Continuity of care
A systematic review and assessment of medical, economic, social and ethical aspects
Conclusions
When comparing higher to lower relational continuity of care, the following findings were made:
For persons with asthma or chronic obstructive pulmonary disease (COPD), higher relational continuity of care leads to:
- Lower risk of premature death (low certainty of evidence)
- Lower risk of hospitalisation to a moderate to high degree (moderate certainty of evidence)
- Lower risk of emergency department visits (low certainty of evidence)
- Lower healthcare costs (low certainty of evidence).
For persons with asthma or COPD, health economic scenario analyses based on the results for health care resource use indicate that higher relational continuity of care leads to:
- 30–60 % fewer hospitalisations. In Sweden, this could imply savings for hospitalisations in the order of 235–470 million Swedish crowns per year.
- 10–60 % fewer emergency department visits. In Sweden, this could imply savings for this type of visit in the order of 16–100 million Swedish crowns per year.
For persons with severe mental illness, higher relational continuity of care leads to:
- Lower risk of premature death (low certainty of evidence)
- Lower risk of emergency department visits (low certainty of evidence)
- Improved quality of life (low certainty of evidence).
For persons with severe mental illness, health economic scenario analyses based on the results for health care resource use indicate that higher relational continuity of care leads to:
- 5–15 % fewer emergency department visits. In Sweden, this could imply savings for this type of visit in the order of 2–7 million Swedish crowns per year.
The estimations of resource use and related changes in costs should be seen as examples of what improved relational continuity of care could imply in a Swedish context, rather than as basis for long term forecasts or transfers to persons with other chronic diseases. The cost estimates are sensitive to changes in the organisation of care and over time, and do not include costs in other care segments.
For persons with asthma or COPD, the importance of relational continuity for adherence to pharmacological treatment and for the experience of care and self-management of the disease cannot be assessed based on the scientific literature.
For persons with severe mental illness, the importance of relational continuity for the risk of hospitalisation, health care costs, symptoms and functioning, as well as adherence to pharmacological treatment cannot be assessed based on the scientific literature.
Background
Relational continuity implies that a patient and their physician or other health care personnel have contact over a longer period of time, providing opportunity to develop a mutual care relationship. Having high relational continuity may be of particular value for patients with chronic conditions.
Aim
The aim of this systematic review was to investigate treatment outcomes associated with receiving higher relational continuity of care for two patient groups whose problems are long term and treatment-intensive: patients with asthma or chronic obstructive pulmonary disease (COPD), and patients with severe mental illness, which includes schizophrenia, bipolar disorder, and severe depression.
Method
Two systematic reviews were conducted in accordance with the PRISMA statement. Moreover, health economic and ethical aspects were assessed.
Based on the studies’ measurement of relational continuity, results were synthesised as a comparison between higher and lower continuity. Due to the included studies’ design, it was not possible to further quantify the degree of relational continuity. Different outcome measures for relational continuity were grouped into categories, and the project team formulated synthesised results based on the evidence. The certainty of evidence was assessed using GRADE’s methodology.
The health economic scenario analyses were based on the results for resource use where the certainty of evidence was deemed low, moderate, or high. In international comparisons with other OECD-countries, Swedish health care has shown shortcomings in continuity of care. Thus, the report’s health economic scenario analyses were based on the assumption that the current situation can be improved upon. National and regional registry data were used to estimate current costs for hospitalisations and emergency department visits in the relevant populations in Sweden. The effect of higher compared to lower relational continuity on resulting costs was investigated in scenario analyses. The risk reduction used in the scenario analyses was based on the range of results for the relevant outcome measures in the systematic review. The evaluation did not assess what is required to establish higher relational continuity of care or what changes in resource allocation this would require.
The protocol was registered in Prospero.
Inclusion criteria (PICOs)
Population
Persons with asthma and/or COPD. Persons with severe mental illness/severe mental disorder (schizophrenia, bipolar disorder, or severe depression/severe episode of major depressive disorder).
Intervention/Exposure
Several different measures of continuity exist and there was no restriction in terms of certain definitions, provided that the measure actually assesses some aspect of relational continuity. Known indices of continuity were accepted as well as sound other measures of the dimensions mentioned.
Control
For clinical studies comparing groups: different levels of continuity should be compared (including no continuity). For observational study data: study of associations between levels of continuity and outcome(s) using adequate methods.
Outcomes
Mortality (all causes and disease specific). Morbidity outcomes, such as assessments of symptoms and or functioning using validated instruments. Economic measures: emergency department visits, hospital admissions, costs of care. Adherence to prescribed medication. For the population clinically relevant laboratory measures. Subjective measures: patient satisfaction, quality of life.
Study design
Observational studies, randomised controlled trials.
Language: English, Swedish, Danish, or Norwegian.
Search period: From 2000 to 2020. Final search February 2021.
