Dialectical Behaviour Therapy (DBT) and Mentalization-Based Therapy (MBT)
A systematic review regarding the effects of DBT and MBT in patients with self-harming behaviour without a diagnosis of BPD, in patients with bulimia or binge eating disorder, and effects of short versions of DBT and MBT.
Conclusion
Effects in diagnoses other than BPD:
- DBT has a better effect than usual carea on several important symptoms and self-destructive behaviours in children and adolescents with self-harming behaviour that do not meet the diagnostic criteria for BPD.
Effects of treatment with short versions of DBT:
- Shorter versions of DBT have a better effect than both waiting list and other structured treatmentb on several important symptoms and self-destructive behaviours in adults with BPD, and in adults with binge eating disorder or bulimia.
Key knowledge gaps:
- Due to the lack of studies that meet our inclusion criteria, we conclude that the following effects remain unknown for:
- All forms of MBT in patients with self-harming behaviour that do not meet the criteria for BPD, as well as in patients with binge eating disorder or bulimia.
- Shorter versions of MBT on all of the populations included in this review.
- All forms of DBT for adults with self-harming behaviour that do not meet the criteria for BPD.
- As a vast majority of the participants in the included studies are female, more studies are needed on boys and men with these difficulties.
- Usual care refers to several different treatments that are given in an unstructured way to the control group, even if the different treatments are structured in their own right.
- Other structured treatment refers to specific treatment that is given in the same structured way to the entire control group
Background
Dialectical Behaviour Therapy (DBT) and Mentalization-Based Therapy (MBT) are interventions that originally were developed for patients with Borderline Personlity Disorder (BPD). The interventions have later been evaluated and used in patients with other diagnoses than BPD, for instance self-harm, suicidal behaviour, and eating disorders. The original versions of the treatments are extensive interventions, designed with individual as well as group therapy. Later, shorter versions of the treatments have been developed that for instance focus on either group or individual therapy. Especially the versions that focus on group therapy are used to some extent in clinical practice today.
Aim
The purpose of this systematic review was to evaluate the scientific support for two questions:
- What are the effects of DBT and MBT in the treatment of:
- patients with self-harming behaviour that do not meet the criteria for BPD
- patients with binge eating disorder or bulimia?
- What are the effects of shorter versions of DBT and MBT, for instance versions solely focusing on group therapy?
Method
We conducted a systematic review and reported int in accordance with the PRISMA statement. The protocol is registered in Prospero (CRD42023459707). Meta-analyses were performed on extracted data from included studies using the inverse variance method and the random effects model in Review Manager 5.4.1 at the end of treatment and at the end of follow-up, respectively. The certainty of the evidence was assessed with GRADE.
Results
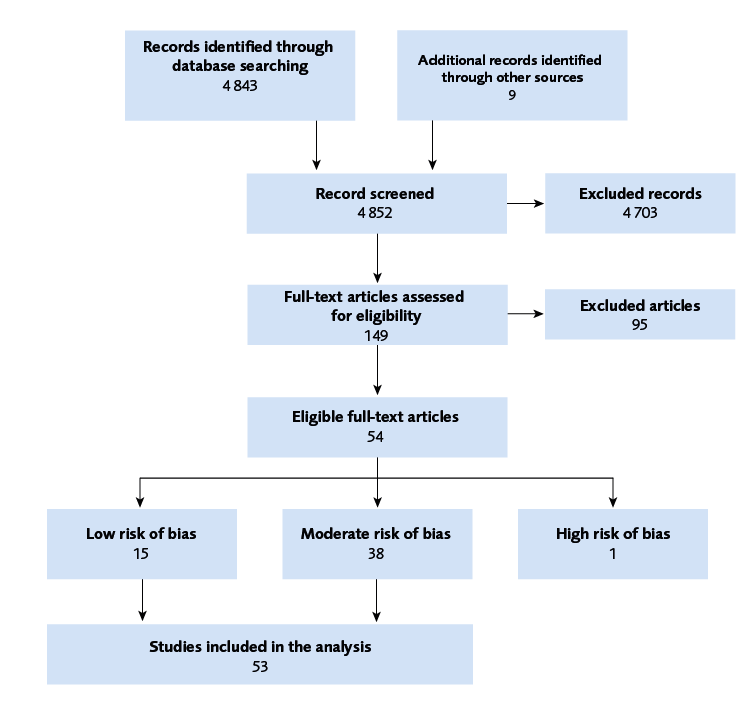
A systematic literature search was conducted in February 2024. The results of this review is based on 53 publications from 42 randomized and controlled studies (Figure 1). Due to multiple populations, interventions, comparisons and outcomes (Table 1), a great number of results from meta-analyses were obtained. As a result of active control treatments and the fact that several of the results from the meta-analyses were based on relatively small number of studies and patients, many results were assessed as a very low level of certainty according to GRADE. None the less, for certain populations, interventions and outcomes, several results were assessed a low, moderate or high level of certainty according to GRADE (Table 2).
Most of the participants in the studies were women. However, the results of existing studies on men do not contradict the results of this review.
Discussion
DBT is a comprehensive and costly treatment. This review concludes that short versions of DBT have an effect on certain outcomes in certain patient populations, and these shorter interventions may be considered if access to treatment needs to be increased and extensive DBT is not fully available.
The results also indicate that DBT in various forms has an effect in at least two populations where the majority of the individuals do not meet the criteria for BPD.
