Health care interventions in case of long-term sick leave
A systematic review and assessment of medical, economic, social and ethical aspects
Conclusions
- Unimodal and multimodal interventions and interventions that involve workplace contact or coordination activities towards the workplace may have a positive effect on return to work in the short time perspective (up to 12 months) for persons on sick leave for mental or musculoskeletal disorders. The certainty of the evidence was assessed to be low. It was not possible to estimate the size of the effect.
- It was not possible to determine the effect on return to work for interventions targeting health care professionals or health care organizations. The certainty of the evidence was assessed to be very low.
- It was not possible to determine intervention effects on return to work in the long-time perspective for any type of intervention. The certainty of the evidence was assessed to be very low.
- It was not possible to determine the effect of interventions on participants’ health or function for any type of intervention. The certainty of the evidence was assessed to be very low.
- It was not possible to determine the effect on return to work, health or functioning for persons on sick leave for breast cancer diagnosis.
- There were no studies investigating return to work interventions for patients on sick leave for post covid or bipolar disorder.
Background
Persons on long term sick leave (defined as longer than 3 months) may benefit from interventions facilitating return to work.
Aim
The aim of this systematic review was to evaluate effects of interventions that may be initiated within the health care system. The primary outcome of interest was return to work. Secondary outcomes included intervention's effects on health and functioning. The aim was also to examine the cost-effectiveness of the evaluated interventions, highlight ethical aspects and identify scientific evidence gaps to guide future research.
Method
A systematic review was conducted in accordance with the PRISMA statement. The protocol is registered in Prospero (CRD42022315330). The certainty of evidence was assessed with the GRADE framework. Studies considered for inclusion were targeting populations on sick leave due to the most common diagnoses for long term sick leave based on Swedish statistics. All types of interventions were considered and were characterized as unimodal (one treatment), multimodal (several treatment modalities), intervention including workplace contact or workplace coordination, and interventions aiming at health care personnel /organizations.
Results were summarized for short time (≤12 months) and long-time (>12 months) effects on return to work. Effects on health and/or function were assessed regardless of follow-up time.
Effects on costs and cost effectiveness were assessed based on results in included studies.
Ethical analysis was performed by the project group, which included an academic scholar in ethics. The method was mainly based on discussion, aimed at identifying conflicts of interest between different agents involved, and potential ethical dilemmas.
Inclusion criteria:
Population
Persons on sick leave for a condition that is common when on long term sick leave according to Swedish statistics.
Intervention
Any intervention that could be initiated within health care practice with the overall aim of facilitating return to work. Interventions could be unimodal or multimodal. Furthermore, it could be collaborative with other organisations, such as employer, occupational health care, or social insurance agency.
Control
Any control, which could be no treatment, treatment as usual, wait list or other active treatment.
Outcome
Primary: measures of sick leave, work participation and/or return to work.
Secondary: measures on health and or functioning.
Health economic outcomes: effects on cost and cost effectiveness
Study design
Randomized controlled studies, including cluster randomized studies.
Other criteria
At least 6 months follow-up.
We performed risk of bias assessments and included studies with low or moderate risk of bias in the analysis.
Due to extensive heterogeneity, we performed a synthesis without meta-analysis investigating effects for each intervention category (unimodal, multimodal, workplace contact or coordination, and interventions targeting heath care staff) and study populations on sick leave for mental disorder, musculoskeletal disorders, or both.
Language: English, Swedish, Norwegian or Danish.
Search period: From 2000 to 2022. Final search May, 2022.
Databases searched: Cochrane Library, EMBASE, PsycINFO (EBSCO) and Medline.
Client/patient involvement: No
Results
We included 95 articles based on 68 unique studies. A total of 40 000 persons were evaluated for the return-to-work outcome. We included 10 studies that evaluated effects on costs and cost effectiveness.
Most of the studies included did not report significant findings on return to work.
