Interventions for adults with co-occurring addictive and psychiatric disorders
A systematic review including health economic and ethical aspects
Main message
Psychological and psychosocial treatment can reduce both substance use and psychiatric symptoms in patients with comorbidity between addiction and other psychiatric conditions. However, there is a significant lack of scientific evidence regarding the effects of pharmacological treatment for this population.
Conclusions
- Psychological and psychosocial treatment, particularly contingency management, may reduce substance use in patients with addiction and co-occurring severe mental illnesses such as schizophrenia or bipolar disorder. In cases of comorbidity between addiction and depression, anxiety disorders, or post-traumatic stress disorder, psychological and psychosocial treatment may lead to reductions in both substance use and psychiatric symptoms. This is especially evident for cognitive behavioural therapy and integrated treatments (treatments that target both substance use and the co-occurring psychiatric condition).
- Naltrexone may reduce alcohol consumption in individuals with alcohol dependence and another comorbid psychiatric disorder, without any apparent negative effect on the psychiatric condition.
- More research is needed on the treatment of specific comorbid combinations, particularly regarding pharmacological interventions. Further research is also needed on treatment addressing psychiatric disorders and co-occurring gambling disorder, as well as any addictive condition in combination with specific psychiatric disorders such as: anxiety disorders, obsessive-compulsive disorder, neuropsychiatric disorders, personality disorders, and eating disorders. In addition, there is a need for research on coordinated care interventions and social support measures for people with dual diagnoses.
- The lack of evidence for the treatment of specific comorbidities should not preclude offering care to individuals with comorbidity, as substance use disorders and co-occurring psychiatric conditions interact in ways that, if left untreated, often lead to a negative cycle and worsening of both conditions.
- Results from studies investigating treatment for either condition alone may, in some cases, be considered the best available knowledge to inform treatment of individuals with co-occurring disorders.
Aim
The aim of this systematic review is to evaluate the scientific evidence for any form of treatment targeting adults with addiction in combination with at least one other psychiatric disorder. The review also includes an analysis of health economic aspects as well as an ethical discussion of the findings.
Background
Co-occurrence of a substance use disorder, and one or more other psychiatric conditions is common and is often associated with significantly poorer health and quality of life, worse treatment prognosis, and an increased risk of premature death compared to having only one of the conditions. This type of comorbidity is also associated with increased burden on family members and substantial costs for society. At the same time, it is important to acknowledge that individuals with comorbid disorders do not represent a homogeneous group; symptom severity and overall functioning can vary widely between individuals.
Method
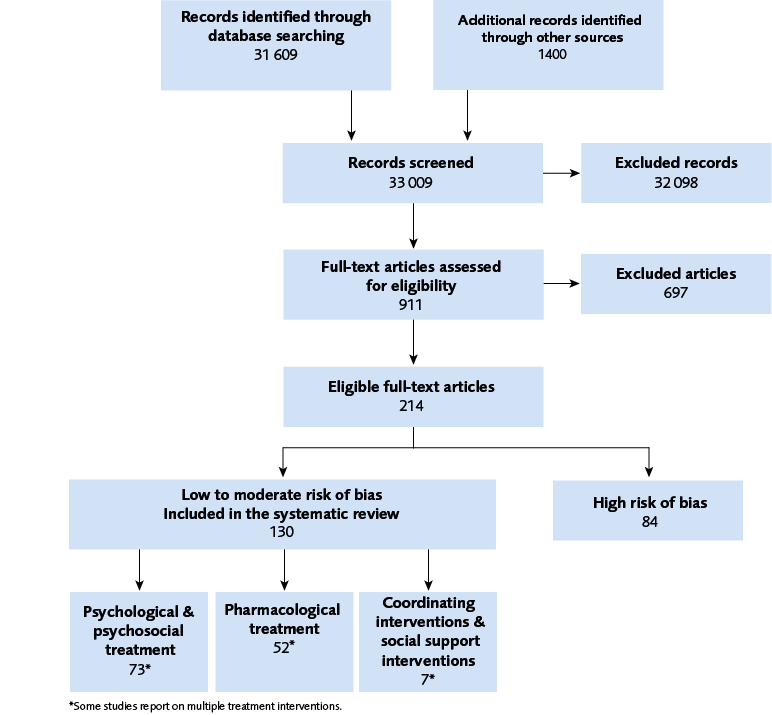
We conducted a systematic review and reported in accordance with the PRISMA statement. The protocol is registered in Prospero (CRD42022382508). The certainty of evidence was assessed with GRADE. Inclusion criteria (PICO)
Population: Adults with diagnosed with a substance use disorder or gambling disorder in combination with at least one other psychiatric diagnosis
Intervention: Any pharmacological, psychological, psychosocial or social support interventions1
Control: Any treatment or no treatment
Outcome: Any of the following: substance use, mental health symptoms, function, quality of life
Study design: Randomized controlled trial (RCT)
Language: English, Swedish, Norwegian, Danish
Databases searched: CINAHL (EBSCO), Cochrane Library (Wiley), Embase (Elsevier), Medline (OvidSP), PsycINFO (EBSCO) and Scopus (Elsevier)
Patient involvement: A reference group comprising diverse stakeholders – including former patients with lived experience, clinicians, health care providers and decision makers – provided feedback on the project plan and the ethical discussion.
1. Studies of social support interventions needed to report outcomes for substance use to be included.
Results
A total of 120 studies, reported across 130 research papers, focusing on the treatment of adults with dual diagnoses, were included. Psychological and psychosocial treatments, pharmacological interventions, as well as coordinating interventions (e.g., case management) and social support interventions, were reported separately. Psychological and psychosocial treatments were compared either to treatment as usual or to another active intervention. The results were further categorised into four diagnostic groups: (1) severe mental illness (bipolar disorder or schizophrenia), (2) depression, anxiety, or PTSD, (3) ADHD, and (4) personality disorders. Pharmacological treatments were assessed based on the specific active pharmacological agent investigated and the combination of psychiatric diagnosis and primary substance use diagnosis (see Figure 3). Due to heterogeneity across studies – including variations in population characteristics, interventions, and outcome measures – the results were synthesised narratively without meta-analysis.
| Treatment | Follow up | Outcome | Grade | Interpretation |
|---|---|---|---|---|
| Psychological or psychosocial treatment (any, main analysis) | 0-3 months post baseline | Per cent days abstinent | More days abstinent | |
| Contingency management (subgroup analysis) | 0-3 months post baseline | Per cent days abstinent | More days abstinent |
| CBT = cognitive behavioural therapy: Integrated treatment = treatment with focus on both addiction and other psychiatric symptoms | ||||
| Treatment | Follow up | Outcome | Grade | Interpretation |
|---|---|---|---|---|
| Psychological or psychosocial treatment (any, main analysis) | 3-12 months post baseline | Per cent days abstinent | More days abstinent | |
| CBT (subgroup analysis) | 3-12 months post baseline | Per cent days abstinent | More days abstinent | |
| Integrated treatment (subgroup analysis) | 3-12 months post baseline | Per cent days abstinent | More days abstinent | |
| Psychological or psychosocial treatment (any, main analysis) | 0-3 months post baseline | Psychiatric symptoms | Less symptoms | |
| CBT (subgroup analysis) | 0-3 months post baseline | Psychiatric symptoms | Less symptoms | |
| Integrated treatment (subgroup analysis) | 0-3 months post baseline | Psychiatric symptoms | Less symptoms | |
| Psychological or psychosocial treatment (any, main analysis) | 3-12 months post baseline | Psychiatric symptoms | Less symptoms | |
| CBT (subgroup analysis) | 3-12 months post baseline | Psychiatric symptoms | Less symptoms | |
| Integrated treatment (subgroup analysis) | 3-12 months post baseline | Psychiatric symptoms | Less symptoms | |
| CBT = cognitive behavioural therapy: Integrated treatment = treatment with focus on both addiction and other psychiatric symptoms | ||||
| Treatment | Follow up | Outcome | Grade | Interpretation |
|---|---|---|---|---|
| CBT compared to other psychological or psychosocial treatment | 3-12 months post baseline | Per cent days abstinent | CBT is at least as good as other kinds of psychological or psychosocial treatment | |
| Integrated treatment compared to addiction treatment alone | 3-12 months post baseline | Per cent days abstinent | Integrated treatment is not better than addiction treatment alone | |
| CBT compared to other psychological or psychosocial treatment | 0-3 months post baseline | Psychiatric symptoms | The evidence is very uncertain about CBT compared to other kinds of psychological or psychosocial treatment | |
| Integrated treatment compared to addiction treatment alone | 0-3 months post baseline | Psychiatric symptoms | Integrated treatment is at least as good as addiction treatment alone | |
| CBT compared to other psychological or psychosocial treatment | 3-12 months post baseline | Psychiatric symptoms | The evidence is very uncertain about CBT compared to other kinds of psychological or psychosocial treatment | |
| Integrated treatment compared to addiction treatment alone | 3-12 months post baseline | Psychiatric symptoms | Integrated treatment is at least as good as addiction treatment alone | |
Health economic aspects
Health economic studies analysing costs, resource utilisation, and quality of life indicate that dual diagnoses are associated with increased healthcare and judicial system costs, as well as resource use, compared to having a single or no psychiatric or substance use disorder diagnosis. Furthermore, while a psychiatric diagnosis alone negatively impacts the person’s quality of life, the presence of concurrent substance use appears to exacerbate this decline.
In the systematic review of health economic literature, two studies were identified that evaluated the cost-effectiveness of contingency management for individuals with severe mental illness. These health economic analyses were based on randomised controlled trials conducted in England and the United States.
Ethics
Research on interventions for individuals with co-occurring substance use disorders and mental health conditions must be guided by the care and support needs of this population. It is therefore essential to consider the living conditions of the target group, alongside broader societal and healthcare system factors. Stigmatisation and discrimination are pervasive challenges faced daily by many individuals within this group. This discussion emphasises ethical issues arising at the intersection of users’ needs, evidence-based knowledge, and the interventions provided. Research in this area involves several ethically significant concerns, often related to the vulnerable position of individuals with dual diagnoses.
Discussion
Interpreting treatment studies on individuals with comorbid substance use and other psychiatric disorders is challenging due to variations in diagnoses, symptom severity, and intervention types. Despite these challenges and the considerable heterogeneity among studies, this systematic review suggests that several psychological, psychosocial, and certain pharmacological treatments may offer benefits. However, the diversity of study designs and populations make it difficult to draw definitive conclusions regarding effect sizes or to identify the most effective treatments for specific comorbidity profiles. Substantial knowledge gaps persist, as high-quality research is often scarce or yields inconclusive findings. Nonetheless, early access to care remains essential given the substantial negative impact of comorbidity on health outcomes and quality of life.