More studies are needed to better understand which patient groups respond to different forms of these treatments. This is especially the case for short versions of MBT, and for MBT in general for patients with other diagnoses than BPD.
| Population | Adults, adolescents and children with Borderline personality disorder (BPD), self-harm and/or suicidal behaviour without BPD, binge-eating disorder or bulimia |
| Intervention | DBT and MBT. Results for the original versions of the interventions, and the shorter versions of the interventions were reported separately |
| Control | Other structured treatment, usual care, waiting list, no intervention |
| Outcome | Severity of BPD, self-harming behaviour, episodes of self-harm, suicidal thoughts, suicide attempts, suicide, suicidal gestures, deviant eating behaviours, binge eating episodes, eating disorder-specific psychopathology, vomiting, other compensatory behaviours, emotion regulation, psychosocial functioning, relationship difficulties, mentalization ability, depression, anxiety and negative side effects |
| Abbreviations: BED (Binge-eating disorder), BN (bulimia nervosa), DBT (Dialectical behaviour therapy) DBT-I (DBT-Individual, short version of DBT that focuses on individual therapy), DBT-ST (DBT skills training, short version of DBT that focuses on skills training in group), BPD (Borderline personality disorder), EOF (End of follow-up), EOT (End of treatment), MBT (Mentalization based therapy), OST (Other structured treatment), SH (Self-harm), SB (Suicidal behaviour), TAU (Treatment as usual), WL/NI (Wait list/no intervention). | ||||||
| Population with BPD | Intervention | Control | EOT | EOF | No of studies | Participants |
|---|---|---|---|---|---|---|
| Children and adolescents | MBT | TAU | 0/5 | 0/5 | 2 | 192 |
| Adults | DBT | TAU | 8/14 | 5/11 | 10 | 570 |
| OST | 4/10 | 0/6 | 4 | 430 | ||
| DBT-ST | WL/NI | 4/6 | 3/5 | 3 | 153 | |
| TAU | 0/2 | − | 1 | 41 | ||
| OST | 2/11 | 1/11 | 6 | 361 | ||
| MBT | OST | 3/11 | 5/10 | 7 | 544 | |
| Population without BPD | Intervention | Control | EOT | EOF | No of studies | Participants |
| Children and adolescents with SH/SB | DBT | TAU | 3/8 | 1/7 | 2 | 112 |
| Adults with BED/BN | DBT | OST | 0/5 | 0/5 | 1 | 67 |
| DBT-ST | WL/NI | 5/8 | − | 4 | 176 | |
| OST | 3/8 | 1/7 | 2 | 137 | ||
| DBT-I | WL/NI | 4/8 | − | 2 | 89 | |
Conflict of Interest
In accordance with SBU’s requirements, the experts and scientific reviewers participating in this project have submitted statements about conflicts of interest. These documents are available upon request from SBU. SBU has determined that the conditions described in the submissions are compatible with SBU’s requirements for objectivity and impartiality.
The full report in Swedish
Dialektisk beteendeterapi (DBT) och Mentaliseringsbaserad terapi (MBT)
Project group
Experts
- Pia Enebrink, Associate professor, Senior lecture
- Hanna Sahlin, Associate professor, Program director
SBU
- Jonatan Alvan, Project director
- Mikael Nilsson, Assistant project director
- Emma Wernersson, Project administrator
- Maja Kärrman-Fredriksson, Information specialist
Flow chart
References
- Bateman A, Fonagy P. Mentalization-Based Treatment. Psychoanal Inq. 2013;33(6):595-613. Available from: http://10.1080/07351690.2013.835170.
- Tate AE, Sahlin H, Liu S, Lu Y, Lundström S, Larsson H, et al. Borderline personality disorder: associations with psychiatric disorders, somatic illnesses, trauma, and adverse behaviors. Molecular Psychiatry. 2022;27(5):2514-21. Available from: https://doi.org/10.1038/s41380-022-01503-z.
- Dehlbom P, Wetterborg D, Lundqvist D, Maurex L, Dal H, Dalman C, et al. Gender differences in the treatment of patients with borderline personality disorder. Personal Disord. 2022;13(3):277-87. Available from: https://doi.org/10.1037/per0000507.
- Grant BF, Chou SP, Goldstein RB, Huang B, Stinson FS, Saha TD, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533-45. Available from: https://doi.org/10.4088/jcp.v69n0404.
- Gunderson JG, Stout RL, McGlashan TH, Shea MT, Morey LC, Grilo CM, et al. Ten-year course of borderline personality disorder: psychopathology and function from the Collaborative Longitudinal Personality Disorders study. Arch Gen Psychiatry. 2011;68(8):827-37. Available from: https://doi.org/10.1001/archgenpsychiatry.2011.37.
- Storebø OJ, Stoffers-Winterling JM, Völlm BA, Kongerslev MT, Mattivi JT, Jørgensen MS, et al. Psychological therapies for people with borderline personality disorder. Cochrane Database of Systematic Reviews. 2020(5). Available from: https://doi.org/10.1002/14651858.CD012955.pub2.
- Holah S, Maguire N, Bennetts A. Dialectical behaviour therapy for men and boys: A systematic review. Counselling and Psychotherapy Research. 2024;24(2):652-65. Available from: https://doi.org/10.1002/capr.12702.
- Sansone RA, Sansone LA. Gender patterns in borderline personality disorder. Innov Clin Neurosci. 2011;8(5):16-20.