Databases searched: CINAHL, Medline, PsycINFO, Scopus, Embase, Cochrane Library, Database of Systematic Review of Effects, DARE, Epistemonikos, NICE Evidence Search, KSR Evidence and AHRQ
Client/patient involvement: No
Results
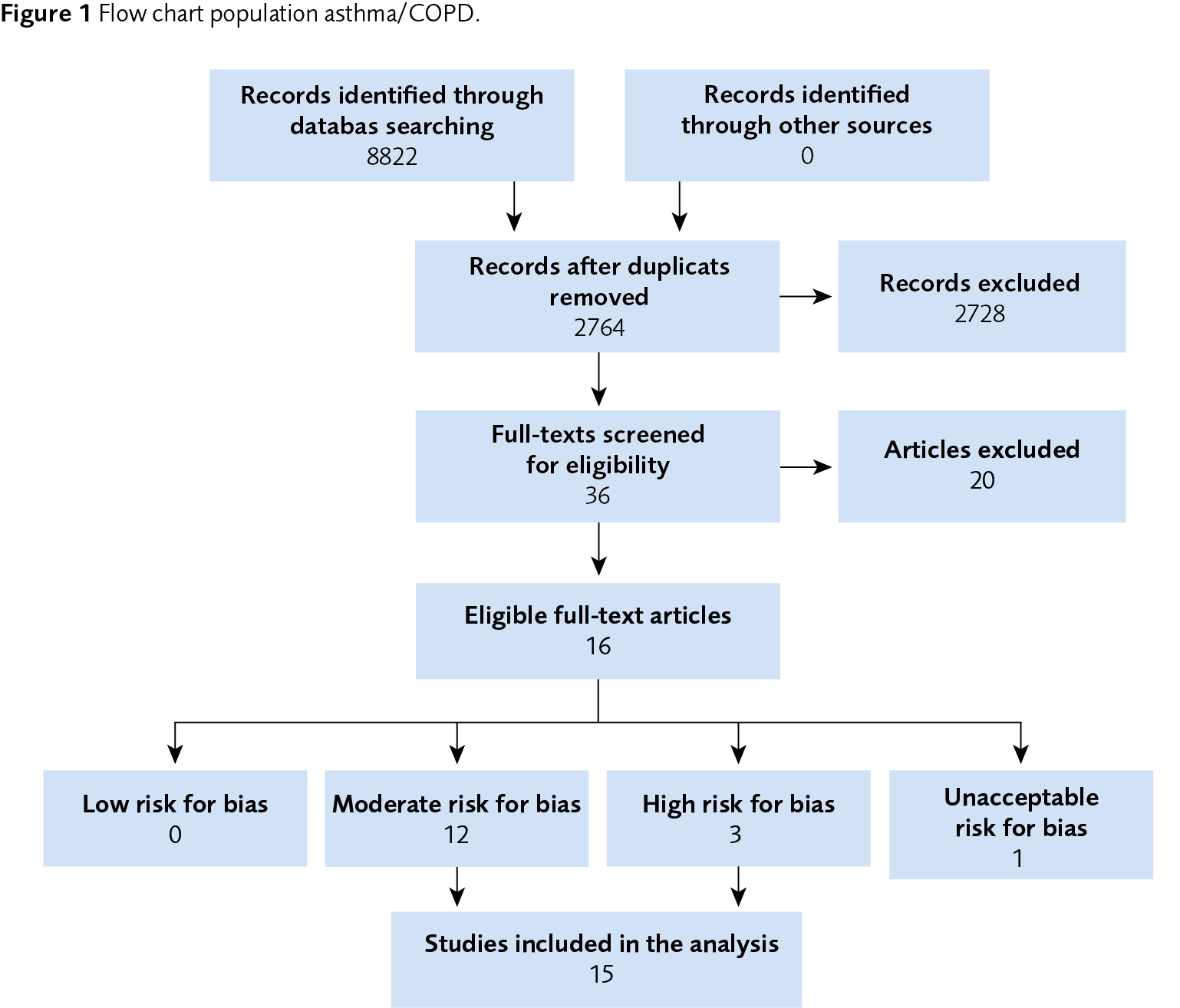
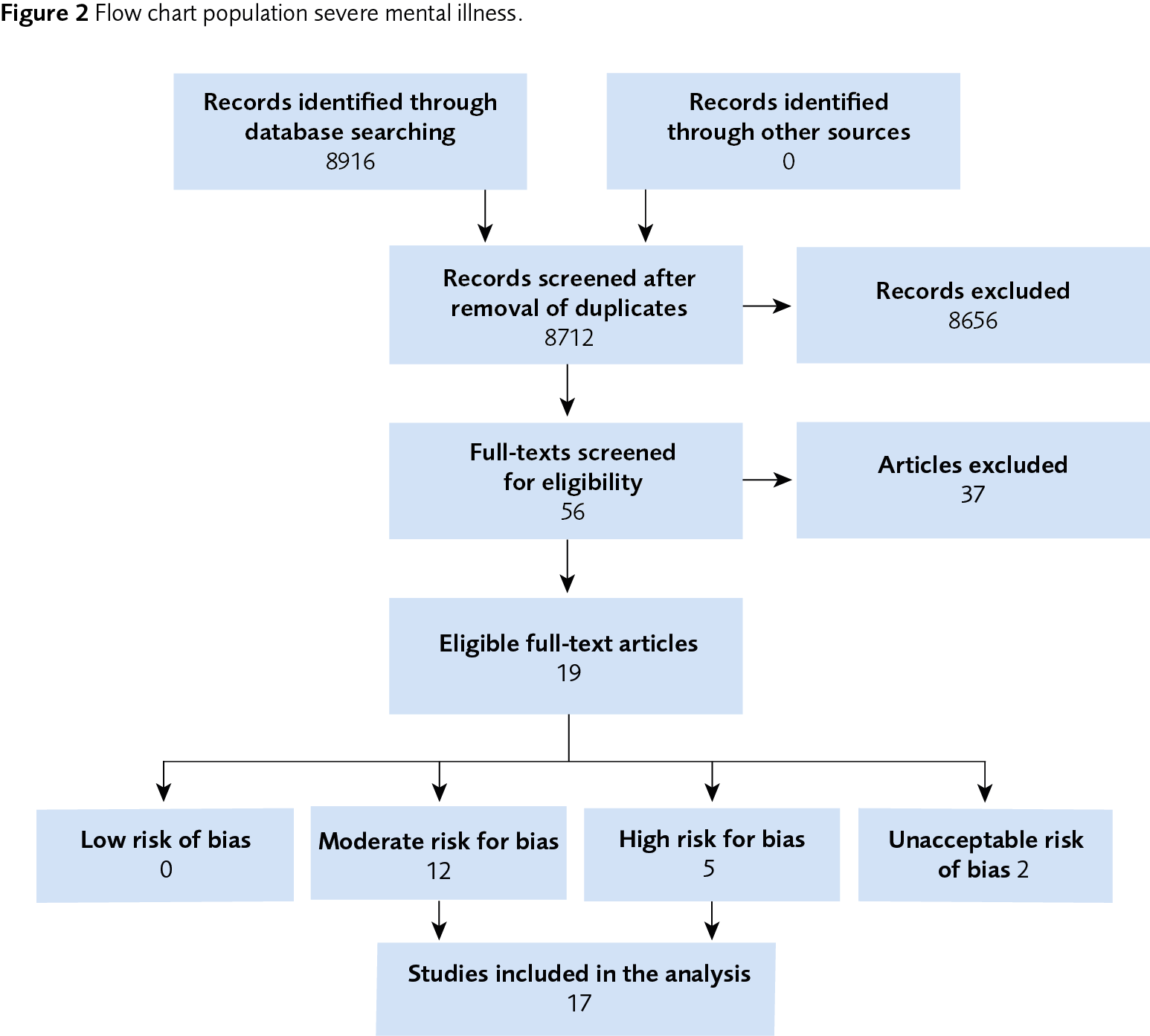
In the review for asthma or COPD, 15 articles were included following the literature review and assessment of relevance and risk of bias. In the review for severe mental illness, 17 articles were included. The included studies were mostly observational studies based on health care registries. The studies concerning asthma or COPD stemmed from Asia, Europe, and North America, while the studies concerning severe mental illness came from Europe and the US. The overarching results for the respective systematic review are shown in the tables below.