Conflict of Interest
In accordance with SBU’s requirements, the experts and scientific reviewers participating in this project have submitted statements about conflicts of interest. These documents are available at SBU’s secretariat. SBU has determined that the conditions described in the submissions are compatible with SBU’s requirements for objectivity and impartiality.
Appendices
- Search strategies (https://www.sbu.se/contentassets/3f6efaada75c454ebee5e59744199dac/appendix-1-search-strategies.pdf)
- Excluded references (https://www.sbu.se/contentassets/3f6efaada75c454ebee5e59744199dac/appendix-2-excluded-studies.pdf)
- Studies not included in analysis due to Risk of Bias (https://www.sbu.se/contentassets/3f6efaada75c454ebee5e59744199dac/appendix-3-studies-with-critical-or-high-risk-of-bias.pdf)
- Characteristics of included studies (https://www.sbu.se/contentassets/3f6efaada75c454ebee5e59744199dac/appendix-4-characteristics-of-included-studies.xlsx and https://www.sbu.se/contentassets/3f6efaada75c454ebee5e59744199dac/appendix-5-characteristics-of-included-pharmacology-studies.pdf)
Project group
Experts
- Joar Guterstam, Senior Psychiatrist, MD, PhD, Associate Professor. Stockholm Centre for Dependency Disorders, Department of Clinical Neuroscience, Karolinska Institutet
- Anders Hammarberg, Lic. Psychotherapist, Associate Professor, , Department of Clinical Neuroscience, Centre for Psychiatry Research, Karolinska Institutet
- Åsa Magnusson, Senior Physician, MD, Stockholm Centre for Dependency Disorders, Department of Clinical Neuroscience, Karolinska Institutet
- Annika Nordström, Social Worker, MD in psychiatry, affiliated with the Department of Epidemiology and Global Health, Umeå University
- Sara Wallhed Finn, Reg. Psychologist, Associate Professor, Stockholm Centre for Dependency Disorders, Department of Global Public Health, Karolinska Institutet
- Agneta Öjehagen, Social Worker, Lic. Psychotherapist, Doctor in Medical Science, Professor, Faculty of Medicine, Psychiatry, Lund University
Kansli
- Nils Stenström, Project Director
- Marie Österberg, Project Director (from 2022--01-01 until 2023-10-31)
- Idha Kurtsdotter, Project Director (from 2023-01-01)
- Rebecca A. Silverstein, Project Director (from March 2023)
- Annicka Hedman, Project Director (from 2023-03-23 until 2023-10-03)
- Johanna Wiss, Health Economist
- Jenny Berg, Health Economist
- Elham Mohammed Ali, Analyst (from 2024-06-11)
- Erik Eriksson, Analyst (from 2024-11-04 until 2025-03-03)
- Hanna Olofsson, Information Specialist (until 2022-08-31)
- Carl Gornitzki, Information Specialist (from 2022-09-01)
- Irini Åberg, Project Administrator (until 2025-03-18)
- Elin Malmer, Project Administrator (from 2025-03-19)
- Maria Ahlberg, Project Administrator (from 2025-03-19)
- Sara Fundell, Project Administrator (from 2025-03-19)
- Maria Hoppe, Project Administrator (from 2025-04-07)
- Sofia Tranæus, Head of Unit
Flow chart
References
- EMCDDA. Comorbidity of substance use and mental health disorders in Europe (Perspectives on drugs). Lisbon: The European Monitoring Centre for Drugs and Drug Addiction (EMCDDA); 2016. [accessed 21 Nov 2023]. Available from: https://www.emcdda.europa.eu/publications/pods/comorbidity-substance-use-mental-health_en
- Nationella riktlinjer för vård och stöd vid missbruk och beroende. Stockholm: Socialstyrelsen; 2018. [accessed 11 nov 2023]. Available from: https://www.socialstyrelsen.se/kunskapsstod-och-regler/regler-och-riktlinjer/nationella-riktlinjer/riktlinjer-och-utvarderingar/missbruk-och-beroende/ .
- Common Comorbidities with Substance Use Disorders Research Report. In. Bethesda (MD): National Institutes on Drug Abuse (US); 2020. Kartläggning av samsjuklighet i form av psykisk ohälsa och beroendeproblematik. Stockholm: Socialstyrelsen; 2019. [accessed 24 nov 2023]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2019-11-6481.pdf
- Crowe M, Eggleston K, Douglas K, Porter RJ. Effects of psychotherapy on comorbid bipolar disorder and substance use disorder: A systematic review. Bipolar Disord. 2021;23(2):141-51. Available from: https://doi.org/10.1111/bdi.12971
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(8):807-16. Available from: https://doi.org/10.1001/archpsyc.61.8.807
- Holmstrand C, Bogren M, Mattisson C, Bradvik L. Long-term suicide risk in no, one or more mental disorders: the Lundby Study 1947-1997. Acta Psychiatr Scand. 2015;132(6):459-69. Available from: https://doi.org/10.1111/acps.12506
- Kommunikation med medförfattare Louise Brådvik. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2024. SBU 2021/775.
- Gerdner A, Hakansson A. Prevalence and comorbidity in a Swedish adolescent community sample - gambling, gaming, substance use, and other psychiatric disorders. BMC Psychiatry. 2022;22(1):594. Available from: https://doi.org/10.1186/s12888-022-04218-1
- SOU 2021:93. Från delar till helhet – En reform för samordnade, behovsanpassade och personcentrerade insatser till personer med samsjuklighet. Statens offentliga utredningar. Stockholm: Elanders Sverige AB. [updated Nov 25 2021; accessed Sep 12 2023]. Available from: https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/2021/11/sou-202193/
- Adult Psychopathology and Diagnosis, 5th Edition. New Jersey: John Wiley & Sons, Inc.; 2011. Available from: https://www.wiley.com/en-us/Adult+Psychopathology+and+Diagnosis%2C+5th+Edition-p-9781118046326
- Langas AM, Malt UF, Opjordsmoen S. Comorbid mental disorders in substance users from a single catchment area—a clinical study. BMC Psychiatry. 2011;11:25. Available from: https://doi.org/10.1186/1471-244X-11-25
- Stahler GJ, Mennis J, Cotlar R, Baron DA. The influence of neighborhood environment on treatment continuity and rehospitalization in dually diagnosed patients discharged from acute inpatient care. Am J Psychiatry. 2009;166(11):1258-68. Available from: https://doi.org/10.1176/appi.ajp.2009.08111667
- Szerman N, Lopez-Castroman J, Arias F, Morant C, Babín F, Mesías B, et al. Dual diagnosis and suicide risk in a Spanish outpatient sample. Subst Use Misuse. 2012;47(4):383-9. Available from: https://doi.org/10.3109/10826084.2011.636135
- Hunt GE, Siegfried N, Morley K, Brooke-Sumner C, Cleary M. Psychosocial interventions for people with both severe mental illness and substance misuse. Cochrane Database Syst Rev. 2019;12(12):Cd001088. Available from: https://doi.org/10.1002/14651858.CD001088.pub4
- Khokhar JY, Dwiel LL, Henricks AM, Doucette WT, Green AI. The link between schizophrenia and substance use disorder: A unifying hypothesis. Schizophr Res. 2018;194:78-85. Available from: https://doi.org/10.1016/j.schres.2017.04.016
- Mueser KT, Deavers F, Penn DL, Cassisi JE. Psychosocial treatments for schizophrenia. Annu Rev Clin Psychol. 2013;9:465-97. Available from: https://doi.org/10.1146/annurev-clinpsy-050212-185620
- Sullivan LE, Fiellin DA, O’Connor PG. The prevalence and impact of alcohol problems in major depression: a systematic review. Am J Med. 2005;118(4):330-41. Available from: https://doi.org/10.1016/j.amjmed.2005.01.007
- SAMHSA/CSAT Treatment Improvement Protocols. In: Substance Use Disorder Treatment for People With Co-Occurring Disorders: Updated 2020. SAMHSA/CSAT Treatment Improvement Protocols. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 2020.
- Kodning inom psykiatrin. Stockholm: Socialstyrelsen. [updated May 2 2023]. Available from: https://www.socialstyrelsen.se/statistik-och-data/klassifikationer-och-koder/icd-10/psykiatrikoder/
- Alkoholberoende, diagnostik och behandling. Kungsbacka: Internetmedicin. [updated Aug 30 2021]. Available from: https://w3.internetmedicin.se/page.aspx?id=1590
- Wallhed Finn S, Lundin A, Sjoqvist H, Danielsson AK. Pharmacotherapy for alcohol use disorders – Unequal provision across sociodemographic factors and co-morbid conditions. A cohort study of the total population in Sweden. Drug Alcohol Depend. 2021;227:108964. Available from: https://doi.org/ 1016/j.drugalcdep.2021.108964
- Förbättrat stöd till unga – enkät februari 2021 till unga med samsjuklighet. Stockholm: Brukarkraft – Resurscentrum för brukarinflytande; 2021. [accessed Sep 12 2023]. Available from: https://brukarkraft.se/wp-content/uploads/2021/04/Rapport-Brukarkrafts-enka%CC%88t-unga-med-samsjukl-ighet.pdf
- De Ruysscher C, Vandevelde S, Vanderplasschen W, De Maeyer J, Vanheule S. The Concept of Recovery as Experienced by Persons with Dual Diagnosis: A Systematic Review of Qualitative Research From a First-Person Perspective. J Dual Diagn. 2017;13(4):264-79. Available from: https://doi.org/10.1080/15504263.2017.1349977
- KBT (Kognitiv beteendeterapi). Stockholm: Socialstyrelsen; 2019. [updated Jan 26 2019; accessed 24 nov 2023]. Available from: https://www.socialstyrelsen.se/kunskapsstod-och-regler/omraden/evidensbaserad-praktik/metodguiden/kbt-kognitiv-beteendeterapi/
- Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten: en metodbok. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2023. Available from: http://www.sbu.se/sv/var-metod/
- Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. 2020;368:l6890. Available from: https://doi.org/10.1136/bmj.l6890
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. Available from: https://doi.org/10.1371/journal.pmed.1000097
- Samsjuklighet mellan substansbruk och annan psykisk sjukdom/tillstånd. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2022. SBU Förstudie. [accessed Sep 12 2023]. Available from: https://www.sbu.se/sv/publikationer/forstudie-sammanfattning/forstudie-samsjuklighet-mellan-substansbruk-och-annan-psykisk-sjukdomtillstand/
- Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan - a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. Available from: https://doi.org/10.1186/s13643-016-0384-4
- Covidence systematic review software. Melbourne: Veritas Health Innovation. Available from: covidence.org
- Bedömning av randomiserade studier (effekt av att tilldelas en intervention (ITT)). Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2020. [accessed Apr 9 2025]. Available from: https://www.sbu.se/sv/granskningsmallar/arkiv-granskningsmallar/
- Borenstein M, Hedges L, Higgins J, Rothstein H. Comprehensive Meta-Analysis Version 4. Englewood, NJ 2022: Biostat.