- Mehlum L, Tormoen AJ, Ramberg M, Haga E, Diep LM, Laberg S, et al. Dialectical behavior therapy for adolescents with repeated suicidal and self-harming behavior: a randomized trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2014;53(10):1082-91. Available from: https://dx.doi.org/10.1016/j.jaac.2014.07.003.
- Zanarini MC, Temes CM, Magni LR, Fitzmaurice GM, Aguirre BA, Goodman M. Prevalence rates of borderline symptoms reported by adolescent inpatients with BPD, psychiatrically healthy adolescents and adult inpatients with BPD. Personal Ment Health. 2017;11(3):150-6. Available from: https://doi.org/10.1002/pmh.1378.
- Blaha Y, Cavelti M, Lerch S, Steinhoff A, Koenig J, Kaess M. Risk-taking and self-harm behaviors as markers of adolescent borderline personality disorder. European Child & Adolescent Psychiatry. 2024. Available from: https://doi.org/10.1007/s00787-023-02353-y.
- Kaess M, Brunner R, Chanen A. Borderline Personality Disorder in Adolescence. Pediatrics. 2014;134(4):782-93. Available from: https://doi.org/10.1542/peds.2013-3677.
- Turner BJ, Dixon-Gordon KL, Austin SB, Rodriguez MA, Zachary Rosenthal M, Chapman AL. Non-suicidal self-injury with and without borderline personality disorder: Differences in self-injury and diagnostic comorbidity. Psychiatry Research. 2015;230(1):28-35. Available from: https://doi.org/10.1016/j.psychres.2015.07.058.
- Andover MS, Morris BW. Expanding and clarifying the role of emotion regulation in nonsuicidal self-injury. Can J Psychiatry. 2014;59(11):569-75. Available from: https://doi.org/10.1177/070674371405901102.
- Swannell SV, Martin GE, Page A, Hasking P, St John NJ. Prevalence of Nonsuicidal Self-Injury in Nonclinical Samples: Systematic Review, Meta-Analysis and Meta-Regression. Suicide and Life-Threatening Behavior. 2014;44(3):273-303. Available from: https://doi.org/10.1111/sltb.12070.
- Ose SO, Tveit T, Mehlum L. Non-suicidal self-injury (NSSI) in adult psychiatric outpatients – A nationwide study. Journal of Psychiatric Research. 2021;133:1-9. Available from: https://doi.org/10.1016/j.jpsychires.2020.11.031.
- Gillies D, Christou MA, Dixon AC, Featherston OJ, Rapti I, Garcia-Anguita A, et al. Prevalence and Characteristics of Self-Harm in Adolescents: Meta-Analyses of Community-Based Studies 1990-2015. J Am Acad Child Adolesc Psychiatry. 2018;57(10):733-41. Available from: https://doi.org/10.1016/j.jaac.2018.06.018.
- Farkas BF, Takacs ZK, Kollárovics N, Balázs J. The prevalence of self-injury in adolescence: a systematic review and meta-analysis. Eur Child Adolesc Psychiatry. 2023. Available from: https://doi.org/10.1007/s00787-023-02264-y.
- Jacobson CM, Muehlenkamp JJ, Miller AL, Turner JB. Psychiatric impairment among adolescents engaging in different types of deliberate self-harm. J Clin Child Adolesc Psychol. 2008;37(2):363-75. Available from: https://doi.org/10.1080/15374410801955771.
- Gratz KL. Measurement of Deliberate Self-Harm: Preliminary Data on the Deliberate Self-Harm Inventory. Journal of Psychopathology and Behavioral Assessment. 2001;23(4):253-63. Available from: https://doi.org/10.1023/A:1012779403943.
- Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: long-term follow-up of patients who presented to a general hospital. Br J Psychiatry. 2003;182:537-42. Available from: https://doi.org/10.1192/bjp.182.6.537.
- Glenn CR, Klonsky ED. Nonsuicidal self-injury disorder: an empirical investigation in adolescent psychiatric patients. J Clin Child Adolesc Psychol. 2013;42(4):496-507. Available from: https://doi.org/10.1080/15374416.2013.794699.
- Socialstyrelsen. Ökning av nya fall av avsiktlig självdestruktiv handling bland flickor under pandemiåret 2021. Stockholm: Socialstyrelsen; 2022. [accessed Juli 8 2024]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2022-10-8154.pdf.
- Beckman K, Mittendorfer-Rutz E, Lichtenstein P, Larsson H, Almqvist C, Runeson B, et al. Mental illness and suicide after self-harm among young adults: long-term follow-up of self-harm patients, admitted to hospital care, in a national cohort. Psychol Med. 2016;46(16):3397-405. Available from: https://doi.org/10.1017/s0033291716002282.
- Socialstyrelsen. Sjukhusvård och eftervård vid avsiktlig självskada. Stockholm: Socialstyrelsen; 2023. [accessed Juli 8 2024]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2023-1-8338.pdf.
- Favril L, Yu R, Geddes JR, Fazel S. Individual-level risk factors for suicide mortality in the general population: an umbrella review. The Lancet Public Health. 2023;8(11):e868-e77. Available from: https://doi.org/10.1016/S2468-2667(23)00207-4.
- Harmer B, Lee S, Rizvi A, Saadabadi A. Suicidal Ideation. In: StatPearls. Treasure Island (FL): StatPearls Publishing Copyright © 2024, StatPearls Publishing LLC.; 2024.
- Diagnostic and statistical manual of mental disorders: DSM-5™, 5th ed. Arlington, VA, US: American Psychiatric Publishing, Inc.; 2013. xliv, 947-xliv, p.