| Outcome | Number of studies/ participants (N) |
Summarised result | Certainty of evidence according to GRADE | Reasons for reduced certainty of the evidence |
| Mortality | 2 N=111 545 |
Higher relational continuity of care for persons with asthma or COPD prevents premature mortality. | Low | Risk of bias –1 Indirectness –0.5 Imprecision –0.5 |
| Hospitalisation | 9 N=525 716 |
Higher relational continuity of care for persons with asthma or COPD reduces the risk of hospitalization by a moderate to high degree. | Moderate | Risk of bias –1 |
| Emergency department visits | 5 N=362 305 |
Higher relational continuity of care for persons with asthma or COPD reduces the risk of emergency department visits by a moderate to high degree. | Low | Risk of bias –1 Indirectness –1 |
| Costs | 4 N=390 685 |
Higher relational continuity of care for persons with asthma or COPD reduces health care costs. | Low | Risk of bias –1 Imprecision –1 |
| Experience of participation in care and self-management of disease |
3 N=2026 |
Higher relational continuity of care for persons with asthma or COPD may improve patients’ experience of participation and knowledge about self-management of the disease | Very low | Risk of bias –1 Indirectness –2 Imprecision –0.5 |
| Treatment adherence | 1 N=971 |
It is not possible to assess the effects of relational continuity of care for persons with asthma or COPD on adherence to pharmacotherapy due to the very low certainty of the evidence. | Very low | Risk of bias –2 Indirectness –1 Imprecision –0.5 |
| SMI = severe mental illness | ||||
| Outcome | Number of studies/ participants (N) |
Summarised result | Certainty of evidence according to GRADE | Reasons for reduced certainty of the evidence |
| Mortality/ suicidality | 3 N=267 667 |
Higher relational continuity of care for persons with SMI can prevent premature mortality/suicide. | Low | Risk of bias –1 Inconsistency –0.5 Indirectness –0.5 |
| Hospitalisation | 4 N= 34 341 |
Higher relational continuity of care for persons with SMI can reduce the risk of hospitalisation. | Very low | Risk of bias –2 Indirectness –1 Imprecision –1 |
| Emergency department visits | 3 N=37 036 |
Higher relational continuity of care for persons with SMI can reduce the risk of emergency department visits. | Low | Risk of bias –1 Indirectness –1 |
| Costs | 3 N=8229 |
Higher relational continuity of care for persons with SMI can reduce health care costs. | Very low | Risk of bias –1 Inconsistency –1 Indirectness –1 |
| Symptoms and functioning | 3 N=5832 |
It is not possible to state if relational continuity of care can improve symptoms and functioning for persons with SMI. | Very low | Risk of bias –2 Indirectness –1 Imprecision –1 |
| Treatment adherence | 2 N=19 665 |
It is not possible to state if relational continuity of care influences treatment adherence for persons with SMI. | Very low | Risk of bias –1 Inconsistency –1 Indirectness –1 |
| Quality of life | 4 N=1852 |
Higher relational continuity of care for persons with SMI can improve their quality of life. | Low | Risk of bias –1 Inconsistency –1 |
Ethical and societal aspects
The effects of relational continuity that have been evaluated in the research field mostly concern medical values. In the ethical analysis, it is emphasised that relational continuity may have a value beyond medical effects, through other aspects and consequences, such as patients’ security, safety, and participation in their care.
Discussion
The results for the two investigated study populations are consistent in the sense that higher relational continuity is correlated with favourable effects. The results can be seen as an indication that relational continuity could be of importance also for other chronic conditions, both somatic and psychological.
Conflicts of Interest
In accordance with SBU’s requirements, the experts and scientific reviewers participating in this project have submitted statements about conflicts of interest. These documents are available at SBU’s secretariat. SBU has determined that the conditions described in the submissions are compatible with SBU’s requirements for objectivity and impartiality.
The full report in Swedish
The full report in Swedish Kontinuitet i vården
Scientific Article
Engström I, Hansson L, Ali L, Berg J, Ekstedt M, Engström S, et al. Relational continuity may give better clinical outcomes in patients with serious mental illness – a systematic review. BMC Psychiatry. 2023;23(1):952. Available from: https://doi.org/10.1186/s12888-023-05440-1
Lytsy P, Engström S, Ekstedt M, Engström I, Hansson L, Ali L, et al. Outcomes associated with higher relational continuity in the treatment of persons with asthma or chronic obstructive pulmonary disease: A systematic review. eClinicalMedicine. 2022;49. Available from: https://doi.org/10.1016/j.eclinm.2022.101492
Project group
Experts
- Lilas Ali, PhD
- Mirjam Ekstedt, Professor
- Ingemar Engström, Affiliated Professor
- Sven Engström, PhD
- Lars Hansson, Senior Professor
SBU
- Per Lytsy, Project Manager
- Jenny Berg, Assistant Project Manager/Health Economist
- Jenny Stenman, Project Administrator
- Jan Liliemark, Project Director
- Maja Kärrman Fredriksson, Information Specialist
External reviewers
- Peter Allebeck, Professor
- Patrik Midlöv, Professor
Flow charts
References
- SFS 2017:30. Hälso- och sjukvårdslag. Svensk författningssamling. Stockholm. [accessed April 25 2021]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/halso--och-sjukvardslag_sfs-2017-30.
- SFS 2014:821. Patientlag. Svensk författningssamling. Stockholm. [accessed April 22 2021]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/patientlag-2014821_sfs-2014-821.
- Rikdagens motion 1992/93:So218. Ädelreformen. Stockholm: Sveriges riksdag. [accessed April 22 2021]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/motion/adelreformen_GG02So218.