We found low certainty evidence that unimodal, multimodal and workplace/coordination interventions may improve return to work.
| RTW = return to work; short = short period, 12 months or shorter; long = long period, longer than 12 months; HoF = Health or functioning. ⊕◯◯◯ = very low certainty, the effect is uncleart; ⊕⊕◯◯ = low certainty, the intervention may have a positive effect; Green colour = Positiv effect of the intervention; Orange colour = Unclear effect of the intervention |
||||||||||
| Population | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mental or muskuloskeletal disorder | Mental disorder | Muskuloskeletal disorder | ||||||||
| Outcome | RTW short | RTW long |
HoF | RTW short | RTW long |
HoF | RTW short | RTW long |
HoF | |
| Type of intervention | Unimodal intervention | ⊕⊕◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕⊕◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ |
| Multimodal intervention |
⊕⊕◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕⊕◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | |
| Coordination/ Workplace intervention |
⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕⊕◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | |
| Interventions targeting health care personnel | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | ⊕◯◯◯ | |
Health Economic Assessment
Ten studies evaluating intervention effects on costs or cost effectiveness were included. It was not possible to assess overall effects based on categories of intervention types, due to the low number of studies in each category. It was concluded that also a small positive effect on return to work (> 5 days relative reduction in one year per person), would result in positive effects on a societal level.
Ethics
The practice of sick leave and return to work is a complex ethical situation where patients may be vulnerable in terms of reduced autonomy and integrity.
Discussion
Despite lots of well conducted research, few studies presented robust support of the relative effectiveness of the investigated intervention. Our results are in line with other systematic reviews in the area. We advise that well conducted research studies with positive findings is replicated in future research. There is a need present outcomes and results in a way that makes it possible to perform meta analyses.
Conflicts of Interest
In accordance with SBU’s requirements, the experts and scientific reviewers participating in this project have submitted statements about conflicts of interest. These documents are available at SBU’s secretariat. SBU has determined that the conditions described in the submissions are compatible with SBU’s requirements for objectivity and impartiality.
The full report in Swedish