- ICD-11: International classification of diseases (11th revision). World Helath Organization (WHO); 2022. [accessed Sept 24 2024]. Available from: https://icd.who.int/en.
- Quadflieg N, Voderholzer U, Meule A, Fichter MM. Comparing ICD-11 and DSM-5 eating disorder diagnoses with the Munich eating and feeding disorder questionnaire (ED-Quest). International Journal of Eating Disorders. 2023;56(9):1826-31. Available from: https://doi.org/10.3390/nu15194247.
- Wilson GT, Fairburn CC, Agras WS, Walsh BT, Kraemer H. Cognitive-behavioral therapy for bulimia nervosa: time course and mechanisms of change. J Consult Clin Psychol. 2002;70(2):267-74.
- Fairburn CG. Cognitive behavior therapy and eating disorders. New York, NY, US: Guilford Press; 2008. xii, 324-xii, p.
- Sacchetti S, Robinson P, Bogaardt A, Clare A, Ouellet-Courtois C, Luyten P, et al. Reduced mentalizing in patients with bulimia nervosa and features of borderline personality disorder: A case-control study. BMC Psychiatry. 2019;19(1):134. Available from: https://doi.org/10.1186/s12888-019-2112-9.
- van Eeden AE, van Hoeken D, Hoek HW. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr Opin Psychiatry. 2021;34(6):515-24. Available from: https://doi.org/10.1097/yco.0000000000000739.
- Keski-Rahkonen A. Epidemiology of binge eating disorder: prevalence, course, comorbidity, and risk factors. Curr Opin Psychiatry. 2021;34(6):525-31. Available from: https://doi.org/10.1097/yco.0000000000000750.
- Kramer K, Vetter A, Schultz-Venrath U, Vogeley K, Reul S. Mentalization-Based Treatment in Groups for Adults With Autism Spectrum Disorder. Front Psychol. 2021;12:708557. Available from: https://doi.org/10.3389/fpsyg.2021.708557.
- Juul S, Frandsen FW, Bo Hansen S, Sørensen P, Bateman A, Simonsen S. A clinical illustration of short-term mentalization-based therapy for borderline personality disorder. Journal of Clinical Psychology. 2022;78(8):1567-78. Available from: https://doi.org/10.1002/jclp.23378.
- Rathus JH, Miller AL. Dialectical Behavior Therapy Adapted for Suicidal Adolescents. Suicide and Life-Threatening Behavior. 2002;32(2):146-57. Available from: https://doi.org/10.1521/suli.32.2.146.24399.
- Miller AL, Rathus JH, Linehan MM. Dialectical behavior therapy with suicidal adolescents. New York, NY, US: Guilford Press; 2007. xviii, 346-xviii, p.
- Rossouw TI, Fonagy P. Mentalization-based treatment for self-harm in adolescents: a randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(12):1304-13.e3. Available from: https://doi.org/10.1016/j.jaac.2012.09.018.
- Safer DL, Telch CF, Agras WS. Dialectical behavior therapy for bulimia nervosa. The American journal of psychiatry. 2001;158(4):632-4.
- Telch CF, Agras WS, Linehan MM. Dialectical behavior therapy for binge eating disorder. Journal of consulting and clinical psychology. 2001;69(6):1061-5.
- Robinson P, Hellier J, Barrett B, Barzdaitiene D, Bateman A, Bogaardt A, et al. The NOURISHED randomised controlled trial comparing mentalisation-based treatment for eating disorders (MBT-ED) with specialist supportive clinical management (SSCM-ED) for patients with eating disorders and symptoms of borderline personality disorder. Trials. 2016;17(1):549. Available from: https://doi.org/10.1186/s13063-016-1606-8.
- Bateman A, Fonagy P. A randomized controlled trial of a mentalization-based intervention (MBT-FACTS) for families of people with borderline personality disorder. Personality Disorders: Theory, Research, and Treatment. 2019;10(1):70-9. Available from: https://doi.org/10.1037/per0000298.
- SBU. Dialektisk beteendeterapi (DBT) vid borderline personlighetsstörning. Stockholm: Statens beredning för medicinsk utvärdering (SBU); 2005. SBU Alert-rapport 2005-07. [accessed Jul 8 2024]. Available from: https://www.sbu.se/200507.
- SBU. DBT-behandling vid svårt självskadebeteende av unga kvinnor med borderline personlighetsstörning. Stockholm: Statens beredning för medicinsk utvärdering (SBU); 2012. SBU:s upplysningstjänst [accessed Jul 8 2024]. Available from: https://www.sbu.se/dbt.
- SBU. Dialektisk beteendeterapi för att minska suicid eller självskadebeteende. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2021. SBU:s upplysningstjänst ut202106. [accessed Jul 8 2024]. Available from: https://www.sbu.se/ut202106.
- Witt KG, Hetrick SE, Rajaram G, Hazell P, Taylor Salisbury TL, Townsend E, et al. Interventions for self-harm in children and adolescents. The Cochrane database of systematic reviews. 2021;3:CD013667. Available from: https://doi.org/10.1002/14651858.CD013667.pub2.
- SBU. Förebygga självskadebeteende och suicidförsök hos barn och ungdomar – effekter av riktade interventioner. Stockholm Statens beredning för medicinsk och social utvärdering (SBU); 2024. SBU Utvärderar 378. Available from: https://www.sbu.se/378.