- Riksdagens motion 1994/95:So214. Psykiatrireformen. Stockholm: Sveriges riksdag. [accessed April 22 2021]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/motion/psykiatrireformen_GI02So214
- Riksdagens motion 1998/99:So436. Ädelreformen Motion. Stockholm: Sveriges riksdag. [accessed April 22 2021]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/motion/adelreformen_GM02So436.
- SFS 2008:962. Lag om valfrihetssystem. Svensk författningssamling. Stockholm. [accessed April 22 2021]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/lag-2008962-om-valfrihetssystem_sfs-2008-962.
- Ekonomifakta. Vårdcentraler i privat regi Stockholm: Ekonomifakta; 2019. [accessed April 22 2021]. Available from: https://www.ekonomifakta.se/Fakta/Valfarden-i-privat-regi/Vard-och-omsorg-i-privat-regi/vardcentraler-i-privat-regi/
- SOU 2016:2. Effektiv vård. Statens offentliga utredningar. Stockholm: Elanders Sverige AB. [accessed April 22 2021]. Available from: http://www.sou.gov.se/wp-content/uploads/2016/01/SOU-2016_2_Hela4.pdf.
- Anell A. Primärvårdens funktion, organisation och ekonomi – en litteraturöversikt. Rapport till utredningen En nationell samordnare för effektivare resursutnyttjande inom hälso- och sjukvården (S 2013:4). http://www.sou.gov.se/wp-content/uploads/2015/01/Prim%C3%A4rv%C3%A5rd-litteratur%C3%B6versikt-2015-S-2013_14.pdf. 2013.
- Regeringen 2013:Kommittédirektiv. En nationell samordnare för effektivare resursutnyttjande inom hälso- och sjukvården. Dir 2013:104. Stockholm. [accessed April 22 2021]. Available from: https://www.regeringen.se/rattsliga-dokument/kommittedirektiv/2013/11/dir.-2013104/.
- Regeringskansliet 2017:Samordnad utveckling för en modern, jämlik, tillgänglig och effektiv vård med fokus på primärvården. Dir 2017:24. [accessed Apriil 22 2021]. Available from: https://www.regeringen.se/rattsliga-dokument/kommittedirektiv/2017/03/dir.201724/.
- SOU 2017:53. God och nära vård. En gemensam färdplan och målbild. Statens offentliga utredningar. Stockholm: Elanders Sverige AB. [accessed April 22 2021]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/statens-offentliga-utredningar/sou-2017-53-_H5B353.
- Regeringens proposition 2017/18:83. Styrande principer inom hälso- och sjukvården och en förstärkt vårdgaranti. Stockholm: Regeringen. [accessed April 22 2021]. Available from: https://data.riksdagen.se/fil/693F2D62-15E2-4FF4-8A74-75BFFBFBC15A.
- SOU 2018:39. God och nära vård – En primärvårdsreform. Statens offentliga utredningar. Stockholm: Elanders Sverige AB. [accessed April 22 2021]. Available from: https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/2018/06/sou-201839/.
- Regeringskansliet 2017:Kommittédirektiv Ordning och reda i vården. Direktiv 2017:128. Stockholm. [accessed April 22 2021]. Available from: https://www.regeringen.se/rattsliga-dokument/kommittedirektiv/2017/12/direktiv-2017-128/.
- SOU 2019:42. Digifysiskt vårdval - Tillgänglig primärvård baserad på behov och kontinuitet. Statens offentliga utredningar. Stockholm: Elanders Sverige AB. [accessed April 22 2021]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/statens-offentliga-utredningar/digifysiskt-vardval---tillganglig-primarvard_H7B342.
- SOU 2020:19. God och nära vård - En reform för ett hållbart hälso- och sjukvårdssystem. Statens offentliga utredningar. Stockholm: Elanders AB. [accessed April 25 2021]. Available from: https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/2020/04/sou-202019/.
- Socialdepartementets proposition 2019/20/164. Inriktning för nära och tillgänglig vård - en primärvårdsreform. Stockholm: Regerlingskansliet. [accessed April 22 2021]. Available from: https://www.regeringen.se/rattsliga-dokument/proposition/2020/05/prop.-201920164/.
- Myndigheten för vård- och omsorgsanalys. Fast kontakt i primärvården. Patienters uppfattning om tillgången till fast läkarkontakt och fast vårdkontakt i primärvården. Stockholm; 2021 PM 2021:1. [accessed April 22 2021]. Available from: https://www.vardanalys.se/rapporter/fast-kontakt-i-primarvarden.
- Myndigheten för vård- och omsorgsanalys. Vården ur primärvårdsläkarnas perspektiv - en jämförelse mellan Sverige och tio andra länder. Stockholm; 2019 Rapport 2020:5. [accessed April 22 2021]. Available from: https://www.vardanalys.se/rapporter/ihp-2019/.
- PrimärvårdsKvalitet. Stockholm: Sveriges Kommuner och Regioner. [accessed April 22 2021]. Available from: http://primarvardskvalitet.skl.se/.
- Saultz JW. Defining and measuring interpersonal continuity of care. Ann Fam Med. 2003;1(3):134-43. Available from: https://doi.org/10.1370/afm.23.
- Haggerty J, Reid R, Freeman G, Starfield B, Adair CM, R. . Continuity of Care: A Multidisciplinary Review BMJ 2003;327:1219– 21 Available from: https://doi.org/10.1136/bmj.327.7425.1219.
- Deeny S, Gardner T, Al-Zaidy SB, I., Steventon A. Briefing: Reducing hospital admissions by improving continuity of care in general practice. The Health Foundation; 2017. [accessed April 22 2021]. Available from: https://www.health.org.uk/sites/default/files/ReducingAdmissionsGPContinuity.pdf.
- Meiqari L, Al-Oudat T, Essink D, Scheele F, Wright P. How have researchers defined and used the concept of ‘continuity of care’ for chronic conditions in the context of resource-constrained settings? A scoping review of existing literature and a proposed conceptual framework. Health Res Policy Sys 2019;17:27.
- Freeman GW, J., Heaney D, Howie J. Personal continuity and the quality of GP consultations: Knowing the doctor or having a regular doctor? European Journal of General Practice. 2002;8:3:90-4. Available from: https://doi.org/10.3109/13814780209160846
- Jee SH, Cabana MD. Indices for continuity of care: a systematic review of the literature. Med Care Res Rev. 2006;63(2):158-88. Available from: https://doi.org/10.1177/1077558705285294.