- The Nordic Cochrane Centre TCC. Review Manager (RevMan) [Computer program]. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration. Available from: https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revman
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Bmj. 2008;336(7650):924-6. Available from: https://doi.org/10.1136/bmj.39489.470347.AD
- Moberg K, Berg J, Eriksson T, Lundqvist M, Wiss J, Ringborg A. A comparison of two search filters for economic evaluations. The CADTH Narrow vs the NHS EED search filter. 27th Cochrane Colloquium; London. Available from: https://doi.org/10.1002/14651858.CD202301
- Mall för kvalitets- granskning av empiriska hälsoekonomiska studier. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2017. [accessed Nov 24 2023]. Available from: https://www.sbu.se/sv/granskningsmallar/#granskningsmall
- Etiska aspekter på insatser inom det sociala området. En vägledning för att identifiera relevanta etiska aspekter. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2019. [accessed April 7 2025]. Available from: https://www.sbu.se/globalassets/ebm/etiska_aspekter_sociala_omradet.pdf
- Etiska aspekter på insatser inom hälso- och sjukvården. En vägledning för att identifiera relevanta etiska aspekter. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2021. [accessed April 7 2025]. Available from: https://www.sbu.se/globalassets/ebm/etiska_aspekter_halso_sjukvarden.pdf
- SOU 2011:35. Bättre insatser vid missbruk och beroende. Statens offentliga utredningar. Stockholm: Elanders Sverige AB. [updated Apr 2 2015; accessed Sep 12 2023]. Available from: https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/2011/04/sou-201135/
- SOU 2023:62. Vi kan bättre! Kunskapsbaserad narkotikapolitik med liv och hälsa i fokus. Statens offentliga utredningar. Stockholm: Elanders Sverige AB. [updated Okt 26 2023; accessed Sep 12 2023]. Available from: https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/2023/10/sou-202362/
- Barrowclough C, Haddock G, Tarrier N, Lewis SW, Moring J, O’Brien R, et al. Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. Am J 2001;158(10):1706-13. Available from: https://doi.org/10.1176/appi.ajp.158.10.1706
- Barrowclough C, Haddock G, Wykes T, Beardmore R, Conrod P, Craig T, et al. Integrated motivational interviewing and cognitive behavioural therapy for people with psychosis and comorbid substance misuse: randomised controlled trial. BMJ. 2010;341:c6325. Available from: https://doi.org/10.1136/bmj.c6325
- Barrowclough C, Marshall M, Gregg L, Fitzsimmons M, Tomenson B, Warburton J, et al. A phase-specific psychological therapy for people with problematic cannabis use following a first episode of psychosis: a randomized controlled trial. Psychol Med. 2014;44(13):2749-61. Available from: https://doi.org/10.1017/S0033291714000208
- Bogenschutz MP, Rice SL, Tonigan JS, Vogel HS, Nowinski J, Hume D, et al. 12-step facilitation for the dually diagnosed: a randomized clinical trial. J Subst Abuse Treat. 2014;46(4):403-11. Available from: https://doi.org/10.1016/j.jsat.2013.12.009
- Bonsack C, Gibellini Manetti S, Favrod J, Montagrin Y, Besson J, Bovet P, et al. Motivational intervention to reduce cannabis use in young people with psychosis: a randomized controlled trial. Psychother Psychosom. 2011;80(5):287-97. Available from: https://doi.org/10.1159/000323466
- Eack SM, Hogarty SS, Greenwald DP, Litschge MY, McKnight SA, Bangalore SS, et al. Cognitive Enhancement Therapy in substance misusing schizophrenia: results of an 18-month feasibility trial. Schizophr Res. 2015;161(2-3):478-83. Available from: https://doi.org/10.1016/j.schres.2014.11.017
- Gonzalez-Ortega I, Echeburua E, Alberich S, Bernardo M, Vieta E, de Pablo GS, et al. Cognitive Behavioral Therapy Program for Cannabis Use Cessation in First-Episode Psychosis Patients: A 1-Year Randomized Controlled Trial. Int J Environ Res Public Health. 2022;19(12). Available from: https://doi.org/10.3390/ijerph19127325
- Gouzoulis-Mayfrank E, Konig S, Koebke S, Schnell T, Schmitz-Buhl M, Daumann J. Trans-Sector Integrated Treatment in Psychosis and Addiction. Dtsch Arztebl Int. 2015;112(41):683-91. Available from: https://doi.org/10.3238/arztebl.2015.0683
- Graeber DA, Moyers TB, Griffith G, Guajardo E, Tonigan S. A pilot study comparing motivational interviewing and an educational intervention in patients with schizophrenia and alcohol use disorders. Community Ment Health J. 2003;39(3):189-202. Available from: https://doi.org/10.1023/a:1023371705506
- Graham HL, Copello A, Griffith E, Freemantle N, McCrone P, Clarke L, et al. Pilot randomised trial of a brief intervention for comorbid substance misuse in psychiatric in-patient settings. Acta Psychiatr Scand. 2016;133(4):298-309. Available from: https://doi.org/10.1111/acps.12530
- Herman SE, Frank KA, Mowbray CT, Ribisl KM, Davidson WS, 2nd, BootsMiller B, et al. Longitudinal effects of integrated treatment on alcohol use for persons with serious mental illness and substance use disorders. J Behav Health Serv Res. 2000;27(3):286-302. Available from: https://doi.org/10.1007/BF02291740
- Hjorthoj CR, Fohlmann A, Larsen AM, Gluud C, Arendt M, Nordentoft M. Specialized psychosocial treatment plus treatment as usual (TAU) versus TAU for patients with cannabis use disorder and psychosis: the CapOpus randomized trial. Psychol Med. 2013;43(7):1499-510. Available from: https://doi.org/10.1017/S0033291712002255
- James W, Preston NJ, Koh G, Spencer C, Kisely SR, Castle DJ. A group intervention which assists patients with dual diagnosis reduce their drug use: a randomized controlled trial. Psychol Med. 2004;34(6):983-90. Available from: https://doi.org/10.1017/s0033291703001648
- Johnson S, Rains LS, Marwaha S, Strang J, Craig T, Weaver T, et al. A contingency management intervention to reduce cannabis use and time to relapse in early psychosis: the CIRCLE RCT. Health Technol Assess. 2019;23(45):1-108. Available from: https://doi.org/10.3310/hta23450
- Madigan K, Brennan D, Lawlor E, Turner N, Kinsella A, O’Connor JJ, et al. A multi-center, randomized controlled trial of a group psychological intervention for psychosis with comorbid cannabis dependence over the early course of illness. Schizophr Res. 2013;143(1):138-42. Available from: https://doi.org/10.1016/j.schres.2012.10.018
- Martino S, Carroll KM, Nich C, Rounsaville BJ. A randomized controlled pilot study of motivational interviewing for patients with psychotic and drug use disorders. Addiction. 2006;101(10):1479-92. Available from: https://doi.org/10.1111/j.1360-0443.2006.01554.x
- McDonell MG, Leickly E, McPherson S, Skalisky J, Srebnik D, Angelo F, et al. ‘A randomized controlled trial of ethyl glucuronide-based contingency management for outpatients with co-occurring alcohol use disorders and serious mental illness’: Correction. Am J Psychiatry. 2017;174(6):604-.
- McDonell MG, Srebnik D, Angelo F, McPherson S, Lowe JM, Sugar A, et al. Randomized controlled trial of contingency management for stimulant use in community mental health patients with serious mental illness. Am J Psychiatry. 2013;170(1):94-101. Available from: https://doi.org/10.1176/appi.ajp.2012.11121831
- Mueser KT, Glynn SM, Cather C, Xie H, Zarate R, Smith LF, et al. A randomized controlled trial of family intervention for co-occurring substance use and severe psychiatric disorders. Schizophr Bull. 2013;39(3):658-72. Available from: https://doi.org/10.1093/schbul/sbr203
- O’Connell MJ, Flanagan EH, Delphin-Rittmon ME, Davidson L. Enhancing outcomes for persons with co-occurring disorders through skills training and peer recovery support. J Ment Health. 2020;29(1):6-11. Available from: https://doi.org/10.1080/09638237.2017.1294733
- Schmitz JM, Averill P, Sayre S, McCleary P, Moeller FG, Swann A. Cognitive-behavioral treatment of bipolar disorder and substance abuse: a preliminary randomized study. Addict Disord Their Treat. 2002;1(1):17-24.
