En systematisköversikt och utvärdering av medicinska,hälsoekonomiska, sociala och etiskaaspekter. Stockholm: Statens beredningför medicinsk och social utvärdering(SBU); 2018. SBU-rapport nr 286. ISBN 978-91-88437-28-0.
- Lidberg L, Wiklund N. Svensk rättspsykiatri: psykisk störning, brott och påföljd. Studentlitteratur AB; 2004: sid 136. ISBN: 9789144037042.
- SBU. Utvärdering av metoder i hälsooch sjukvården. En handbok, 2 uppl. Stockholm 2014. http://www.sbu.se/metodbok.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ2008;336:924-6.
- Fontanarosa J, Uhl S, Oyesanmi O, Schoelles KM. Interventions for adult offenders with serious mental illness. Rockville (MD): Agency for Healthcare Research and Quality (US); 2013 Aug. Report No.: 13-EHC107-EF. AHRQ Comparative Effectiveness Reviews.
- Vetenskapsrådet. Kartläggning av rättspsykiatrisk forskning, 2017. ISBN: 978-91-7307-349-3.
- Uppdrag Psykisk Hälsa, Avdelningen Vård och omsorg, Sveriges Kommuner och Landsting, 2018. Vårdens innehåll i rättspsykiatrin – kartläggning2017.
- Nationellt rättspsykiatriskt kvalitetsregister (RättspsyK). Årsrapport 2016. Tryckår 2017. ISSN 2001-3698.
- Kartläggning 2016. Rättspsykiatri. En kartläggning gjord av Helseplan Nysam. Uppdrag Psykisk Hälsa, Sveriges Kommuner och Landsting2017.
- Aho-Mustonen K, Tiihonen J, RepoTiihonen E, Ryynänen OP, Miettinen R, Räty H. Group psychoeducation for long-term offender patients with schizophrenia: an exploratory randomisedpsykologiska behandlingar och psykosociala insatser i rättspsykiatrisk vård 82 controlled trial. Crim Behav Ment Health 2011;21:163-76.
- Cavezza C, Aurora M, Ogloff JRP. The effects of an adherence therapy approach in a secure forensic hospital: A randomised controlled trial. J Forens Psychiatry Psychol 2013;24:458-78.
- Yip V, Gudjonsson GH, Perkins D, Doidge A, Hopkin G, Young S. Anon-randomised controlled trial ofthe R&R2MHP cognitive skills program in high risk male offenders with severe mental illness. BMC Psychiatry2013;13:267-67.
- Kuokkanen R, Lappalainen R, RepoTiihonen E, Tiihonen J. Metacognitive group training for forensic and dangerous non-forensic patients with schizophrenia:a randomised controlled feasibility trial. Crim Behav Ment Health 2014;24:345-57.
- Walker H, Tulloch L, Ramm M, Drysdale E, Steel A, Martin C, et al. A randomised controlled trial to explore insight into psychosis; Effects of a psychoeducation programme on insight in aforensic population. J Forens Psychiatry Psychol 2013;24:756-71.
- Tomlinson MF, Hoaken PNS. The potential for a skills-based dialectical behavior therapy program to reduce aggression, anger, and hostility in a Canadian forensic psychiatric sample:A pilot study. Int J Forensic Ment Health 2017;16:215-26.
- Tyler N, Gannon TA, Lockerbie L, Ó Ciardha C. An evaluation of a specialist firesetting treatment programme formale and female mentally disorderedoffenders (the FIP-MO). Clin Psychol Psychother 2017;1-13.
- Walker H, Connaughton J, Wilson I, Martin CR. Improving outcomes for psychoses through the use of psychoeducation; preliminary findings.J Psychiatr Ment Health Nurs 2012; 19:881-90.
- Jotangia A, Rees-Jones A, Gudjonsson GH, Young S. A multi-site controlledtrial of the R&R2MHP cognitive skills program for mentally disordered female offenders. Int J Offender TherComp Crimino l 2015;59:539-59.
- Cullen AE, Clarke AY, Kuipers E, Hodgins S, Dean K, Fahy T. A multisite randomized trial of a cognitive skills program for male mentally disordered offenders: violence and antisocial behavior outcomes. J Consult Clin Psychol 2012;80: 1114-20.
- Clarke AY, Cullen AE, Walwyn R, Fahy T. A quasi-experimental pilot study of the reasoning and rehabilitation programme with mentally disordered offenders. J Forens Psychiatry Psychol 2010;21:490-500.
- Williams E, Ferrito M, Tapp J. Cognitive-behavioural therapy for schizophrenia in a forensic mental health setting. Journal of Forensic Practice 2014;16:68-77.
- Ross RR, Fabiano EA, Ross RD. Reasoning & Rehabilitation: A handbook for teaching cognitive skills. Ottawa: Cognive Centre of Canada, University of Ottawa, 1986.
- Behandlingsprogrammet ETS i Kriminalvården. Utvärdering av återfall i brott för programdeltagare 2004-2009. Maria Danielsson, Axel Fors, Ingrid Freij, 2012. ISBN: 978-91-86903-07-7. Hemsida: www.kriminalvarden.se/publikationer.
- Moritz S, Woodward TS. Metacognitive training in schizophrenia: from basic research to knowledge translation and intervention. Curr Opin Psychiatry 2007;20:619-25.
- Higgins J, Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from http://handbook.cochrane.org.
- Raboch J, Kalisova L, Nawka A, Kitzlerova E, Onchev G, Karastergiou A, et al. Use of coercive measures during involuntary hospitalization: findings from ten European countries. PsychiatrServ 2010;61:1012-7.