- Baker R, Freeman GK, Haggerty JL, Bankart MJ, Nockels KH. Primary medical care continuity and patient mortality: a systematic review. Br J Gen Pract. 2020;70(698):e600-e11. Available from: https://doi.org/10.3399/bjgp20X712289.
- Palmer W, Hemmings N, Rosen R, Keeble E, Williams S, Paddison C, et al. Improving access and continuity in general practice Evidence review. London: Nuffield Trust; 2018. [accessed April 22 2021].
- Available from: https://www.nuffieldtrust.org.uk/files/2019-01/improving-access-and-continuity-in-general-practice-evidence-review-final-update-01-2019.pdf.
- Lautamatti E, Sumanen MR, R. , Mattila KJ. Continuity of care is associated with satisfaction with local health care services. BMC Fam Pract. 2020;21:181. Available from: https://doi.org/10.1186/s12875-020-01251-5.
- Sveriges Läkarförbund. Läkarförbundets enkät till primärvårdens läkare 2015 - steg tre i förbundets utvärdering av vårdvalet i primärvården. Stockholm; 2015. [accessed April 22 2021]. Available from: https://www.nfgp.org/files/24/presentation_sweden_1_of_2.pdf.
- Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev. 2018;7:CD001271. Available from: https://doi.org/10.1002/14651858.CD001271.pub3.
- Riksrevisionen. Primärvårdens styrning - efter behov eller efterfrågan? RiR 2014:22. Stockholm; 2014. [accessed April 22 2021]. Available from:
- https://www.riksrevisionen.se/download/18.78ae827d1605526e94b2fc81/ 1518435446126/RIR_2014_22_%20v%C3%A5rdval_Anpassad_2.pd.
- Myndigheten för vård- och omsorgsanalys. Primärt i vården En studie om befolkningens syn på kontinuitet vid vårdcentraler. Rapport 2020:9. Stockholm; 2020. [accessed April 22 2021]. Available from: https://www.vardanalys.se/rapporter/primart-i-varden/.
- Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. . BMC Psychiatry. 2010;10:113. Available from: https://doi.org/10.1186/1471-244X-10-113.
- Doheney M, Agerholm J, Orsini N, Schön P, Burström B. Socio-demographic differences in the frequent use of emergency department care by older persons: a population-based study in Stockholm County. BMC Health Serv Res. 2019;19(202). Available from: https://doi.org/10.1186/s12913-019-4029-x.
- Al-Windi A, Elmfeldt D, Svärdsudd K. The influence of sociodemographic characteristics on health care utilisation in a Swedish municipality. Ups J Med Sci. 2004;109(1):33-42. Available from: https://doi.org/10.3109/2000-1967-108.
- Westin MW, R. Health and healthcare utilization among single mothers and single fathers in Sweden. Scand J Public Health. 2006;34(2):182-9. Available from: https://doi.org/10.1080/14034940500325939.
- Socialstyrelsen. Vård och omsorg om äldre. Lägesrapport 2020 Stockholm; 2020. [accessed April 22 2021]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2020-3-6603.pdf.
- Cho KH, Nam CM, Choi Y, Choi JW, Lee SH, Park EC. Impact of continuity of care on preventable hospitalization of patients with type 2 diabetes: a nationwide Korean cohort study, 2002-10. Int J Qual Health Care. 2016;28(4):478-85. Available from: https://doi.org/10.1093/intqhc/mzw050.
- Maciejewski ML, Hammill BG, Ding L, Curtis LH, Bayliss EA, Hoffman AF, et al. Care continuity impacts medicare expenditures of older adults: Fact or fiction? Healthc (Amst). 2020;8(1):100364. Available from: https://doi.org/10.1016/j.hjdsi.2019.05.004.
- Holmes HM, Luo R, Kuo YF, Baillargeon J, Goodwin JS. Association of potentially inappropriate medication use with patient and prescriber characteristics in Medicare Part D. 2013;22(7):728-34. Available from: https://doi.org/10.1002/pds.3431.
- Hansen RA, Voils CI, Farley JF, Powers BJ, Sanders LL, Sleath B, et al. Prescriber continuity and medication adherence for complex patients. Ann Pharmacother. 2015;49(3):293-302. Available from: https://doi.org/10.1177/1060028014563266.
- Maciejewski ML, Hammill BG, Bayliss EA, Ding L, Voils CI, Curtis LH, et al. Prescriber Continuity and Disease Control of Older Adults. Med Care. 2017;55(4):405-10. Available from: https://doi.org/10.1097/MLR.0000000000000658.
- Gill JM, Mainous AG, 3rd, Diamond JJ, Lenhard MJ. Impact of provider continuity on quality of care for persons with diabetes mellitus. Ann Fam Med. 2003;1(3):162-70. Available from: https://doi.org/10.1370/afm.22.
- Socialstyrelsen. Nationella riktlinjer för vård vid astma och KOL Stöd för styrning och ledning. Stockholm: Socialstyrelsen; 2020. Nationella riktlinjer. [accessed April 22 2021]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/nationella-riktlinjer/2020-12-7135.pdf.
- McGrath J, Saha S, Welham J, El Saadi O, MacCauley C, Chant D. A systematic review of the incidence of schizophrenia: the distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Med. 2004;2:13. Available from: https://doi.org/10.1186/1741-7015-2-13.
- Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. 2005;2(5):e141. Available from: https://doi.org/10.1371/journal.pmed.0020141.
- Socialstyrelsen. Nationella riktlinjer för vård och stöd vid schizofreni och schizofreniliknande tillstånd Stöd för styrning och ledning. Stockholm: Socialstyrelsen; 2018. Nationella riktlinjer. [accessed April 22 2021]. Available from: https://www.socialstyrelsen.se/regler-och-riktlinjer/nationella-riktlinjer/riktlinjer-och-utvarderingar/schizofreni/.
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018;392:1789-858. Available from: https://doi.org/10.1016/S0140-6736(18)32279-7.
- SBU. Behandling av depressionssjukdomar, volym 1. En systematisk litteraturöversikt. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2004. SBU Utvärderar 166/1. Available from: https://www.sbu.se/sv/publikationer/SBU-utvarderar/behandling-av-depressionssjukdomar/.