- Weiss RD, Griffin ML, Jaffee WB, Bender RE, Graff FS, Gallop RJ, et al. A “community-friendly” version of integrated group therapy for patients with bipolar disorder and substance dependence: a randomized controlled trial. Drug Alcohol Depend. 2009;104(3):212-9. Available from: https://doi.org/ 1016/j.drugalcdep.2009.04.018
- Weiss RD, Griffin ML, Kolodziej ME, Greenfield SF, Najavits LM, Daley DC, et al. A randomized trial of integrated group therapy versus group drug counseling for patients with bipolar disorder and substance dependence. Am J Psychiatry. 2007;164(1):100-7. Available from: https://doi.org/10.1176/ajp.2007.164.1.100
- Wenze SJ, Gaudiano BA, Weinstock LM, Tezanos KM, Miller IW. Adjunctive psychosocial intervention following Hospital discharge for Patients with bipolar disorder and comorbid substance use: A pilot randomized controlled trial. Psychiatry Res. 2015;228(3):516-25. Available from: https://doi.org/ 1016/j.psychres.2015.06.005
- de Waal MM, Dekker JJM, Kikkert MJ, Christ C, Chmielewska J, Staats MWM, et al. Self-wise, Other-wise, Streetwise (SOS) training, an intervention to prevent victimization in dual-diagnosis patients: results from a randomized clinical trial. Addiction. 2019;114(4):730-40. Available from: https://doi.org/10.1111/add.14500
- Baker AL, Kavanagh DJ, Kay-Lambkin FJ, Hunt SA, Lewin TJ, Carr VJ, et al. Randomized controlled trial of cognitive-behavioural therapy for coexisting depression and alcohol problems: short-term outcome. Addiction. 2010;105(1):87-99. Available from: https://doi.org/ 1111/j.1360-0443.2009.02757.x
- Haddock G, Barrowclough C, Tarrier N, Moring J, O’Brien R, Schofield N, et al. Cognitive-behavioural therapy and motivational intervention for schizophrenia and substance misuse. 18-month outcomes of a randomised controlled trial. Br J Psychiatry. 2003;183:418-26. Available from: https://doi.org/10.1192/bjp.183.5.418
- Agyapong VI, Ahern S, McLoughlin DM, Farren CK. Supportive text messaging for depression and comorbid alcohol use disorder: single-blind randomised trial. J Affect Disord. 2012;141(2-3):168-76. Available from: https://doi.org/10.1016/j.jad.2012.02.040
- Agyapong VI, McLoughlin DM, Farren CK. Six-months outcomes of a randomised trial of supportive text messaging for depression and comorbid alcohol use disorder. J Affect Disord. 2013;151(1):100-4. Available from: https://doi.org/10.1016/j.jad.2013.05.058
- Back SE, Killeen T, Badour CL, Flanagan JC, Allan NP, Ana ES, et al. Concurrent treatment of substance use disorders and PTSD using prolonged exposure: A randomized clinical trial in military veterans. Addict Behav. 2019;90:369-77. Available from: https://doi.org/10.1016/j.addbeh.2018.11.032
- Baker AL, Kavanagh DJ, Kay-Lambkin FJ, Hunt SA, Lewin TJ, Carr VJ, et al. Randomized controlled trial of MICBT for co-existing alcohol misuse and depression: outcomes to 36-months. J Subst Abuse Treat. 2014;46(3):281-90. Available from: https://doi.org/10.1016/j.jsat.2013.10.001
- Buckner JD, Zvolensky MJ, Ecker AH, Schmidt NB, Lewis EM, Paulus DJ, et al. Integrated cognitive behavioral therapy for comorbid cannabis use and anxiety disorders: A pilot randomized controlled trial. Behav Res Ther. 2019;115:38-45. Available from: https://doi.org/10.1016/j.brat.2018.10.014
- Coffey SF, Schumacher JA, Nosen E, Littlefield AK, Henslee AM, Lappen A, et al. Trauma-focused exposure therapy for chronic posttraumatic stress disorder in alcohol and drug dependent patients: A randomized controlled trial. Psychol Addict Behav. 2016;30(7):778-90. Available from: https://doi.org/10.1037/adb0000201
- Daros AR, Guimond TH, Yager C, Palermo EH, Wilks CR, Quilty LC. Feasibility, Acceptability, and Potential Efficacy of a Self-Guided Internet-Delivered Dialectical Behavior Therapy Intervention for Substance Use Disorders: Randomized Controlled Trial. JMIR Ment Health. 2024;11:e50399. Available from: https://doi.org/10.2196/50399
- DiNitto DM, Webb DK, Rubin A. The Effectiveness of an Integrated Treatment Approach for Clients With Dual Diagnoses. Res Soc Work Pract. 2002;12(5):621-41. Available from: https://doi.org/10.1177/1049731502012005003
- Drebing CE, Van Ormer EA, Mueller L, Hebert M, Penk WE, Petry NM, et al. Adding contingency management intervention to vocational rehabilitation: outcomes for dually diagnosed veterans. J Rehabil Res Dev. 2007;44(6):851-65.
- Fals-Stewart W, Schafer J. The treatment of substance abusers diagnosed with obsessive-compulsive disorder: an outcome study. J Subst Abuse Treat. 1992;9(4):365-70. Available from: https://doi.org/10.1016/0740-5472(92)90032-j
- Foa EB, Yusko DA, McLean CP, Suvak MK, Bux DA, Jr., Oslin D, et al. Concurrent naltrexone and prolonged exposure therapy for patients with comorbid alcohol dependence and PTSD: a randomized clinical trial. JAMA. 2013;310(5):488-95. Available from: https://doi.org/10.1001/jama.2013.8268
- Garland EL, Roberts-Lewis A, Tronnier CD, Graves R, Kelley K. Mindfulness-Oriented Recovery Enhancement versus CBT for co-occurring substance dependence, traumatic stress, and psychiatric disorders: Proximal outcomes from a pragmatic randomized trial. Behav Res Ther. 2016;77:7-16. Available from: https://doi.org/10.1016/j.brat.2015.11.012
- Greenfield SF, Sugarman DE, Freid CM, Bailey GL, Crisafulli MA, Kaufman JS, et al. Group therapy for women with substance use disorders: results from the Women’s Recovery Group Study. Drug Alcohol Depend. 2014;142:245-53. Available from: https://doi.org/10.1016/j.drugalcdep.2014.06.035
- Haller M, Norman SB, Cummins K, Trim RS, Xu X, Cui R, et al. Integrated Cognitive Behavioral Therapy Versus Cognitive Processing Therapy for Adults With Depression, Substance Use Disorder, and Trauma. J Subst Abuse Treat. 2016;62:38-48. Available from: https://doi.org/10.1016/j.jsat.2015.11.005
- Hien DA, Wells EA, Jiang H, Suarez-Morales L, Campbell AN, Cohen LR, et al. Multisite randomized trial of behavioral interventions for women with co-occurring PTSD and substance use disorders. J Consult Clin Psychol. 2009;77(4):607-19. Available from: https://doi.org/10.1037/a0016227
- Hoffman SN, Lyons RC, Stein MB, Taylor CT, Norman SB. Changes in positive and negative affect following prolonged exposure for PTSD comorbid with alcohol use disorder: Secondary analysis of a randomized clinical trial. Behav Res Ther. 2022;155:104097. Available from: https://doi.org/ 1016/j.brat.2022.104097
- Johnson JE, Zlotnick C. Pilot study of treatment for major depression among women prisoners with substance use disorder. J Psychiatr Res. 2012;46(9):1174-83. Available from: https://doi.org/10.1016/j.jpsychires.2012.05.007
- Kehle-Forbes SM, Chen S, Polusny MA, Lynch KG, Koffel E, Ingram E, et al. A randomized controlled trial evaluating integrated versus phased application of evidence-based psychotherapies for military veterans with comorbid PTSD and substance use disorders. Drug Alcohol Depend. 2019;205:107647. Available from: https://doi.org/10.1016/j.drugalcdep.2019.107647
- Korte KJ, Bountress KE, Tomko RL, Killeen T, Moran-Santa Maria M, Back SE. Integrated Treatment of PTSD and Substance Use Disorders: The Mediating Role of PTSD Improvement in the Reduction of Depression. J Clin Med. 2017;6(1). Available from: https://doi.org/10.3390/jcm6010009
- Kushner MG, Maurer EW, Thuras P, Donahue C, Frye B, Menary KR, et al. Hybrid cognitive behavioral therapy versus relaxation training for co-occurring anxiety and alcohol disorder: a randomized clinical trial. J Consult Clin Psychol. 2013;81(3):429-42. Available from: https://doi.org/10.1037/a0031301
- Lyons R, Panza KE, Helm J, Angkaw AC, Straus E, Norman SB. Psychosocial functioning in integrated treatment of co-occurring posttraumatic stress disorder and alcohol use disorder. J Psychiatr Res. 2021;142:40-7. Available from: https://doi.org/10.1016/j.jpsychires.2021.07.036
- McGovern MP, Lambert-Harris C, Xie H, Meier A, McLeman B, Saunders E. A randomized controlled trial of treatments for co-occurring substance use disorders and post-traumatic stress disorder. Addiction. 2015;110(7):1194-204. Available from: https://doi.org/10.1111/add.12943
- Milby JB, Schumacher JE, McNamara C, Wallace D, Usdan S, McGill T, et al. Initiating abstinence in cocaine abusing dually diagnosed homeless persons. Drug Alcohol Depend. 2000;60(1):55-67. Available from: https://doi.org/10.1016/s0376-8716(99)00139-8
- Mills KL, Teesson M, Back SE, Brady KT, Baker AL, Hopwood S, et al. Integrated exposure-based therapy for co-occurring posttraumatic stress disorder and substance dependence: a randomized controlled trial. JAMA. 2012;308(7):690-9. Available from: https://doi.org/10.1001/jama.2012.9071
- Morley KC, Baillie A, Leung S, Sannibale C, Teesson M, Haber PS. Is Specialized Integrated Treatment for Comorbid Anxiety, Depression and Alcohol Dependence Better than Treatment as Usual in a Public Hospital Setting? Alcohol Alcohol. 2016;51(4):402-9. Available from: https://doi.org/10.1093/alcalc/agv131
- Najavits LM, Krinsley K, Waring ME, Gallagher MW, Skidmore C. A Randomized Controlled Trial for Veterans with PTSD and Substance Use Disorder: Creating Change versus Seeking Safety. Subst Use Misuse. 2018;53(11):1788-800. Available from: https://doi.org/10.1080/10826084.2018.1432653
- Norman SB, Trim R, Haller M, Davis BC, Myers US, Colvonen PJ, et al. Efficacy of Integrated Exposure Therapy vs Integrated Coping Skills Therapy for Comorbid Posttraumatic Stress Disorder and Alcohol Use Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2019;76(8):791-9. Available from: https://doi.org/10.1001/jamapsychiatry.2019.0638
- O’Reilly H, Hagerty A, O’Donnell S, Farrell A, Hartnett D, Murphy E, et al. Alcohol Use Disorder and Comorbid Depression: A Randomized Controlled Trial Investigating the Effectiveness of Supportive Text Messages in Aiding Recovery. Alcohol Alcohol. 2019;54(5):551-8.
- Peck KR, Badger GJ, Cole R, Higgins ST, Moxley-Kelly N, Sigmon SC. Prolonged exposure therapy for PTSD in individuals with opioid use disorder: A randomized pilot study. Addict 2023;143:107688. Available from: https://doi.org/10.1016/j.addbeh.2023.107688
- Randall CL, Thomas S, Thevos AK. Concurrent alcoholism and social anxiety disorder: a first step toward developing effective treatments. Alcohol Clin Exp Res. 2001;25(2):210-20.