- Lee NK, Cameron J, Jenner L. A systematic review of interventions for co-occurring substance use and borderline personality disorders. Drug Alcohol Rev. 2015;34(6):663-72. Available from: https://doi.org/10.1111/dar.12267.
- Brazier J, Tumur I, Holmes M, Ferriter M, Parry G, Dent-Brown K, et al. Psychological therapies including dialectical behaviour therapy for borderline personality disorder: a systematic review and preliminary economic evaluation. Health Technol Assess. 2006;10(35):iii, ix-xii, 1-117. Available from: https://doi.org/10.3310/hta10350.
- Duarte R, Lloyd A, Kotas E, Andronis L, White R. Are acceptance and mindfulness-based interventions 'value for money'? Evidence from a systematic literature review. Br J Clin Psychol. 2019;58(2):187-210. Available from: https://doi.org/10.1111/bjc.12208.
- Midgley N, Sprecher EA, Sleed M. Mentalization-Based Interventions for Children Aged 6-12 and Their Carers: A Narrative Systematic Review. Journal of Infant, Child, and Adolescent Psychotherapy. 2021;20(2):169-89. Available from: https://doi.org/10.1080/15289168.2021.1915654.
- Rozakou-Soumalia N, Dârvariu Ş, Sjögren JM. Dialectical Behaviour Therapy Improves Emotion Dysregulation Mainly in Binge Eating Disorder and Bulimia Nervosa: A Systematic Review and Meta-Analysis. J Pers Med. 2021;11(9). Available from: https://doi.org/10.3390/jpm11090931.
- SBU. Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten: En metodbok. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2023. [accessed Dec 22 2023]. Available from: https://www.sbu.se/metodbok.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372(71).
- Lynch TR, Gray KLH, Hempel RJ, Titley M, Chen EY, O’Mahen HA. Radically open-dialectical behavior therapy for adult anorexia nervosa: feasibility and outcomes from an inpatient program. BMC Psychiatry. 2013;13(1):293. Available from: https://doi.org/10.1186/1471-244X-13-293.
- Covidence systematic review software. Available at www.covidence.org. Melbourne, Australia: Veritas Health Innovation.
- SBU. Granskningsmallar för interventionssudier. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2024. [updated Jan 4 2024; accessed Jul 8 2024]. Available from: https://www.sbu.se/sv/granskningsmallar/#granskningsmall.
- GRADE handbook for grading quality of evidence and strength of recommendations. The GRADE Working Group. [accessed Jul 8 2024]. Available from: https://www.gradeworkinggroup.org/.
- Zeng L, Brignardello-Petersen R, Hultcrantz M, Mustafa RA, Murad MH, Iorio A, et al. GRADE Guidance 34: update on rating imprecision using a minimally contextualized approach. Journal of Clinical Epidemiology. 2022;150:216-24. Available from: byt till denna länk https://doi.org/10.1016/j.jclinepi.2022.07.014.
- Mazzeo SE, Lydecker J, Harney M, Palmberg AA, Kelly NR, Gow RW, et al. Development and preliminary effectiveness of an innovative treatment for binge eating in racially diverse adolescent girls. Eating behaviors. 2016;22:199-205.
- Beck E, Bo S, Jorgensen MS, Gondan M, Poulsen S, Storebo OJ, et al. Mentalization-based treatment in groups for adolescents with borderline personality disorder: a randomized controlled trial. Journal of child psychology and psychiatry, and allied disciplines. 2020;61(5):594-604. Available from: https://doi.org/10.1111/jcpp.13152.
- Jorgensen MS, Storebo OJ, Bo S, Poulsen S, Gondan M, Beck E, et al. Mentalization-based treatment in groups for adolescents with Borderline Personality Disorder: 3- and 12-month follow-up of a randomized controlled trial. European child & adolescent psychiatry. 2021;30(5):699-710. Available from: https://link.springer.com/article/10.1007/s00787-020-01551-2.
- Bianchini V, Cofini V, Curto M, Lagrotteria B, Manzi A, Navari S, et al. Dialectical behaviour therapy (DBT) for forensic psychiatric patients: An Italian pilot study. Criminal behaviour and mental health : CBMH. 2019;29(2):122-30. Available from: https://doi.org/10.1002/cbm.2102.
- Carter GL, Willcox CH, Lewin TJ, Conrad AM, Bendit N. Hunter DBT project: randomized controlled trial of dialectical behaviour therapy in women with borderline personality disorder. The Australian and New Zealand journal of psychiatry. 2010;44(2):162-73. Available from: https://doi.org/10.3109/00048670903393621.
- Dixon-Gordon KL, Chapman AL, Turner BJ. A preliminary pilot study comparing dialectical behavior therapy emotion regulation skills with interpersonal effectiveness skills and a control group treatment. Journal of Experimental Psychopathology. 2015;6(4):369-88. Available from: https://doi.org/10.5127/jep.041714.
- Feigenbaum JD, Fonagy P, Pilling S, Jones A, Wildgoose A, Bebbington PE. A real-world study of the effectiveness of DBT in the UK National Health Service. The British journal of clinical psychology. 2012;51(2):121-41. Available from: https://doi.org/10.1111/j.2044-8260.2011.02017.x.
- Hamid N, Molajegh RR, Bashlideh K, Shehniyailagh M. The comparison of effectiveness of dialectical behavioral therapy (DBT) and schema therapy (ST) in reducing the severity of clinical symptoms (disruptive communication, emotional deregulation and behavioral deregulation) of borderline personality disorder. Pakistan Journal of Medical and Health Sciences. 2020;14(2):1354-63.