- Dell'Aglio JC, Jr., Basso LA, Argimon, II, Arteche A. Systematic review of the prevalence of bipolar disorder and bipolar spectrum disorders in population-based studies. Trends Psychiatry Psychother. 2013;35(2):99-105. Available from: https://doi.org/10.1590/s2237-60892013000200002.
- Sanai-Farid SB, L. Bipolär sjukdom. Läkartidningen. 2019;116.
- Goering PN, Wasylenki D. Integrated Mental Health Services: Modern Community Psychiatry. 1 ed. Breakey WR, editor. New York: Oxford University Press; 1996.
- SBU. Vetenskapligt underlag till Socialstyrelsens nationella riktlinjer för vård och behandling vid schizofreni. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2017. SBU Bereder 271. [accessed April 22 2021]. Available from: https://www.sbu.se/271.
- Dieterich M, Irving CB, Bergman H, Khokhar MA, Park B, Marshall M. Intensive case management for severe mental illness. Cochrane Database Syst Rev. 2017;1:CD007906. Available from: https://doi.org/10.1002/14651858.CD007906.pub3.
- SBU. Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten: en metodbok. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2020. [accessed April 22 2021]. Available from: https://www.sbu.se/sv/metod/sbus-metodbok/.
- Viktlistor för NordDRG. Stockholm: Socialstyrelsen; 2019. [accessed April 22 2021]. Available from: https://www.socialstyrelsen.se/utveckla-verksamhet/e-halsa/klassificering-och-koder/drg/viktlistor/.
- Statistik om NordDRG. Socialstyrelsens statistikdatabas: DRG-statistik, Antal vårdtillfällen, 2015–2019. Stockholm: Socialstyrelsen. [accessed April 22 2021]. Available from: https://www.socialstyrelsen.se/utveckla-verksamhet/e-halsa/klassificering-och-koder/drg/statistik-om-norddrg/.
- Statistik om vårdproduktion och vårdkonsumtion enligt DRG. Stockholm: Socialstyrelsen. [accessed April 28 2021]. Available from: https://www.socialstyrelsen.se/statistik-och-data/statistik/statistikamnen/vardproduktion-och-vardkonsumtion/.
- Shor E, Roelfs D, Vang ZM. The "Hispanic mortality paradox" revisited: Meta-analysis and meta-regression of life-course differentials in Latin American and Caribbean immigrants' mortality. Soc Sci Med. 2017;186:20-33. Available from: https://doi.org/10.1016/j.socscimed.2017.05.049.
- Grant RL. Converting an odds ratio to a range of plausible relative risks for better communication of research findings. BMJ. 2014;348:f7450. Available from: https://doi.org/10.1136/bmj.f7450.
- SBU. Etiska aspekter på insatser inom hälso- och sjukvården. En vägledning för att identifiera relevanta etiska aspekter. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2021. [accessed April 22 2021 2021]. Available from: https://www.sbu.se/globalassets/ebm/etiska_aspekter_halso_sjukvarden.pdf.
- Hussey PS, Schneider EC, Rudin RS, Fox DS, Lai J, Pollack CE. Continuity and the costs of care for chronic disease. JAMA Internal Medicine. 2014;174(5):742-8. Available from: https://doi.org/10.1001/jamainternmed.2014.245.
- Swanson JO, Vogt V, Sundmacher L, Hagen TP, Moger TA. Continuity of care and its effect on readmissions for COPD patients: A comparative study of Norway and Germany. Health Policy. 2018;122(7):737-45. Available from: https://doi.org/10.1016/j.healthpol.2018.05.013.
- Love MM, Mainous IAG, Talbert JC, Hager GL. Continuity of care and the physician-patient relationship: The importance of continuity for adult patients with asthma. Journal of Family Practice. 2000;49(11):998-1004.
- Wireklint P, Hasselgren M, Montgomery S, Lisspers K, Ställberg B, Janson C, et al. Factors associated with knowledge of self-management of worsening asthma in primary care patients - a cross-sectional study. The Journal of asthma : official journal of the Association for the Care of Asthma. 2020:1-11. Available from: https://doi.org/10.1080/02770903.2020.1753209.
- Svereus S, Larsson K, Rehnberg C. Clinic continuity of care, clinical outcomes and direct costs for COPD in Sweden: a population based cohort study. European Clinical Respiratory Journal. 2017;4(1):1290193. Available from: https://doi.org/10.1080/20018525.2017.1290193.
- Frandsen BR, Joynt KE, Rebitzer JB, Jha AK. Care Fragmentation, Quality, and Costs Among Chronically 111 Patients. American Journal of Managed Care. 2015;21(5):355-62.
- Kao YH, Wu SC. STROBE-compliant article: Is continuity of care associated with avoidable hospitalization among older asthmatic patients? Medicine. 2016;95(38):e4948. Available from: https://doi.org/https://dx.doi.org/10.1097/MD.0000000000004948.
- Kao YH, Wu SC. Effect of Continuity of Care on Emergency Department Visits in Elderly Patients with Asthma in Taiwan. Journal of the American Board of Family Medicine: JABFM. 2017;30(3):384-95. Available from: https://doi.org/https://dx.doi.org/10.3122/jabfm.2017.03.160285.
- Kao YH, Tseng TS, Ng YY, Wu SC. Association between continuity of care and emergency department visits and hospitalization in senior adults with asthma-COPD overlap. Health Policy. 2019;123(2):222-8. Available from: https://doi.org/https://dx.doi.org/10.1016/j.healthpol.2018.11.005.
- Cho KH, Kim YS, Nam CM, Kim TH, Kim SJ, Han KT, et al. The Association between Continuity of Care and All-Cause Mortality in Patients with Newly Diagnosed Obstructive Pulmonary Disease: A Population-Based Retrospective Cohort Study, 2005-2012. PLoS ONE [Electronic Resource]. 2015;10(11):e0141465. Available from: https://doi.org/https://dx.doi.org/10.1371/journal.pone.0141465.
- Einarsdottir K, Preen DB, Emery JD, Kelman C, Holman CD. Regular primary care lowers hospitalisation risk and mortality in seniors with chronic respiratory diseases. Journal of General Internal Medicine. 2010;25(8):766-73. Available from: https://doi.org/https://dx.doi.org/10.1007/s11606-010-1361-6.