- Saavedra LM, Morgan-Lopez AA, Back SE, Patel SV, Hien DA, Killeen TK, et al. Measurement Error-Corrected Estimation of Clinically Significant Change Trajectories for Interventions Targeting Comorbid PTSD and Substance Use Disorders in OEF/OIF Veterans. Behav Ther. 2022;53(5):1009-23. Available from: https://doi.org/10.1016/j.beth.2022.04.007
- Sannibale C, Teesson M, Creamer M, Sitharthan T, Bryant RA, Sutherland K, et al. Randomized controlled trial of cognitive behaviour therapy for comorbid post-traumatic stress disorder and alcohol use disorders. Addiction. 2013;108(8):1397-410. Available from: https://doi.org/10.1111/add.12167
- Schacht RL, Brooner RK, King VL, Kidorf MS, Peirce JM. Incentivizing attendance to prolonged exposure for PTSD with opioid use disorder patients: A randomized controlled trial. J Consult Clin Psychol. 2017;85(7):689-701. Available from: https://doi.org/10.1037/ccp0000208
- Schade A, Marquenie LA, van Balkom AJ, Koeter MW, de Beurs E, van den Brink W, et al. The effectiveness of anxiety treatment on alcohol-dependent patients with a comorbid phobic disorder: a randomized controlled trial. Alcohol Clin Exp Res. 2005;29(5):794-800. Available from: https://doi.org/10.1097/01.alc.0000163511.24583.33
- Schafer I, Lotzin A, Hiller P, Sehner S, Driessen M, Hillemacher T, et al. A multisite randomized controlled trial of Seeking Safety vs. Relapse Prevention Training for women with co-occurring posttraumatic stress disorder and substance use disorders. Eur J Psychotraumatol. 2019;10(1):1577092. Available from: https://doi.org/10.1080/20008198.2019.1577092
- Schouten MJE, Goudriaan AE, Schaub MP, Dekker JJM, Blankers M. Effectiveness of a digital alcohol intervention as an add-on to depression treatment for young adults: results of a pragmatic randomized controlled trial. Psychol Med. 2024;54(11):2887-98. Available from: https://doi.org/10.1017/S0033291724000953
- Simpson TL, Kaysen DL, Fleming CB, Rhew IC, Jaffe AE, Desai S, et al. Cognitive Processing Therapy or Relapse Prevention for comorbid Posttraumatic Stress Disorder and Alcohol Use Disorder: A randomized clinical trial. PLoS One. 2022;17(11):e0276111. Available from: https://doi.org/10.1371/journal.pone.0276111
- Stapinski LA, Sannibale C, Subotic M, Rapee RM, Teesson M, Haber PS, et al. Randomised controlled trial of integrated cognitive behavioural treatment and motivational enhancement for comorbid social anxiety and alcohol use disorders. Aust N Z J Psychiatry. 2021;55(2):207-20. Available from: https://doi.org/10.1177/0004867420952539
- Stappenbeck CA, Luterek JA, Kaysen D, Rosenthal CF, Gurrad B, Simpson TL. A controlled examination of two coping skills for daily alcohol use and PTSD symptom severity among dually diagnosed individuals. Behav Res Ther. 2015;66:8-17. Available from: https://doi.org/10.1016/j.brat.2014.12.013
- Wolitzky-Taylor K, Glasner S, Tanner A, Ghahremani DG, London ED. Targeting maladaptive reactivity to negative affect in emerging adults with cannabis use disorder: A preliminary test and proof of concept. Behav Res Ther. 2022;150:104032. Available from: https://doi.org/10.1016/j.brat.2022.104032
- Zlotnick C, Johnson J, Najavits LM. Randomized controlled pilot study of cognitive-behavioral therapy in a sample of incarcerated women with substance use disorder and PTSD. Behav Ther. 2009;40(4):325-36. Available from: https://doi.org/10.1016/j.beth.2008.09.004
- Starosta AN, Leeman RF, Volpicelli JR. The BRENDA model: integrating psychosocial treatment and pharmacotherapy for the treatment of alcohol use disorders. J Psychiatr Pract. 2006;12(2):80-9. Available from: https://doi.org/10.1097/00131746-200603000-00003
- Sherwood Brown E, McArdle M, Palka J, Bice C, Ivleva E, Nakamura A, et al. A randomized, double-blind, placebo-controlled proof-of-concept study of ondansetron for bipolar and related disorders and alcohol use disorder. Eur Neuropsychopharmacol. 2021;43:92-101. Available from: https://doi.org/10.1016/j.euroneuro.2020.12.006
- Notzon DP, Mariani JJ, Pavlicova M, Glass A, Mahony AL, Brooks DJ, et al. Mixed-amphetamine salts increase abstinence from marijuana in patients with co-occurring attention-deficit/hyperactivity disorder and cocaine dependence. Am J Addict. 2016;25(8):666-72. Available from: https://doi.org/10.1111/ajad.12467
- Brooner RK, Kidorf MS, King VL, Peirce J, Neufeld K, Stoller K, et al. Managing psychiatric comorbidity within versus outside of methadone treatment settings: a randomized and controlled evaluation. Addiction. 2013;108(11):1942-51. Available from: https://doi.org/10.1111/add.12269
- Park TW, Cheng DM, Samet JH, Winter MR, Saitz R. Chronic care management for substance dependence in primary care among patients with co-occurring disorders. Psychiatr Serv. 2015;66(1):72-9. Available from: https://doi.org/10.1176/appi.ps.201300414
- Gregory RJ, Chlebowski S, Kang D, Remen AL, Soderberg MG, Stepkovitch J, et al. A controlled trial of psychodynamic psychotherapy for co-occurring borderline personality disorder and alcohol use disorder. Psychotherapy (Chic). 2008;45(1):28-41. Available from: https://doi.org/10.1037/0033-3204.45.1.28
- Philips B, Wennberg P, Konradsson P, Franck J. Mentalization-Based Treatment for Concurrent Borderline Personality Disorder and Substance Use Disorder: A Randomized Controlled Feasibility Study. Eur Addict Res. 2018;24(1):1-8. Available from: https://doi.org/10.1159/000485564
- Thylstrup B, Schroder S, Hesse M. Psycho-education for substance use and antisocial personality disorder: a randomized trial. BMC Psychiatry. 2015;15:283. Available from: https://doi.org/10.1186/s12888-015-0661-0
- Thylstrup B, Hesse M. Impulsive lifestyle counseling to prevent dropout from treatment for substance use disorders in people with antisocial personality disorder: A randomized study. Addict Behav. 2016;57:48-54. Available from: https://doi.org/10.1016/j.addbeh.2016.02.001
- van Emmerik-van Oortmerssen K, Vedel E, Kramer FJ, Blankers M, Dekker JJM, van den Brink W, et al. Integrated cognitive behavioral therapy for ADHD in adult substance use disorder patients: Results of a randomized clinical trial. Drug Alcohol Depend. 2019;197:28-36. Available from: https://doi.org/10.1016/j.drugalcdep.2018.12.023
- Brown ES, Davila D, Nakamura A, Carmody TJ, Rush AJ, Lo A, et al. A randomized, double-blind, placebo-controlled trial of quetiapine in patients with bipolar disorder, mixed or depressed phase, and alcohol dependence. Alcohol Clin Exp Res. 2014;38(7):2113-8. Available from: https://doi.org/10.1111/acer.12445
- Brown ES, Garza M, Carmody TJ. A randomized, double-blind, placebo-controlled add-on trial of quetiapine in outpatients with bipolar disorder and alcohol use disorders. J Clin Psychiatry. 2008;69(5):701-5. Available from: https://doi.org/10.4088/jcp.v69n0502
- Brown ES, Sunderajan P, Hu LT, Sowell SM, Carmody TJ. A randomized, double-blind, placebo-controlled, trial of lamotrigine therapy in bipolar disorder, depressed or mixed phase and cocaine dependence. Neuropsychopharmacology. 2012;37(11):2347-54. Available from: https://doi.org/10.1038/npp.2012.90
- Brown ES, Todd JP, Hu LT, Schmitz JM, Carmody TJ, Nakamura A, et al. A Randomized, Double-Blind, Placebo-Controlled Trial of Citicoline for Cocaine Dependence in Bipolar I Disorder. Am J Psychiatry. 2015;172(10):1014-21. Available from: https://doi.org/10.1176/appi.ajp.2015.14070857
- Gao K, Ganocy SJ, Conroy C, Brownrigg B, Serrano MB, Calabrese JR. A placebo controlled study of quetiapine-XR in bipolar depression accompanied by generalized anxiety with and without a recent history of alcohol and cannabis use. Psychopharmacology (Berl). 2017;234(15):2233-44. Available from: https://doi.org/10.1007/s00213-017-4642-5
- Hollander E, Pallanti S, Allen A, Sood E, Baldini Rossi N. Does sustained- release lithium reduce impulsive gambling and affective instability versus placebo in pathological gamblers with bipolar spectrum disorders? Am J Psychiatry. 2005;162(1):137-45. Available from: https://doi.org/10.1176/appi.ajp.162.1.137
- Nejtek VA, Avila M, Chen LA, Zielinski T, Djokovic M, Podawiltz A, et al. Do atypical antipsychotics effectively treat co-occurring bipolar disorder and stimulant dependence? A randomized, double-blind trial. J Clin Psychiatry. 2008;69(8):1257-66. Available from: https://doi.org/10.4088/jcp.v69n0808
- Salloum IM, Cornelius JR, Daley DC, Kirisci L, Himmelhoch JM, Thase ME. Efficacy of valproate maintenance in patients with bipolar disorder and alcoholism: a double-blind placebo-controlled study. Arch Gen Psychiatry. 2005;62(1):37-45. Available from: https://doi.org/10.1001/archpsyc.62.1.37
- Stedman M, Pettinati HM, Brown ES, Kotz M, Calabrese JR, Raines S. A double-blind, placebo-controlled study with quetiapine as adjunct therapy with lithium or divalproex in bipolar I patients with coexisting alcohol dependence. Alcohol Clin Exp Res. 2010;34(10):1822-31. Available from: https://doi.org/10.1111/j.1530-0277.2010.01270.x
- Tolliver BK, Desantis SM, Brown DG, Prisciandaro JJ, Brady KT. A randomized, double-blind, placebo-controlled clinical trial of acamprosate in alcohol-dependent individuals with bipolar disorder: a preliminary report. Bipolar Disord. 2012;14(1):54-63. Available from: https://doi.org/10.1111/j.1399-5618.2011.00973.x