- Koons CR, Robins CJ, Lindsey Tweed J, Lynch TR, Gonzalez AM, Morse JQ, et al. Efficacy of dialectical behavior therapy in women veterans with borderline personality disorder. Behavior Therapy. 2001;32(2):371-90. Available from: https://doi.org/10.1016/S0005-7894(01)80009-5.
- Kramer U, Pascual-Leone A, Berthoud L, de Roten Y, Marquet P, Kolly S, et al. Assertive Anger Mediates Effects of Dialectical Behaviour-informed Skills Training for Borderline Personality Disorder: A Randomized Controlled Trial. Clinical psychology & psychotherapy. 2016;23(3):189-202. Available from: https://doi.org/10.1002/cpp.1956.
- Lin T-J, Ko H-C, Wu JY-W, Oei TP, Lane H-Y, Chen C-H. The Effectiveness of Dialectical Behavior Therapy Skills Training Group vs. Cognitive Therapy Group on Reducing Depression and Suicide Attempts for Borderline Personality Disorder in Taiwan. Archives of suicide research : official journal of the International Academy for Suicide Research. 2019;23(1):82-99. Available from: https://doi.org/10.1080/13811118.2018.1436104.
- Linehan MM, Armstrong HE, Suarez A, Allmon D, Heard HL. Cognitive-behavioral treatment of chronically parasuicidal borderline patients. Archives of general psychiatry. 1991;48(12):1060-4.
- Linehan MM, Comtois KA, Murray AM, Brown MZ, Gallop RJ, Heard HL, et al. Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder. Archives of general psychiatry. 2006;63(7):757-66.
- Linehan MM, Heard HL, Armstrong HE. Naturalistic follow-up of a behavioral treatment for chronically parasuicidal borderline patients. Archives of general psychiatry. 1993;50(12):971-4.
- Linehan MM, Korslund KE, Harned MS, Gallop RJ, Lungu A, Neacsiu AD, et al. Dialectical behavior therapy for high suicide risk in individuals with borderline personality disorder: a randomized clinical trial and component analysis. JAMA psychiatry. 2015;72(5):475-82. Available from: https//doi:10.1001/jamapsychiatry.2014.3039.
- Linehan MM, Schmidt H, 3rd, Dimeff LA, Craft JC, Kanter J, Comtois KA. Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. The American journal on addictions. 1999;8(4):279-92.
- Linehan MM, Tutek DA, Heard HL, Armstrong HE. Interpersonal outcome of cognitive behavioral treatment for chronically suicidal borderline patients. The American journal of psychiatry. 1994;151(12):1771-6.
- McMain SF, Guimond T, Barnhart R, Habinski L, Streiner DL. A randomized trial of brief dialectical behaviour therapy skills training in suicidal patients suffering from borderline disorder. Acta psychiatrica Scandinavica. 2017;135(2):138-48. Available from: https://doi.org/10.1111/acps.12664.
- McMain SF, Guimond T, Streiner DL, Cardish RJ, Links PS. Dialectical behavior therapy compared with general psychiatric management for borderline personality disorder: clinical outcomes and functioning over a 2-year follow-up. The American journal of psychiatry. 2012;169(6):650-61. Available from: https://doi.org/10.1176/appi.ajp.2012.11091416.
- McMain SF, Links PS, Gnam WH, Guimond T, Cardish RJ, Korman L, et al. A randomized trial of dialectical behavior therapy versus general psychiatric management for borderline personality disorder. The American journal of psychiatry. 2009;166(12):1365-74. Available from: https://doi.org/10.1176/appi.ajp.2009.09010039.
- Mohamadizadeh L, Makvandi B, Pasha R, Bakhtiarpour S, Hafezi F. Comparing of the effect of Dialectical Behavior Therapy (DBT) and Schema Therapy (ST) on reducing mood activity and suicidal thoughts in patients with borderline personality disorder. Acta Medica Mediterranea. 2017;2017(6):1025-31. Available from: https://doi.org/10.19193/0393-6384_2017_6_162.
- Pistorello J, Fruzzetti AE, Maclane C, Gallop R, Iverson KM. Dialectical behavior therapy (DBT) applied to college students: a randomized clinical trial. Journal of consulting and clinical psychology. 2012;80(6):982-94. Available from: https://doi.org/10.1037/a0029096.
- Priebe S, Bhatti N, Barnicot K, Bremner S, Gaglia A, Katsakou C, et al. Effectiveness and cost-effectiveness of dialectical behaviour therapy for self-harming patients with personality disorder: a pragmatic randomised controlled trial. Psychotherapy and psychosomatics. 2012;81(6):356-65. Available from: https://doi.org/10.1159/000338897.
- Soler J, Pascual JC, Tiana T, Cebria A, Barrachina J, Campins MJ, et al. Dialectical behaviour therapy skills training compared to standard group therapy in borderline personality disorder: a 3-month randomised controlled clinical trial. Behaviour research and therapy. 2009;47(5):353-8. Available from: https://doi.org/10.1016/j.brat.2009.01.013.
- Steuwe C, Berg M, Beblo T, Driessen M. Narrative Exposure Therapy in Patients With Posttraumatic Stress Disorder and Borderline Personality Disorder in a Naturalistic Residential Setting: A Randomized Controlled Trial. Frontiers in psychiatry. 2021;12:765348. Available from: https://doi.org/10.3389/fpsyt.2021.765348.