- Hong JS, Kang HC, Kim J. Continuity of care for elderly patients with diabetes mellitus, hypertension, asthma, and chronic obstructive pulmonary disease in Korea. Journal of Korean Medical Science. 2010;25(9):1259-71. Available from: https://doi.org/https://dx.doi.org/10.3346/jkms.2010.25.9.1259.
- Corsico AG, Cazzoletti L, de Marco R, Janson C, Jarvis D, Zoia MC, et al. Factors affecting adherence to asthma treatment in an international cohort of young and middle-aged adults. Respiratory Medicine. 2007;101(6):1363-7. Available from: https://doi.org/10.1016/j.rmed.2006.11.012.
- Lin IP, Wu SC. Effects of long-term high continuity of care on avoidable hospitalizations of chronic obstructive pulmonary disease patients. Health Policy. 2017;121(9):1001-7. Available from: https://doi.org/https://dx.doi.org/10.1016/j.healthpol.2017.06.010.
- Uijen AA, Bischoff EW, Schellevis FG, Bor HH, Van Den Bosch WJ, Schers HJ. Continuity in different care modes and its relationship to quality of life: A randomised controlled trial in patients with COPD. British Journal of General Practice. 2012;62(599):e422-e8. Available from: https://doi.org/10.3399/bjgp12X649115.
- Adair CE, McDougall GM, Mitton CR, Joyce AS, Wild TC, Gordon A, et al. Continuity of care and health outcomes among persons with severe mental illness. Psychiatric Services. 2005;56(9):1061-9. Available from: https://doi.org/10.1176/appi.ps.56.9.1061.
- Adnanes M, Kalseth J, Ose SO, Ruud T, Rugkasa J, Puntis S. Quality of life and service satisfaction in outpatients with severe or non-severe mental illness diagnoses. Quality of Life Research. 2019;28(3):713-24. Available from: https://doi.org/https://dx.doi.org/10.1007/s11136-018-2039-5.
- Bindman J, Johnson S, Szmukler G, Wright S, Kuipers E, Thornicroft G, et al. Continuity of care clinical outcome: A prospective cohort study. Social Psychiatry and Psychiatric Epidemiology. 2000;35(6):242-7. Available from: https://doi.org/10.1007/s001270050234.
- Catty J, White S, Clement S, Cowan N, Geyer C, Harvey K, et al. Continuity of care for people with psychotic illness: its relationship to clinical and social functioning. International Journal of Social Psychiatry. 2013;59(1):5-17. Available from: https://doi.org/https://dx.doi.org/10.1177/0020764011421440.
- Chien CF, Steinwachs DM, Lehman A, Fahey M, Skinner EA. Provider continuity and outcomes of care for persons with schizophrenia. Mental Health Services Research. 2000;2(4):201-11. Available from: https://doi.org/10.1023/A:1010160419561.
- Conti V, Lora A, Cipriani A, Fortino I, Merlino L, Barbui C. Persistence with pharmacological treatment in the specialist mental healthcare of patients with severe mental disorders. European Journal of Clinical Pharmacology. 2012;68(12):1647-55. Available from: https://doi.org/10.1007/s00228-012-1298-2.
- Desai RA, Dausey DJ, Rosenheck RA. Mental health service delivery and suicide risk: the role of individual patient and facility factors. American Journal of Psychiatry. 2005;162(2):311-8. Available from: https://doi.org/10.1176/appi.ajp.162.2.311.
- Farley JF, Wang CC, Hansen RA, Voils CI, Maciejewski ML. Continuity of antipsychotic medication management for Medicaid patients with schizophrenia. Psychiatric Services. 2011;62(7):747-52. Available from: https://doi.org/https://dx.doi.org/10.1176/ps.62.7.pss6207_0747.
- Giacco D, Bird VJ, Ahmad T, Bauer M, Lasalvia A, Lorant V, et al. The same or different psychiatrists for in- and out-patient treatment? A multi-country natural experiment. Epidemiology & Psychiatric Science. 2018;29:e10. Available from: https://doi.org/https://dx.doi.org/10.1017/S2045796018000732.
- Hoertel N, Limosin F, Leleu H. Poor longitudinal continuity of care is associated with an increased mortality rate among patients with mental disorders: results from the French National Health Insurance Reimbursement Database. European Psychiatry: the Journal of the Association of European Psychiatrists. 2014;29(6):358-64. Available from: https://doi.org/https://dx.doi.org/10.1016/j.eurpsy.2013.12.001.
- Kaltsidis G, Bamvita JM, Grenier G, Fleury MJ. Predictors of Frequent Emergency Department Utilization for Mental Health Reasons. Journal of Behavioral Health Services & Research. 2020;17:17. Available from: https://doi.org/https://dx.doi.org/10.1007/s11414-020-09695-4.
- Macdonald A, Adamis D, Craig T, Murray R. Continuity of care and clinical outcomes in the community for people with severe mental illness. British Journal of Psychiatry. 2019;214(5):273-8. Available from: https://doi.org/https://dx.doi.org/10.1192/bjp.2018.261.
- Mitton CR, Adair CE, McDougall GM, Marcoux G. Continuity of care and health care costs among persons with severe mental illness. Psychiatric Services. 2005;56(9):1070-6. Available from: https://doi.org/10.1176/appi.ps.56.9.1070.
- Puntis SR, Rugkasa J, Burns T. The association between continuity of care and readmission to hospital in patients with severe psychosis. Social Psychiatry & Psychiatric Epidemiology. 2016;51(12):1633-43. Available from: https://doi.org/10.1007/s00127-016-1287-3.
- Ride J, Kasteridis P, Gutacker N, Doran T, Rice N, Gravelle H, et al. Impact of family practice continuity of care on unplanned hospital use for people with serious mental illness. Health Services Research. 2019;54(6):1316-25. Available from: https://doi.org/https://dx.doi.org/10.1111/1475-6773.13211.
- van der Lee A, de Haan L, Beekman A. Schizophrenia in the Netherlands: Continuity of Care with Better Quality of Care for Less Medical Costs. PLoS ONE [Electronic Resource]. 2016;11(6):e0157150. Available from: https://doi.org/https://dx.doi.org/10.1371/journal.pone.0157150.