- Brunette MF, Correll CU, O’Malley SS, McDonnell D, DiPetrillo L, Jiang Y, et al. Olanzapine Plus Samidorphan (ALKS 3831) in Schizophrenia and Comorbid Alcohol Use Disorder: A Phase 2, Randomized Clinical Trial. J Clin Psychiatry. 2020;81(2). Available from: https://doi.org/10.4088/JCP.19m12786
- Green AI, Brunette MF, Dawson R, Buckley P, Wallace AE, Hafez H, et al. Long-acting injectable vs oral risperidone for schizophrenia and co-occurring alcohol use disorder: a randomized trial. J Clin Psychiatry. 2015;76(10):1359-65. Available from: https://doi.org/10.4088/JCP.13m08838
- Adamson SJ, Sellman JD, Foulds JA, Frampton CM, Deering D, Dunn A, et al. A randomized trial of combined citalopram and naltrexone for nonabstinent outpatients with co-occurring alcohol dependence and major depression. J Clin Psychopharmacol. 2015;35(2):143-9. Available from: https://doi.org/10.1097/JCP.0000000000000287
- Carpenter KM, Brooks AC, Vosburg SK, Nunes EV. The effect of sertraline and environmental context on treating depression and illicit substance use among methadone maintained opiate dependent patients: a controlled clinical trial. Drug Alcohol Depend. 2004;74(2):123-34. Available from: https://doi.org/10.1016/j.drugalcdep.2003.11.015
- Cornelius JR, Salloum IM, Ehler JG, Jarrett PJ, Cornelius MD, Perel JM, et al. Fluoxetine in depressed alcoholics. A double-blind, placebo-controlled trial. Arch Gen Psychiatry. 1997;54(8):700-5. Available from: https://doi.org/10.1001/archpsyc.1997.01830200024004
- Gual A, Balcells M, Torres M, Madrigal M, Diez T, Serrano L. Sertraline for the prevention of relapse in detoxicated alcohol dependent patients with a comorbid depressive disorder: a randomized controlled trial. Alcohol Alcohol. 2003;38(6):619-25. Available from: https://doi.org/10.1093/alcalc/agg124
- Han DH, Kim SM, Choi JE, Min KJ, Renshaw PF. Adjunctive aripiprazole therapy with escitalopram in patients with co-morbid major depressive disorder and alcohol dependence: clinical and neuroimaging evidence. J Psychopharmacol. 2013;27(3):282-91. Available from: https://doi.org/ 1177/0269881112472563
- Hernandez-Avila CA, Modesto-Lowe V, Feinn R, Kranzler HR. Nefazodone treatment of comorbid alcohol dependence and major depression. Alcohol Clin Exp Res. 2004;28(3):433-40. Available from: https://doi.org/10.1097/01.alc.0000118313.63897.ee
- Kleber HD, Weissman MM, Rounsaville BJ, Wilber CH, Prusoff BA, Riordan CE. Imipramine as treatment for depression in addicts. Arch Gen Psychiatry. 1983;40(6):649-53. Available from: https://doi.org/10.1001/archpsyc.1983.04390010059007
- Kranzler HR, Mueller T, Cornelius J, Pettinati HM, Moak D, Martin PR, et al. Sertraline treatment of co-occurring alcohol dependence and major depression. J Clin Psychopharmacol. 2006;26(1):13-20. Available from: https://doi.org/10.1097/01.jcp.0000194620.61868.35
- Levin FR, Mariani J, Brooks DJ, Pavlicova M, Nunes EV, Agosti V, et al. A randomized double-blind, placebo-controlled trial of venlafaxine-extended release for co-occurring cannabis dependence and depressive disorders. Addiction. 2013;108(6):1084-94. Available from: https://doi.org/10.1111/add.12108
- McDowell D, Nunes EV, Seracini AM, Rothenberg J, Vosburg SK, Ma GJ, et al. Desipramine treatment of cocaine-dependent patients with depression: a placebo-controlled trial. Drug Alcohol Depend. 2005;80(2):209-21. Available from: https://doi.org/10.1016/j.drugalcdep.2005.03.026
- McGrath PJ, Nunes EV, Stewart JW, Goldman D, Agosti V, Ocepek-Welikson K, et al. Imipramine treatment of alcoholics with primary depression: A placebo-controlled clinical trial. Arch Gen Psychiatry. 1996;53(3):232-40. Available from: https://doi.org/10.1001/archpsyc.1996.01830030054009
- Moak DH, Anton RF, Latham PK, Voronin KE, Waid RL, Durazo-Arvizu R. Sertraline and cognitive behavioral therapy for depressed alcoholics: results of a placebo-controlled trial. J Clin Psychopharmacol. 2003;23(6):553-62. Available from: https://doi.org/10.1097/01.jcp.0000095346.32154.41
- Muhonen LH, Lahti J, Sinclair D, Lonnqvist J, Alho H. Treatment of alcohol dependence in patients with co-morbid major depressive disorder-predictors for the outcomes with memantine and escitalopram medication. Subst Abuse Treat Prev Policy. 2008;3:20. Available from: https://doi.org/10.1186/1747-597X-3-20
- Muhonen LH, Lonnqvist J, Juva K, Alho H. Double-blind, randomized comparison of memantine and escitalopram for the treatment of major depressive disorder comorbid with alcohol dependence. J Clin Psychiatry. 2008;69(3):392-9. Available from: https://doi.org/10.4088/jcp.v69n0308
- Nunes EV, Quitkin FM, Donovan SJ, Deliyannides D, Ocepek-Welikson K, Koenig T, et al. Imipramine treatment of opiate-dependent patients with depressive disorders. A placebo-controlled trial. Arch Gen Psychiatry. 1998;55(2):153-60. Available from: https://doi.org/10.1001/archpsyc.55.2.153
- Petrakis I, Carroll KM, Nich C, Gordon L, Kosten T, Rounsaville B. Fluoxetine treatment of depressive disorders in methadone-maintained opioid addicts. Drug Alcohol Depend. 1998;50(3):221-6. Available from: https://doi.org/10.1016/s0376-8716(98)00032-5
- Pettinati HM, Oslin DW, Kampman KM, Dundon WD, Xie H, Gallis TL, et al. A double-blind, placebo-controlled trial combining sertraline and naltrexone for treating co-occurring depression and alcohol dependence. Am J Psychiatry. 2010;167(6):668-75. Available from: https://doi.org/10.1176/appi.ajp.2009.08060852
- Raby WN, Rubin EA, Garawi F, Cheng W, Mason E, Sanfilippo L, et al. A randomized, double-blind, placebo-controlled trial of venlafaxine for the treatment of depressed cocaine-dependent patients. Am J Addict. 2014;23(1):68-75. Available from: https://doi.org/10.1111/j.1521-0391.2013.12065.x
- Roy-Byrne PP, Pages KP, Russo JE, Jaffe C, Blume AW, Kingsley E, et al. Nefazodone treatment of major depression in alcohol-dependent patients: a double-blind, placebo-controlled trial. J Clin Psychopharmacol. 2000;20(2):129-36. Available from: https://doi.org/ 1097/00004714-200004000-00003
- Schmitz JM, Averill P, Stotts AL, Moeller FG, Rhoades HM, Grabowski J. Fluoxetine treatment of cocaine-dependent patients with major depressive disorder. Drug Alcohol Depend. 2001;63(3):207-14. Available from: https://doi.org/10.1016/s0376-8716(00)00208-8
- Book SW, Thomas SE, Randall PK, Randall CL. Paroxetine reduces social anxiety in individuals with a co-occurring alcohol use disorder. J Anxiety Disord. 2008;22(2):310-8. Available from: https://doi.org/10.1016/j.janxdis.2007.03.001
- Malcolm R, Anton RF, Randall CL, Johnston A, Brady K, Thevos A. A placebo-controlled trial of buspirone in anxious inpatient alcoholics. Alcohol Clin Exp Res. 1992;16(6):1007-13. Available from: https://doi.org/10.1111/j.1530-0277.1992.tb00691.x
- Thomas SE, Randall PK, Book SW, Randall CL. A complex relationship between co-occurring social anxiety and alcohol use disorders: what effect does treating social anxiety have on drinking? Alcohol Clin Exp Res. 2008;32(1):77-84. Available from: https://doi.org/10.1111/j.1530-0277.2007.00546.x
- Back SE, Flanagan JC, Mintz J, Brady KT, Jones J, Jarnecke AM, et al. A Double-Blind Randomized Controlled Trial of Doxazosin for Co-Occurring PTSD and Alcohol Use Disorder in Veterans. J Clin Psychiatry. 2023;84(2):08. Available from: https://doi.org/10.4088/JCP.21m14367
- Batki SL, Pennington DL, Lasher B, Neylan TC, Metzler T, Waldrop A, et al. Topiramate treatment of alcohol use disorder in veterans with posttraumatic stress disorder: a randomized controlled pilot trial. Alcohol Clin Exp Res. 2014;38(8):2169-77. Available from: https://doi.org/10.1111/acer.12496
- Hien DA, Levin FR, Ruglass LM, Lopez-Castro T, Papini S, Hu MC, et al. Combining seeking safety with sertraline for PTSD and alcohol use disorders: A randomized controlled trial. J Consult Clin Psychol. 2015;83(2):359-69. Available from: https://doi.org/10.1037/a0038719
- Petrakis IL, Desai N, Gueorguieva R, Arias A, O’Brien E, Jane JS, et al. Prazosin for Veterans with Posttraumatic Stress Disorder and Comorbid Alcohol Dependence: A Clinical Trial. Alcohol Clin Exp Res. 2016;40(1):178-86. Available from: https://doi.org/10.1111/acer.12926
- Simpson TL, Malte CA, Dietel B, Tell D, Pocock I, Lyons R, et al. A pilot trial of prazosin, an alpha-1 adrenergic antagonist, for comorbid alcohol dependence and posttraumatic stress disorder. Alcohol Clin Exp Res. 2015;39(5):808-17. Available from: https://doi.org/10.1111/acer.12703
- Davis LL, Petrakis IL, Pilkinton PD, Nolen T, Vandergrift N, Hirsch S, et al. Comorbid alcohol use disorder and posttraumatic stress disorder: A proof-of-concept randomized placebo-controlled trial of buprenorphine and naltrexone combination treatment. Alcohol Clin Exp Res (Hoboken). 2023;47(9):1756-72. Available from: https://doi.org/10.1111/acer.15155
- Konstenius M, Jayaram-Lindström N, Guterstam J, Beck O, Philips B, Franck J. ‘Methylphenidate for attention deficit hyperactivity disorder and drug relapse in criminal offenders with substance dependence: A 24-week randomized placebo-controlled trial’: Corrigendum. 2014;109(9):1571-2.