- Turner RM. Naturalistic evaluation of dialectical behavior therapy-oriented treatment for borderline personality disorder. Cognitive and Behavioral Practice. 2000;7(4):413-9. Available from: https://doi.org/10.1016/S1077-7229(00)80052-8.
- van den Bosch LMC, Koeter MWJ, Stijnen T, Verheul R, van den Brink W. Sustained efficacy of dialectical behaviour therapy for borderline personality disorder. Behaviour research and therapy. 2005;43(9):1231-41.
- Verheul R, Van Den Bosch LMC, Koeter MWJ, De Ridder MAJ, Stijnen T, Van Den Brink W. Dialectical behaviour therapy for women with borderline personality disorder: 12-month, randomised clinical trial in The Netherlands. The British journal of psychiatry : the journal of mental science. 2003;182:135-40.
- Walton CJ, Bendit N, Baker AL, Carter GL, Lewin TJ. A randomised trial of dialectical behaviour therapy and the conversational model for the treatment of borderline personality disorder with recent suicidal and/or non-suicidal self-injury: An effectiveness study in an Australian public mental health servic. The Australian and New Zealand journal of psychiatry. 2020;54(10):1020-34. Available from: https://doi.org/10.1177/0004867420931164.
- Bateman A, Constantinou MP, Fonagy P, Holzer S. Eight-year prospective follow-up of mentalization-based treatment versus structured clinical management for people with borderline personality disorder. Personality disorders. 2021;12(4):291-9. Available from: https://doi.org/10.1037/per0000422.
- Bateman A, Fonagy P. Effectiveness of partial hospitalization in the treatment of borderline personality disorder: a randomized controlled trial. The American journal of psychiatry. 1999;156(10):1563-9.
- Bateman A, Fonagy P. Treatment of borderline personality disorder with psychoanalytically oriented partial hospitalization: an 18-month follow-up. The American journal of psychiatry. 2001;158(1):36-42.
- Bateman A, Fonagy P. 8-year follow-up of patients treated for borderline personality disorder: mentalization-based treatment versus treatment as usual. The American journal of psychiatry. 2008;165(5):631-8. Available from: https://doi.org/10.1176/appi.ajp.2007.07040636.
- Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. The American journal of psychiatry. 2009;166(12):1355-64. Available from: https://doi.org/10.1176/appi.ajp.2009.09040539.
- Carlyle D, Green R, Inder M, Porter R, Crowe M, Mulder R, et al. A Randomized-Controlled Trial of Mentalization-Based Treatment Compared With Structured Case Management for Borderline Personality Disorder in a Mainstream Public Health Service. Frontiers in psychiatry. 2020;11:561916. Available from: https://doi.org/10.3389/fpsyt.2020.561916.
- Jorgensen CR, Freund C, Boye R, Jordet H, Andersen D, Kjolbye M. Outcome of mentalization-based and supportive psychotherapy in patients with borderline personality disorder: a randomized trial. Acta psychiatrica Scandinavica. 2013;127(4):305-17. Available from: https://doi.org/10.1111/j.1600-0447.2012.01923.x.
- Laurenssen EMP, Luyten P, Kikkert MJ, Westra D, Peen J, Soons MBJ, et al. Day hospital mentalization-based treatment v. specialist treatment as usual in patients with borderline personality disorder: randomized controlled trial. Psychological medicine. 2018;48(15):2522-9. Available from: https://doi.org/10.1017/S0033291718000132.
- Philips B, Wennberg P, Konradsson P, Franck J. Mentalization-Based Treatment for Concurrent Borderline Personality Disorder and Substance Use Disorder: A Randomized Controlled Feasibility Study. European addiction research. 2018;24(1):1-8. Available from: https://doi.org/10.1159/000485564.
- Santamarina-Perez P, Mendez I, Singh MK, Berk M, Picado M, Font E, et al. Adapted Dialectical Behavior Therapy for Adolescents with a High Risk of Suicide in a Community Clinic: A Pragmatic Randomized Controlled Trial. Suicide & life-threatening behavior. 2020;50(3):652-67. Available from: https://doi.org/10.1111/sltb.12612.
- Mehlum L, Ramberg M, Tormoen AJ, Haga E, Diep LM, Stanley BH, et al. Dialectical Behavior Therapy Compared With Enhanced Usual Care for Adolescents With Repeated Suicidal and Self-Harming Behavior: Outcomes Over a One-Year Follow-Up. Journal of the American Academy of Child and Adolescent Psychiatry. 2016;55(4):295-300. Available from: https://doi.org/10.1016/j.jaac.2016.01.005.
- Mehlum L, Ramleth R-K, Tormoen AJ, Haga E, Diep LM, Stanley BH, et al. Long term effectiveness of dialectical behavior therapy versus enhanced usual care for adolescents with self-harming and suicidal behavior. Journal of child psychology and psychiatry, and allied disciplines. 2019;60(10):1112-22. Available from: https://doi.org/10.1111/jcpp.13077.
- Chen EY, Cacioppo J, Fettich K, Gallop R, McCloskey MS, Olino T, et al. An adaptive randomized trial of dialectical behavior therapy and cognitive behavior therapy for binge-eating. Psychological medicine. 2017;47(4):703-17. Available from: https://doi.org/10.1017/S0033291716002543.