- Hörberg U, Sjögren R, Dahlberg K. To be strategically struggling against resignation: the lived experience of being cared for in forensic psychiatric care. Issues Ment Health Nurs 2012;33:743-51.
- Olsson H, Audulv A, Strand S, Kristiansen L. Reducing or increasing violence in forensic care:a qualitative study of inpatient experiences. Arch Psychiatr Nurs 2015;29:393-400.
- Selvin M, Almqvist K, Kjellin L, Schroder A. The concept of patient participation in forensic psychiatric care: The patient perspective. J Forensic Nurs 2016;12:57-63.
- Olsson H, Strand S, Kristiansen L. Reaching a turning point--how patients in forensic care describe trajectories of recovery. Scand J Caring Sci 2014;28:505-14.
- Doyle P, Quayle E, Newman E. Social climate in forensic mental health settings: A systematic review of qualitativestudies. Aggress Violent Behav 2017;36:118-136.
- Shepherd A, Doyle M, Sanders C, Shaw J. Personal recovery within forensic settings--Systematic review and meta-synthesis of qualitative methods studies. Crim Behav MentHealth 2016;26:59-75.
- Statistiska centralbyrån (SCB). Lönestatistik 2017. https://www.scb.se/hitta-statistik/sverige-i-siffror/lonesok/
- Kriminalvården. Årsredovisning2017. https://www.kriminalvarden.se/globalassets/publikationer/ekonomi/kriminalvardens-arsredovisning-2017.pdf
- Brottsförebyggande rådet (BRÅ). Att minska isolering i häkte – Lägesbild och förslag. Rapport 2017:6. ISBN978-91-87335-83-9.
- Åklagarmyndigheten. Årsredovisning 2017. https://www.aklagare.se/globalassets/dokument/planeringoch-uppfoljning/arsredovisningar/arsredovisning-2017.pdf
- Rättsmedicinalverket. Årsredovisning 2017. Dnr X17-90134. https://www.rmv.se/wp-content/uploads/arsredovisning2017tillganglighetsanpassad.pdf
- Sveriges domstolar. Årsredovisning 2017. http://www.domstol.se/Publikationer/Arsredovisning/arsredovisning_2017_sverigesdomstolar.pdf
- Naionellt rättspsykiatriskt kvalitetsregister (RättspsyK). Årsrapport 2017. Tryckår 2018. ISSN 2001-3698.
- SBU. Etiska aspekter på åtgärder inom hälso- och sjukvården. Reviderad 2014. Statens beredning för medicinsk och social utvärdering (SBU). Tillgänglig från http://www.sbu.se/globalassets/ebm/metodbok/mall_etiska_aspekter.pdf
- Adshead G, Davies T. Wise restraints: ethical issues in the coercion of forensic patients. In Völlm B, Nedopil N (red). The use of coercive measures in forensic psychiatric care: Legal, ethical and practical challenges. Springer International Publishing 2016. ISBN 3319267485, 9783319267487.
- Adshead G. Care or custody? Ethical dilemmas in forensic psychiatry. J Med Ethics 2000;26:302-04.
- Maruna S. Making good: How exconvicts reform and rebuild their lives. Washington, DC, American Psychological Association 2001. ISBN: 978-1-55798-731-0.
- Socialstyrelsen. Innehållet i den rättspsykiatriska vården – Delrapport till Nationell psykiatrisamordning, 2009. 5:12 Psykologiska behandlingsmetoder.
- Cislo AM, Trestman R. Challenges and solutions for conducting research in correctional settings: the U.S. experience. Int J Law Psychiatry 2013;36:304-10.
- Moser DJ, Arndt S, Kanz JE, Benjamin ML, Bayless JD, Reese RL, et al. Coercion and informed consent in research involving prisoners. Compr Psychiatry 2004;45:1-9.
- World Medical Association (WMA). WMA declaration of Helsinki – ethical principles for medical research involving human subjects. https://www.wma.net/policies-post/wma-declaration-ofhelsinki-ethical-principles-for-medicalresearch-involving-human-subjects/
- Weisburd D. Ethical practice and evaluation of interventions in crime and justice The moral imperative for randomized trials. Eval Rev 2003:27:336-54.
- Gabor T. Costs of crime and criminal justice responses. Research report: psykologiska behandlingar och psykosociala insatser i rättspsykiatrisk vård 84 2015-R022. Research Division, Public Safety Canada, Ottawa, Ontario. ISBN: 978-0-660-03409-6
- McCollister K, French M, Fang H. The cost of crime to society: new crime-specific estimates for policy and program evaluation. Drug Alcohol Depend 2010;108:98-109.
- Dolan P, Loomes G, Peasgood T, Tsuchiya A. Estimating the intangible victim costs of violent crime. Br J Criminol 2005;45:958-76.
- Kisely SR, Campbell LA, Preston NJ. Compulsory community and involuntary outpatient treatment for people with severe mental disorders. Cochrane Database Syst Rev 2011; Feb 16;(2):CD004408.
- Hopkin G, Evans-Lacko, S, Forrester, A, Shaw, J, Thornicroft, G. Interventions at the transition from prison to the community for prisoners with mental illness: A systematic review. Adm Policy Ment Health 2018 Jan 23. doi:10.1007/ s10488-018-0848-z.

 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services
 Share on Facebook
Share on Facebook
 Share on LinkedIn
Share on LinkedIn
 Share via Email
Share via Email