- Levin FR, Evans SM, Brooks DJ, Garawi F. Treatment of cocaine dependent treatment seekers with adult ADHD: double-blind comparison of methylphenidate and placebo. Drug Alcohol Depend. 2007;87(1):20-9. Available from: https://doi.org/10.1016/j.drugalcdep.2006.07.004
- Levin FR, Evans SM, Brooks DJ, Kalbag AS, Garawi F, Nunes EV. Treatment of methadone-maintained patients with adult ADHD: double-blind comparison of methylphenidate, bupropion and placebo. Drug Alcohol Depend. 2006;81(2):137-48. Available from: https://doi.org/10.1016/j.drugalcdep.2005.06.012
- Levin FR, Mariani JJ, Specker S, Mooney M, Mahony A, Brooks DJ, et al. Extended-Release Mixed Amphetamine Salts vs Placebo for Comorbid Adult Attention-Deficit/Hyperactivity Disorder and Cocaine Use Disorder: A Randomized Clinical Trial. JAMA Psychiatry. 2015;72(6):593-602. Available from: https://doi.org/10.1001/jamapsychiatry.2015.41
- Schubiner H, Saules KK, Arfken CL, Johanson CE, Schuster CR, Lockhart N, et al. Double-blind placebo-controlled trial of methylphenidate in the treatment of adult ADHD patients with comorbid cocaine dependence. Exp Clin Psychopharmacol. 2002;10(3):286-94. Available from: https://doi.org/10.1037//1064-1297.10.3.286
- Wilens TE, Adler LA, Weiss MD, Michelson D, Ramsey JL, Moore RJ, et al. Atomoxetine treatment of adults with ADHD and comorbid alcohol use disorders. Drug Alcohol Depend. 2008;96(1-2):145-54. Available from: https://doi.org/10.1016/j.drugalcdep.2008.02.009
- Rains LS, Marston L, Hinton M, Marwaha S, Craig T, Fowler D, et al. Clinical and cost-effectiveness of contingency management for cannabis use in early psychosis: The CIRCLE randomised clinical trial. BMC Medicine. 2019;17(1). Available from: https://doi.org/10.1186/s12916-019-1395-5
- Petrakis IL, O’Malley S, Rounsaville B, Poling J, McHugh-Strong C, Krystal JH, et al. Naltrexone augmentation of neuroleptic treatment in alcohol abusing patients with schizophrenia. Psychopharmacology (Berl). 2004;172(3):291-7. Available from: https://doi.org/10.1007/s00213-003-1658-9
- Ralevski E, Balachandra K, Gueorguieva R, Limoncelli D, Petrakis I. Effects of naltrexone on cognition in a treatment study of patients with schizophrenia and comorbid alcohol dependence. J Dual Diagn. 2006;2(4):53-69. Available from: https://doi.org/10.1300/J374v02n04_05
- Petrakis IL, Poling J, Levinson C, Nich C, Carroll K, Rounsaville B, et al. Naltrexone and disulfiram in patients with alcohol dependence and comorbid psychiatric disorders. Biol Psychiatry. 2005;57(10):1128-37. Available from: https://doi.org/10.1016/j.biopsych.2005.02.016
- Drake RE, McHugo GJ, Clark RE, Teague GB, Xie H, Miles K, et al. Assertive community treatment for patients with co-occurring severe mental illness and substance use disorder: a clinical trial. Am J Orthopsychiatry. 1998;68(2):201-15. Available from: https://doi.org/10.1037/h0080330
- Essock SM, Mueser KT, Drake RE, Covell NH, McHugo GJ, Frisman LK, et al. Comparison of ACT and standard case management for delivering integrated treatment for co-occurring disorders. Psychiatr Serv. 2006;57(2):185-96. Available from: https://doi.org/10.1176/appi.ps.57.2.185
- Clayton A, O’Connell MJ, Bellamy C, Benedict P, Rowe M. The Citizenship Project part II: impact of a citizenship intervention on clinical and community outcomes for persons with mental illness and criminal justice involvement. Am J Community Psychol. 2013;51(1-2):114-22. Available from: https://doi.org/10.1007/s10464-012-9549-z
- Murphy SM, McDonell MG, McPherson S, Srebnik D, Angelo F, Roll JM, et al. An economic evaluation of a contingency-management intervention for stimulant use among community mental health patients with serious mental illness. Drug Alcohol Depend. 2015;153:293-9. Available from: https://doi.org/10.1016/j.drugalcdep.2015.05.004
- Clark RE, Teague GB, Ricketts SK, Bush PW, Xie H, McGuire TG, et al. Cost-effectiveness of assertive community treatment versus standard case management for persons with co-occurring severe mental illness and substance use disorders. Health Serv Res. 1998;33(5 Pt 1):1285-308.
- Clark RE, Ricketts SK, McHugo GJ. Legal system involvement and costs for persons in treatment for severe mental illness and substance use disorders. Psychiatr Serv. 1999;50(5):641-7. Available from: https://doi.org/10.1176/ps.50.5.641
- de Waal MM, Blankers M, Lommerse NM, Kikkert MJ, Dekker JJM, Goudriaan AE. Economic Evaluation of the SOS Training to Reduce Victimization in Dual Diagnosis Patients. J Dual Diagn. 2021;17(4):333-43. Available from: https://doi.org/10.1080/15504263.2021.1965409
- French MT, Sacks S, De Leon G, Staines G, McKendrick K. Modified therapeutic community for mentally ill chemical abusers: outcomes and costs. Eval Health Prof. 1999;22(1):60-85. Available from: https://doi.org/10.1177/016327879902200104
- McGeary KA, French MT, Sacks S, McKendrick K, De Leon G. Service use and cost by mentally ill chemical abusers: differences by retention in a therapeutic community. J Subst Abuse. 2000;11(3):265-79. Available from: https://doi.org/10.1016/s0899-3289(00)00026-2
- Morse GA, Calsyn RJ, Dean Klinkenberg W, Helminiak TW, Wolff N, Drake RE, et al. Treating homeless clients with severe mental illness and substance use disorders: costs and outcomes. Community Ment Health J. 2006;42(4):377-404. Available from: https://doi.org/10.1007/s10597-006-9050-y
- Joshi K, Lafeuille MH, Kamstra R, Tiggelaar S, Lefebvre P, Kim E, et al. Real-world adherence and economic outcomes associated with paliperidone palmitate versus oral atypical antipsychotics in schizophrenia patients with substance-related disorders using Medicaid benefits. J Comp Eff Res. 2018;7(2):121-33. Available from: https://doi.org/10.2217/cer-2017-0043
- Lefebvre P, Muser E, Joshi K, DerSarkissian M, Bhak RH, Duh MS, et al. Impact of Paliperidone Palmitate Versus Oral Atypical Antipsychotics on Health Care Resource Use and Costs in Veterans With Schizophrenia and Comorbid Substance Abuse. Clin Ther. 2017;39(7):1380-95 e4. Available from: https://doi.org/10.1016/j.clinthera.2017.05.356
- Olsson TM, Fridell M. Women with comorbid substance dependence and psychiatric disorders in Sweden: a longitudinal study of hospital care utilization and costs. BMC Health Serv Res. 2015;15:224. Available from: https://doi.org/10.1186/s12913-015-0873-5
- Sök räntor och valutakurser. Stockholm: Sveriges Riksbank. Available from: https://www.riksbank.se/sv/statistik/rantor-och-valutakurser/sok-rantor-och-valutakurser/
- Pris- och beslutsdatabasen. Tandvårds- och Läkemedelsförmånsverket (TLV). [accessed Nov 22 2023]. Available from: https://www.tlv.se/beslut/sok-priser-och-beslut-i-databasen.html
- Gralén K, Hjalte F, Persson U. Hälso- och sjukvårdsuppgifternas utveckling i Sverige. Lund: Institutet för Hälso- och Sjukvårdsekonomi (IHE). IHE Rapport 5. [accessed Sep 12 2023]. Available from: https://ihe.se/app/uploads/2019/09/IHE-Rapport-2019_5_.pdf
- Lafeuille MH, Dean J, Fastenau J, Panish J, Olson W, Markowitz M, et al. Burden of schizophrenia on selected comorbidity costs. Expert Rev Pharmacoecon Outcomes Res. 2014;14(2):259-67. Available from: https://doi.org/10.1586/14737167.2014.894463
- Ding K, Yang J, Cheng G, Schiltz T, Summers KM, Skinstad AH. Hospitalizations and hospital charges for co-occurring substance use and mental disorders. J Subst Abuse 2011;40(4):366-75. Available from: https://doi.org/10.1016/j.jsat.2010.12.005
- Dickey B, Azeni H. Persons with dual diagnoses of substance abuse and major mental illness: their excess costs of psychiatric care. Am J Public Health. 1996;86(7):973-7. Available from: https://doi.org/10.2105/ajph.86.7.973
- Clark RE, Samnaliev M, McGovern MP. Impact of substance disorders on medical expenditures for medicaid beneficiaries with behavioral health disorders. Psychiatr Serv. 2009;60(1):35-42. Available from: https://doi.org/10.1176/ps.2009.60.1.35
- Graham K, Cheng J, Bernards S, Wells S, Rehm J, Kurdyak P. How Much Do Mental Health and Substance Use/Addiction Affect Use of General Medical Services? Extent of Use, Reason for Use, and Associated Costs. Can J Psychiatry. 2017;62(1):48-56. Available from: https://doi.org/10.1177/0706743716664884
- Libutzki B, Ludwig S, May M, Jacobsen RH, Reif A, Hartman CA. Direct medical costs of ADHD and its comorbid conditions on basis of a claims data analysis. Eur Psychiatry. 2019;58:38-44. Available from: https://doi.org/10.1016/j.eurpsy.2019.01.019
- Snow KJ, Petrie D, Young JT, Preen DB, Heffernan E, Kinner SA. Impact of dual diagnosis on healthcare and criminal justice costs after release from Queensland prisons: a prospective cohort study. Aust J Prim Health. 2022;28(3):264-70. Available from: https://doi.org/10.1071/PY21142
- Olsson TM, Fridell M. Women with co-occurring substance abuse and mental disorders in Sweden: a longitudinal study of criminal justice system involvement and costs. Mental Health and Substance Use. 2013;6(3):219-36. Available from: https://doi.org/10.1080/17523281.2012.708356
- Olsson TM. Productivity loss, victim costs and the intangible costs of crime: Followup to a longitudinal study of criminal justice system involvement and costs of women with co-occurring substance abuse and mental disorders in Sweden. Mental Health and Substance Use: Dual Diagnosis. 2014;7(2):102-9. Available from: https://doi.org/10.1080/17523281.2013.806344
- Clark RE. Family costs associated with severe mental illness and substance use. Hosp Community Psychiatry. 1994;45(8):808-13. Available from: https://doi.org/10.1176/ps.45.8.808
- Roberts J, Lenton P, Keetharuth AD, Brazier J. Quality of life impact of mental health conditions in England: results from the adult psychiatric morbidity surveys. Health Qual Life Outcomes. 2014;12:6. Available from: https://doi.org/10.1186/1477-7525-12-6
- Wittenberg E, Barbosa C, Hein R, Hudson E, Thornburg B, Bray JW. Health-related quality of life of alcohol use disorder with co-occurring conditions in the US population. Drug Alcohol Depend. 2021;221:108558. Available from: https://doi.org/10.1016/j.drugalcdep.2021.108558
- Uppsala: Läkemedelsverket. [updated Dec 15 2023]. Available from: https://www.lakemedelsverket.se/sv/behandling-och-forskrivning/utbytbara-lakemedel/utbytbarhetslista#contactInformation
- Destoop M, Docx L, Morrens M, Dom G. Meta-Analysis on the Effect of Contingency Management for Patients with Both Psychotic Disorders and Substance Use Disorders. J Clin Med. 2021;10(4):616. Available from: https://doi.org/10.3390/jcm10040616
- Israelsson M, Gerdner A. Internationell utblick på tvångsvård vid substansmissbruk. In: Dahlin M, Juth N, Sjöström S, editors. Tvång på gott och ont; 2025. p. 221-42.