- Dastan B, Afshar Zanjani S, Froueddin Adl A, Habibi M. The effectiveness of dialectical behaviour therapy for treating women with obesity suffering from BED: A feasibility and pilot study. Clinical Psychologist. 2020;24(2):133-42. Available from: https://doi.org/10.1111/cp.12197.
- Hill DM, Craighead LW, Safer DL. Appetite-focused dialectical behavior therapy for the treatment of binge eating with purging: a preliminary trial. The International journal of eating disorders. 2011;44(3):249-61. Available from: https://onlinelibrary.wiley.com/doi/10.1002/eat.20812.
- Klein AS, Skinner JB, Hawley KM. Targeting binge eating through components of dialectical behavior therapy: preliminary outcomes for individually supported diary card self-monitoring versus group-based DBT. Psychotherapy (Chicago, Ill). 2013;50(4):543-52. Available from: fungera: https://psycnet.apa.org/doiLanding?doi=10.1037%2Fa0033130.
- Masson PC, von Ranson KM, Wallace LM, Safer DL. A randomized wait-list controlled pilot study of dialectical behaviour therapy guided self-help for binge eating disorder. Behaviour research and therapy. 2013;51(11):723-8.
- Rahmani M, Omidi A, Asemi Z, Akbari H. The effect of dialectical behaviour therapy on binge eating, difficulties in emotion regulation and BMI in overweight patients with binge-eating disorder: A randomized controlled trial. Mental Health and Prevention. 2018;9:13-8. Available from: https://doi.org/10.1016/j.mhp.2017.11.002.
- Safer DL, Robinson AH, Jo B. 'Outcome from a randomized controlled trial of group therapy for binge eating disorder: Comparing dialectical behavior therapy adapted for binge eating to an active comparison group therapy' [Behavior Therapy 41 (2010) 106–120]: Erratum. Behavior Therapy. 2010;41(3):432-. Available from: https://doi.org/10.1016/j.beth.2010.04.001.
- Cochrane. Cochrane Handbook for Systematic Reviews of Interventions. Chapter 7: Considering bias and conflicts of interest among the included studies. London: Cochrane. [accessed Jul 8 2024]. Available from: https://training.cochrane.org/handbook/current/chapter-07.
- Jørgensen CR, Bøye R, Andersen D, Døssing Blaabjerg AH, Freund C, Jordet H, et al. Eighteen months post-treatment naturalistic follow-up study of mentalization-based therapy and supportive group treatment of borderline personality disorder: Clinical outcomes and functioning. Nordic Psychology. 2014;66(4):254-73. Available from: https://doi.org/10.1080/19012276.2014.963649.
- Stoffers-Winterling JM, Storebø OJ, Simonsen E, Sedoc Jørgensen M, Pereira Ribeiro J, Kongerslev MT, et al. Perspectives on Dialectical Behavior Therapy and Mentalization-Based Therapy for Borderline Personality Disorder: Same, Different, Complementary? Psychol Res Behav Manag. 2022;15:3179-89. Available from: https://doi.org/10.2147/prbm.S342257.
- Cristea IA, Gentili C, Cotet CD, Palomba D, Barbui C, Cuijpers P. Efficacy of Psychotherapies for Borderline Personality Disorder: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2017;74(4):319-28. Available from: https://doi.org/10.1001/jamapsychiatry.2016.4287.
- Statistik om suicid. Stockholm: Folkhälsomyndigheten. [updated Jun 27 2024; accessed Jul 8 2024]. Available from: https://www.folkhalsomyndigheten.se/livsvillkor-levnadsvanor/psykisk-halsa-och-suicidprevention/suicidprevention/statistik-om-suicid/.
- McCauley E, Berk MS, Asarnow JR, Adrian M, Cohen J, Korslund K, et al. Efficacy of Dialectical Behavior Therapy for Adolescents at High Risk for Suicide: A Randomized Clinical Trial. JAMA Psychiatry. 2018;75(8):777-85. Available from: https://doi.org/10.1001/jamapsychiatry.2018.1109.
- Socialstyrelsen. Nationella riktlinjer 2024: Ätstörningar. Stockholm: Socialstyrelsen; 2024. Nationella riktlinjer. [accessed Sept 25 2024]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/nationella-riktlinjer/2024-5-9039.pdf.
- Zetterqvist M, Lundh LG, Dahlström O, Svedin CG. Prevalence and function of non-suicidal self-injury (NSSI) in a community sample of adolescents, using suggested DSM-5 criteria for a potential NSSI disorder. J Abnorm Child Psychol. 2013;41(5):759-73. Available from: https://doi.org/10.1007/s10802-013-9712-5.
- Griffiths H, Duffy F, Duffy L, Brown S, Hockaday H, Eliasson E, et al. Efficacy of Mentalization-based group therapy for adolescents: the results of a pilot randomised controlled trial. BMC Psychiatry. 2019;19(1):167. Available from: https://doi.org/10.1186/s12888-019-2158-8.
- Prevolnik Rupel V, Jagger B, Fialho LS, Chadderton L-M, Gintner T, Arntz A, et al. Standard set of patient-reported outcomes for personality disorder. Quality of Life Research. 2021;30(12):3485-500. Available from: https://doi.org/10.1007/s11136-021-02870-w.
- Gunderson JG. Borderline personality disorder: ontogeny of a diagnosis. Am J Psychiatry. 2009;166(5):530-9. Available from: https://doi.org/10.1176/appi.ajp.2009.08121825.

 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services
 Share on Facebook
Share on Facebook
 Share on LinkedIn
Share on LinkedIn
 Share via Email
Share via Email