Treatment for binge eating disorder
A systematic review and assessment of the medical, economic, social and ethical aspects
Binge eating disorder (BED) is a new formal diagnosis in DSM-5, although it has been defined in previous version of the DSM since 1994 as a research category, and used in clinical settings for nearly 20 years. The aim of this systematic review was to evaluate the efficacy of treatments for BED.
Aim
Binge eating disorder (BED) is a new formal diagnosis in DSM-5, although it has been defined in previous version of the DSM since 1994 as a research category, and used in clinical settings for nearly 20 years. The aim of this systematic review was to evaluate the efficacy of treatments for BED.
Conclusions
- Several different treatments for BED result in remission (defined as cessation of binge episodes) or decreased frequency of binge eating episodes.
- Both CBT and IPT result in remission, or decreased frequency of binge eating episodes up to one year after end of treatment. No conclusions are presented for follow ups beyond one year due to few studies. At end of treatment, guided self-help, based on CBT, results in remission and decreased frequency of binge eating episodes.
- SSRI and lisdexamfetamine result in remission and decreased frequency of binge eating episodes at end of treatment. The effect of psychopharmacology beyond the end of treatment is unknown.
- Future research should investigate the long term and adverse effects, cost-effectiveness, the effect of treatments for children and adolescents, and the effect of treatments on quality of life.
Background
Binge eating disorder is associated with psychological and physical suffering and is perceived as shameful by those with the condition. The diagnostic criteria for BED include recurrent episodes of binge eating associated with at least three of the following; eating much more rapidly than normal, eating until feeling uncomfortably full, eating large amounts of food when not feeling physically hungry, eating alone because of embarrassment, and/or feeling disgusted with oneself, depressed or very guilty after overeating. BED is similar to Bulimia Nervosa regarding the binge eating episodes but does not involve purging, or other compensatory behaviours. In contrast to other eating disorders a considerable proportion of individuals with BED are overweight or obese.
In the general population, 1–4% are estimated to meet criteria for BED. The lifetime comorbidity with other psychiatric disorders is estimated to 70%. Many individuals with BED never seek treatment and those who do wait approximately between 10 to 19 years.
Method
The systematic review was conducted according to the PRISMA statement. Inclusion criteria were individuals with binge eating disorder (full or subthreshold) and psychological, behavioural, pharmacological, and combination interventions. Controlled clinical studies, with and without randomization were included. Five different databases were searched until November 2015. The methodological quality of eligible studies was assessed and only studies with moderate or low risk of bias were included in the analysis. GRADE was used to evaluate the certainty/quality of the evidence (strong (![]() ), moderate (
), moderate (![]() ), low (
), low (![]() ) and very low (
) and very low (![]() )).
)).
Main results
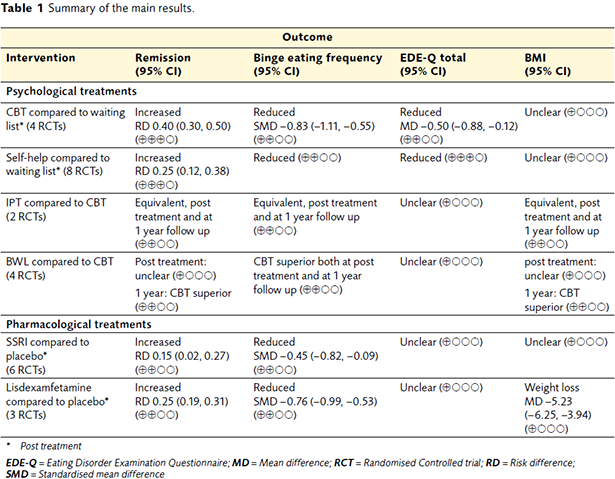
Altogether 44 studies in 53 publications were identified fulfilling inclusion and quality criteria. All were randomized. Approximately half of them could be included in a meta-analysis. We found evidence for several interventions for the short-term outcome of binge eating disorder (i.e. post-treatment outcome). The main results are presented in Table 1. There was a lack of cost analyses in these studies.
Table 1 Summary of the main results.
Consequences
The conclusion from this systematic review is that there are several different treatments that are effective for BED. However, the long-term effect is unknown for most of the interventions since the majority of the studies only analysed effects post treatment, except for CBT and IPT.
Psychological therapy may be more effective than pharmacologic but no direct comparison has been done. Indirect comparisons are difficult since studies have used either waiting list or placebo as control condition.
With respect to pharmacological treatments, the adverse effects associated with SSRI and lisdexamfetamine described for other disorders are also present for persons with BED. The risk for adverse events from psychological treatments is unknown. No studies reported any adverse events but it is unclear whether this was systematically investigated.
Despite the fact that patients with BED are known to have reduced quality of life, most studies had not evaluated if this was improved or changed after the treatment. In addition, health economic studies are lacking.
How to cite this report: SBU. Treatment for binge eating disorder. Stockholm: Swedish Agency for Health Technology Assessment and Assessment of Social Services (SBU); 2016. SBU report no 248 (in Swedish).
More on the subject
Scientific article
Ghaderi A, Odeberg J, Gustafsson S, Råstam M, Brolund A, Pettersson A, et al. Psychological, pharmacological, and combined treatments for binge eating disorder: a systematic review and meta-analysis. PeerJ. 2018;6:e5113. Open access

 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services
 Share on Facebook
Share on Facebook
 Share on LinkedIn
Share on LinkedIn
 Share via Email
Share via Email