- Watkins KE, Paddock SM, Hudson TJ, Ounpraseuth S, Schrader AM, Hepner KA, et al. Association Between Quality Measures and Mortality in Individuals With Co-Occurring Mental Health and Substance Use Disorders. Journal of Substance Abuse Treatment. 2016;69:1-8. Available from: https://doi.org/https://dx.doi.org/10.1016/j.jsat.2016.06.001.
- SBU. Patient-läkarrelationen: läkekonst på vetenskaplig grund. Stockholm: Natur och kultur i samarbete med Statens beredning för medicinsk utvärdering (SBU); 1999.
- Myndigheten för vård- och omsorgsanalys. Vården ur befolkningens perspektiv En jämförelse mellan Sverige och tio andra länder Stockholm; 2021 2021:4. [accessed April 25 2021]. Available from: https://www.vardanalys.se/rapporter/varden-ur-befolkningens-perspektiv-2020/.
- Sandlund M, Bremer A, Ågård A, Engström I, Sallin K. Kontinuitet främjar personligt och professionellt ansvarstagande. Läkartidningen. 2017;114:ETHI.
- Knudsen HC, Thornicroft G. Mental Health Service Evaluation. Cambridge: Cambridge University Press; 1996.
- Tansella M, Thornicroft G. A conceptual framework for mental health services: the matrix model. Psychol Med. 1998;28(3):503-8. Available from: https://doi.org/10.1017/s0033291796005880.
- Engström I, Ågård A. Läkarens viktiga möte med patienten. Läkartidningen. 2017;114:ESC3.
- Engström I, Bengtsson S. Vården börjar alltid med mötet. Läkartidningen. 2017;114:ERRM.
- Lundberg M, Lood Q, Swedberg K, Norberg A. Personcentrering - en etik i praktiken. I Ekman I. (red). Personcentrering inom hälso- och sjukvård. Från filosofi till praktik. Personcentrering inom hälso- och sjukvård (liber.se). Stockholm: Liber AB; 2020.
- Ekman I, Swedberg K, Taft C, Lindseth A, Norberg A, Brink E, et al. Person-centered care--ready for prime time. Eur J Cardiovasc Nurs. 2011;10(4):248-51. Available from: https://doi.org/10.1016/j.ejcnurse.2011.06.008.
- Yang F, Xiong ZF, Yang C, Li L, Qiao G, Wang Y, et al. Continuity of Care to Prevent Readmissions for Patients with Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis. COPD. 2017;14(2):251-61. Available from: https://doi.org/10.1080/15412555.2016.1256384.
- Diab N, Gershon AS, Sin DD, Tan WC, Bourbeau J, Boulet LP, et al. Underdiagnosis and Overdiagnosis of Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2018;198(9):1130-9. Available from: https://doi.org/10.1164/rccm.201804-0621CI.
- Puntis S, Rugkasa J, Forrest A, Mitchell A, Burns T. Associations between continuity of care and patient outcomes in mental health care: a systematic review. Psychiatr Serv. 2015;66(4):354-63. Available from: https://doi.org/10.1176/appi.ps.201400178.
- Omer S, Priebe S, Giacco D. Continuity across inpatient and outpatient mental health care or specialisation of teams? A systematic review. Eur Psychiatry. 2015;30(2):258-70. Available from: https://doi.org/10.1016/j.eurpsy.2014.08.002.
- Pereira Gray DJ, Sidaway-Lee K, White E, Thorne A, Evans PH. Continuity of care with doctors-a matter of life and death? A systematic review of continuity of care and mortality. BMJ Open. 2018;8(6):e021161. Available from: https://doi.org/10.1136/bmjopen-2017-021161.
- Kao YH, Lin WT, Chen WH, Wu SC, Tseng TS. Continuity of outpatient care and avoidable hospitalization: a systematic review. Am J Manag Care. 2019;25(4):e126-e34.
- Health Quality Ontario. Continuity of care to optimize chronic disease management in the community setting: an evidence-based analysis. Ontario; 2013. Ont Health Technol Assess Ser 13(6). [accessed April 26 2021]. Available from: http://www.hqontario.ca/Portals/0/Documents/evidence/reports/full-report-continuity-care-ocdm-130906-en.pdf.
- Santomassino M, Costantini GD, McDermott M, Primiano D, Slyer JT, Singleton JK. A systematic review on the effectiveness of continuity of care and its role in patient satisfaction and decreased hospital readmissions in the adult patient receiving home care services. JBI Libr Syst Rev. 2012;10(21):1214-59. Available from: https://doi.org/10.11124/01938924-201210210-00001.
- Facchinetti G, D'Angelo D, Piredda M, Petitti T, Matarese M, Oliveti A, et al. Continuity of care interventions for preventing hospital readmission of older people with chronic diseases: A meta-analysis. Int J Nurs Stud. 2020;101:103396. Available from: https://doi.org/10.1016/j.ijnurstu.2019.103396.
- Chen HM, Tu YH, Chen CM. Effect of Continuity of Care on Quality of Life in Older Adults With Chronic Diseases: A Meta-Analysis. Clin Nurs Res. 2017;26(3):266-84. Available from: https://doi.org/10.1177/1054773815625467.
- Bian J, Lyu T, Loiacono A, Viramontes TM, Lipori G, Guo Y, et al. Assessing the practice of data quality evaluation in a national clinical data research network through a systematic scoping review in the era of real-world data. J Am Med Inform Assoc. 2020;27(12):1999-2010. Available from: https://doi.org/10.1093/jamia/ocaa245.
- Berger ML, Sox H, Willke RJ, Brixner DL, Eichler HG, Goettsch W, et al. Good practices for real-world data studies of treatment and/or comparative effectiveness: Recommendations from the joint ISPOR-ISPE Special Task Force on real-world evidence in health care decision making. Pharmacoepidemiol Drug Saf. 2017;26(9):1033-9. Available from: https://doi.org/10.1002/pds.4297.
- van Walraven C, Oake N, Jennings A, Forster AJ. The association between continuity of care and outcomes: a systematic and critical review. J Eval Clin Pract. 2010;16(5):947-56. Available from: https://doi.org/10.1111/j.1365-2753.2009.01235.x

 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services
 Share on Facebook
Share on Facebook
 Share on LinkedIn
Share on LinkedIn
 Share via Email
Share via Email