The full report in Swedish, Insatser i vården vid långtidssjukskrivning

Project group
Experts
- Professor Gunnar Bergström. University of Gävle
- Assistant/Associate Professor Emilie Friberg. Karolinska Institutet
- Dr Therese Eskilsson. University of Umeå
- Assistant/Associate Professor Sara Holmberg. Linneaus University
- Assistant/Associate Professor Lars Lindblom. University of Linköping
SBU
- Per Lytsy, Project Manager (www.sbu.se/359)
External reviewers
- Henna Hasson, professor, LIME, Karolinska institutet, Swedan
- Sigmund Østgård Gismervik, associate professor, NTNU, Norway.
Flow Chart
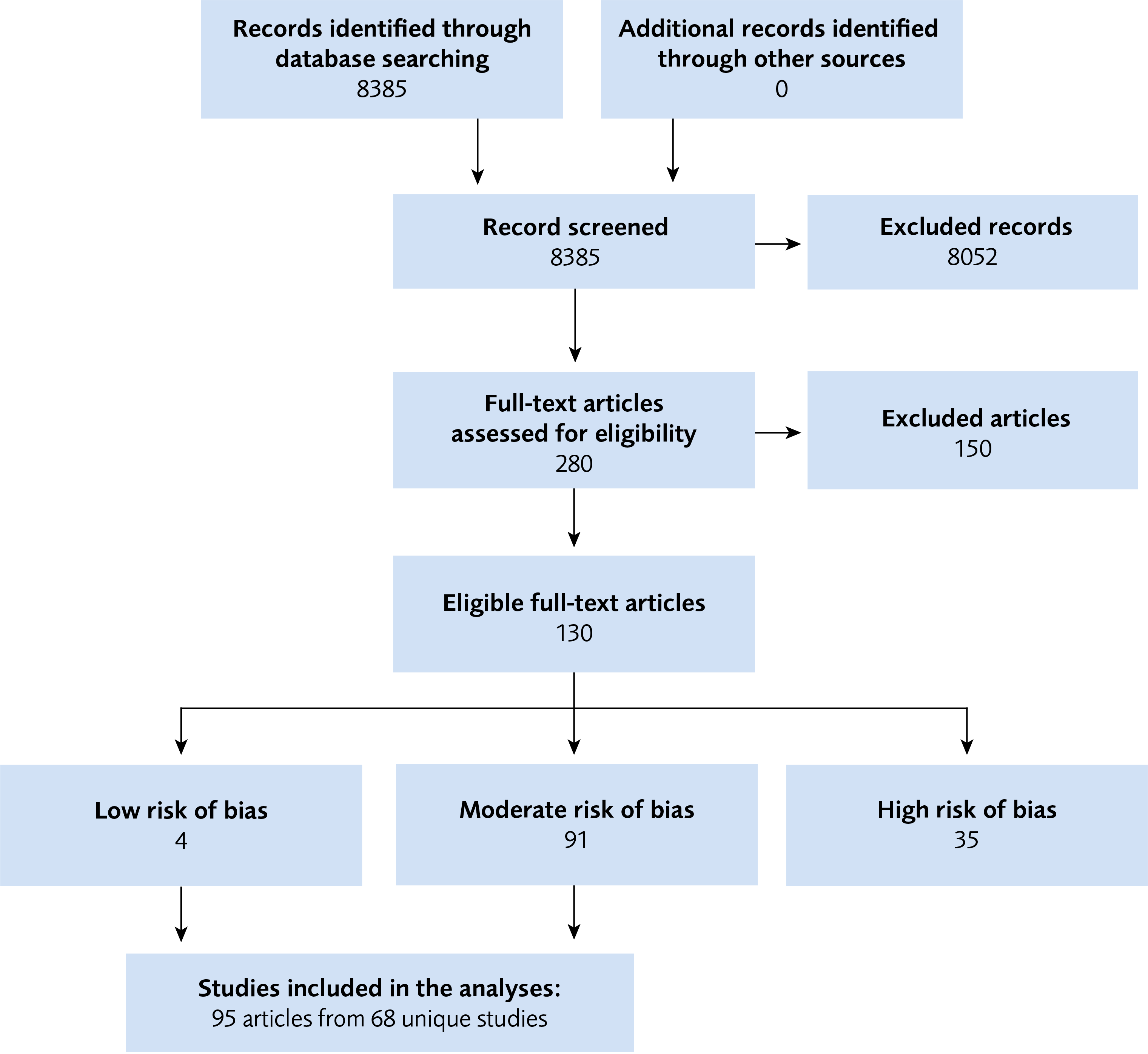
Figure 1 Flow Chart
References
- Regeringskansliet 2021:Regleringsbrev för budgetåret 2021 avseende Statens beredning för medicinsk och social utvärdering. S2020/09593 (delvis). Stockholm.
- Järvholm B, Mannelqvist R, Olofsson C, Torén K. Försäkringsmedicin. Lund: Studentlitteratur AB; 2013.
- SOU 2020:24. Tillsammans för en välfungerande sjukskrivnings- och rehabiliteringsprocess Statens offentliga utredningar. Stockholm: Norstedts. [accessed Aug 30 2022]. Available from: Tillsammans för en välfungerande sjukskrivnings- och rehabiliteringsprocess - Regeringen.se.
- SBU. Sjukskrivning – orsaker, konsekvenser och praxis. En systematisk litteraturöversikt. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2003. SBU-rapport 167. Available from: https://www.sbu.se/contentassets/20cf3afd857a4e7797b0ad59971398ff/sjukskrivning.pdf.
- Sjukskrivningsmiljarden 2013. Stockholm: Sveriges Kommuner och Regioner (SKR); 2013. [accessed Dec 12 2022]. Available from: https://skr.se/skr/tjanster/rapporterochskrifter/publikationer/sjukskrivningsmiljarden2013.65509.html.
- Söder M. Sjukskrivningsmiljarden. Landstingets syn på ekonomiska incitament för att påverka sjukfrånvaron. Göteborg: Inspektionen för socialförsäkringen (ISF); 2013 11. [accessed Dec 12 2022]. Available from: https://isf.se/publikationer/rapporter/2013/2013-08-15-sjukskrivningsmiljarden.
- Aronsson G, Lundberg U. REHABILITERING OCH SAMORDNING. Ett regeringsuppdrag om att utvärdera, sammanställa och analysera resultat från forskningsprogrammet Rehsam (S2014/5621/SF). Slutrapport: Utvärdering av Rehsams forskningsprogram 2009–2011. Stockholm: Forte – Forskningsrådet för hälsa, arbetsliv och välfärd; 2014. [accessed Dec 12 2022]. Available from: https://forte.se/app/uploads/2017/04/rehsam-webb.pdf.
- Busch H, Bonnevier H, Hagberg J, Lohela Karlsson M, Bodin L, Norlund A, et al. En nationell utvärdering av rehabiliteringsgarantins effekter på sjukfrånvaro och hälsa. Slutrapport del I. Stockholm: Enheten för interventions- och implementeringsforskning, Institutet för miljömedicin (IMM), Karolinska Institutet; 2011. [accessed Nov 22 2022]. Available from: https://ki.se/media/120214/download?attachment.