- Lagrådsremiss En förebyggande socialtjänstlag – för ökade rättigheter, skyldigheter och möjligheter. Stockholm. [updated Jul 4 2024; accessed Apr 11 2025]. Available from: https://www.regeringen.se/rattsliga-dokument/lagradsremiss/2024/07/en-forebyggande-socialtjanstlag--for-okade-rattigheter-skyldigheter-och-mojligheter/
- Sjöstrand L. Bellmans diktning rör vid själva livsnerven i alkoholbruket. Läkartidningen. 1990;87:26-7.
- Album D. [The prestige of diseases and medical specialties]. Tidsskr Nor Laegeforen. 1991;111(17):2127-33.
- Gehlert S, Mozersky J. Seeing Beyond the Margins: Challenges to Informed Inclusion of Vulnerable Populations in Research. J Law Med Ethics. 2018;46(1):30-43. Available from: https://doi.org/10.1177/1073110518766006
- Bejerot S. Vår behandling kan rädda liv men kanske får vi aldrig veta. DN debatt 2025-01-22. [accessed Apr 11 2025]. Available from: dn.se/debatt/var-behandling-kan-radda-liv-men-kanske-far-vi-aldrig-veta/
- Prioriterade utfall, Core Outcome set (COS). Stockholm: Statens beredning för medicinsk och social utvärdering (SBU). [accessed Apr 11 2025]. Available from: https://www.sbu.se/sv/metod/core-outcome-set-cos-en-lista-av-centrala-utfall/
- Bethesda: The National Institute of Mental Health. [accessed March 19]. Available from: https://www.nimh.nih.gov/health/statistics/mental-illness
- Ruggeri M, Leese M, Thornicroft G, Bisoffi G, Tansella M. Definition and prevalence of severe and persistent mental illness. Br J Psychiatry. 2000;177(2):149-55. Available from: https://doi.org/10.1192/bjp.177.2.149
- World Health Organization. The ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research. World Health Organization (WHO); 1993. [accessed Apr 16 2025]. Available from: https://iris.who.int/handle/10665/37108
- Engel PA, Engel AG. George L. Engel 1913-1999: remembering his life and work: strengthening a father-son bond in a new time of grief. Aust N Z J Psychiatry. 2002;36(4):443-8. Available from: https://doi.org/10.1046/j.1440-1614.2001.01029.x
- Nationell utvärdering av vård och stöd vid schizofreni och schizofreniliknande tillstånd – 2022. Huvudrapport med förbättringsområden. Stockholm: Socialstyrelsen; 2022. Artikelnummer: 2022-8-8072. [accessed Apr 11 2025]. Available from: https://www.socialstyrelsen.se/kunskapsstod-och-regler/regler-och-riktlinjer/nationella-riktlinjer/riktlinjer-och-utvarderingar/schizofreni/
- Vård som inte bör göras. Följsamhet till nationella riktlinjer. Stockholm: Socialstyrelsen; 2023. Artikelnummer: 2023-11-8818. [accessed Apr 11 2025]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/nationella-riktlinjer/2023-11-8818.pdf
- SFS 1991:1128. Lag om psykiatrisk tvångsvård. Svensk författningssamling. Stockholm: Riksdagen. [accessed Apr 11 2024]. Available from: https://www.riksdagen.se/sv/dokument-och-lagar/dokument/svensk-forfattningssamling/lag-19911128-om-psykiatrisk-tvangsvard_sfs-1991-1128/
- Gagnon M, Payne A, Guta A. What are the ethical implications of using prize-based contingency management in substance use? A scoping review. Harm Reduct J. 2021;18(1):82. Available from: https://doi.org/10.1186/s12954-021-00529-w
- Tiet QQ, Mausbach B. Treatments for patients with dual diagnosis: a review. Alcohol Clin Exp Res. 2007;31(4):513-36. Available from: https://doi.org/10.1111/j.1530-0277.2007.00336.x
- Schramm E, Klein DN, Elsaesser M, Furukawa TA, Domschke K. Review of dysthymia and persistent depressive disorder: history, correlates, and clinical implications. Lancet Psychiatry. 2020;7(9):801-12. Available from: https://doi.org/10.1016/S2215-0366(20)30099-7
- Agabio R, Trogu E, Pani PP. Antidepressants for the treatment of people with co-occurring depression and alcohol dependence. Cochrane Database Syst Rev. 2018;4(4):CD008581. Available from: https://doi.org/10.1002/14651858.CD008581.pub2
- Gold AK, Otto MW, Deckersbach T, Sylvia LG, Nierenberg AA, Kinrys G. Substance use comorbidity in bipolar disorder: A qualitative review of treatment strategies and outcomes. Am J Addict. 2018;27(3):188-201. Available from: https://doi.org/10.1111/ajad.12713
- Grant S, Azhar G, Han E, Booth M, Motala A, Larkin J, et al. Clinical interventions for adults with comorbid alcohol use and depressive disorders: A systematic review and network meta-analysis. PLOS Medicine. 2021;18(10):e1003822. Available from: https://doi.org/10.1371/journal.pmed.1003822
- Ipser JC, Wilson D, Akindipe TO, Sager C, Stein DJ. Pharmacotherapy for anxiety and comorbid alcohol use disorders. Cochrane Database Syst Rev. 2015;1(1):Cd007505. Available from: https://doi.org/10.1002/14651858.CD007505.pub2
- Stokes PRA, Jokinen T, Amawi S, Qureshi M, Husain MI, Yatham LN, et al. Pharmacological Treatment of Mood Disorders and Comorbid Addictions: A Systematic Review and Meta-Analysis: Traitement Pharmacologique des Troubles de L’humeur et des Dependances Comorbides: Une Revue Systematique et une Meta-Analyse. Can J Psychiatry. 2020;65(11): 749-69. Available from: https://doi.org/10.1177/0706743720915420
- Temmingh HS, Williams T, Siegfried N, Stein DJ. Risperidone versus other antipsychotics for people with severe mental illness and co-occurring substance misuse. Cochrane Database Syst Rev. 2018;1(1):CD011057. Available from: https://doi.org/10.1002/14651858.CD011057.pub2
- Hien DA, Papini S, Saavedra LM, Bauer AG, Ruglass LM, Ebrahimi CT, et al. Project harmony: A systematic review and network meta-analysis of psychotherapy and pharmacologic trials for comorbid posttraumatic stress, alcohol, and other drug use disorders. Psychol Bull. 2024;150(3):319-53. Available from: https://doi.org/10.1037/bul0000409
- The COMET Initiative database Liverpool: The COMET Initiative. [accessed Jan 13 2022]. Available from: https://www.comet-initiative.org/Resources/Database
- Karnik NS, Marsden J, McCluskey C, Boley RA, Bradley KA, Campbell CI, et al. The opioid use disorder core outcomes set (OUD-COS) for treatment research: findings from a Delphi consensus study. Addiction. 2022;117(9):2438-47. Available from: https://doi.org/10.1111/add.15875
- Retzer A, Sayers R, Pinfold V, Gibson J, Keeley T, Taylor G, et al. Development of a core outcome set for use in community-based bipolar trials-A qualitative study and modified Delphi. PLoS One. 2020;15(10):e0240518. Available from: https://doi.org/10.1371/journal.pone.0240518
- Witkiewitz K, Hallgren KA, Kranzler HR, Mann KF, Hasin DS, Falk DE, et al. Clinical Validation of Reduced Alcohol Consumption After Treatment for Alcohol Dependence Using the World Health Organization Risk Drinking Levels. Alcohol Clin Exp Res. 2017;41(1):179-86. Available from: https://doi.org/10.1111/acer.13272
- Witkiewitz K, Kranzler HR, Hallgren KA, O’Malley SS, Falk DE, Litten RZ, et al. Drinking Risk Level Reductions Associated with Improvements in Physical Health and Quality of Life Among Individuals with Alcohol Use Disorder. Alcohol Clin Exp Res. 2018;42(12):2453-65. Available from: https://doi.org/10.1111/acer.13897
- Witkiewitz K, Heather N, Falk DE, Litten RZ, Hasin DS, Kranzler HR, et al. World Health Organization risk drinking level reductions are associated with improved functioning and are sustained among patients with mild, moderate and severe alcohol dependence in clinical trials in the United States and United Kingdom. Addiction. 2020;115(9):1668-80. Available from: https://doi.org/10.1111/add.15011
- Dyer A, Böhnke JR, Curran D, McGrath K, Toner P. A systematic review of quality of life and health-related quality of life as outcomes in substance and behavioural addictions. Drug Alcohol Rev. 2023;42(7):1680-700. Available from: https://doi.org/10.1111/dar.13717

 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services
 Share on Facebook
Share on Facebook
 Share on LinkedIn
Share on LinkedIn
 Share via Email
Share via Email