- Försäkringsmedicinskt beslutsstöd. Stockholm: Socialstyrelsen; 2022. [accessed Nov 22 2022]. Available from: https://roi.socialstyrelsen.se/fmb.
- Alexanderson K, Arrelöv B, Friberg E, Haque M, Lindholm C, Lytsy P, et al. Läkares erfarenheter av arbete med sjukskrivning av patienter. Resultat från en enkät år 2017 och jämförelser med resultat från motsvarande enkäter år 2012, 2008 respektive 2004. Huvudrapport 2018. Stockholm: Avdelningen för försäkringsmedicin Institutionen för klinisk neurovetenskap Karolinska Institutet 2018. [accessed Sep 12 2022]. Available from: https://ki.se/media/206724/download?attachment.
- Sveriges Riksdag 2019:Lag (2019:1297) om koordineringsinsatser för sjukskrivna patienter. Socialdepartementet. Stockholm. [accessed Nov 22 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/lag-20191297-om-koordineringsinsatser-for_sfs-2019-1297.
- Regeringskansliet. En kvalitetssäker och effektiv sjukskrivnings- och rehabiliteringsprocess. Överenskommelse mellan staten och Sveriges Kommuner och Landsting 2017–2018. Stockholm: Socialdepartementet; 2016. [accessed Nov 22 2022]. Available from: En kvalitetssäker och effektiv sjukskrivnings- och rehabiliteringsprocess - Regeringen.se.
- SBU. Postcovid – behandling och rehabilitering. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2022. SBU Bereder 328. [accessed Nov 22 2022]. Available from: https://www.sbu.se/328.
- Försäkringskassan. Lång väg tillbaka till arbete vid sjukskrivning. Stockholm: Avdelningen för analys och prognos. Psykiatriska diagnoser, Korta analyser 2017:1. [accessed Nov 22 2022]. Available from: psykiatriska-diagnoser-korta-analyser-2017-1.pdf (forsakringskassan.se).
- Socialstyrelsen. Internationell statistisk klassifikation av sjukdomar och relaterade hälsoproblem – Systematisk förteckning, svensk version 2018 (ICD-10-SE). Stockholm: Socialstyrelsen; 2022. [accessed Nov 22 2022]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/klassifikationer-och-koder/2022-1-7717.pdf.
- Hellman T, Wåhlin C. Företagshälsans guide om arbetsförmåga - begrepp, samtal och utredning: Sveriges företagshälsor; 2021. [accessed Aug 30 2022]. Available from: https://www.foretagshalsor.se/sites/default/files/2021-11/Arbetsfo%CC%88rma%CC%8Ageguide_2021.pdf.
- ISF. Regeringens mål om ett sjukpenningtal på 9,0 dagar. En redovisning av hur regeringen styr Försäkringskassan och hur myndigheten arbetar för att bidra till att målet uppnås 2018:17. Stockholm: Inspektionen för socialförsäkringen; 2018. [accessed Aug 30 2022]. Available from: https://isf.se/download/18.6e75aae16a591304896ba5/1565330431157/Regeringens%20ma%CC%8Al%20om%20ett%20sjukpenningtal%20pa%CC%8A%209,0%20dagar-ISF-Rapport%202018-17.pdf.
- ISF. Förändrad styrning av och i Försäkringskassan. En analys av hur regeringens mål om ett sjukpenningtal på 9,0 dagar påverkar handläggningen av sjukpenning 2018:16. Stockholm: Inspektionen för socialförsäkringen; 2018. [accessed Aug 30 2022]. Available from: https://isf.se/download/18.6e75aae16a591304896ba4/1565330431186/Fo%CC%88ra%CC%88ndrad%20styrning%20av%20och%20i%20Fo%CC%88rsa%CC%88kringskassan-ISF-Rapport%202018-16.pdf.
- Hägglund P, Johansson P. Sjukskrivningarnas anatomi – en ESO-rapport om drivkrafterna i sjukförsäkringssystemet. Rapport till Expertgruppen för studier i offentlig ekonomi 2016:2. Stockholm: Regeringskansliet Finansdepartementet; 2016. [accessed Aug 30 2022]. Available from: https://eso.expertgrupp.se/wp-content/uploads/2014/06/ESO_rapport-2016_2-160201.pdf.
- Försäkringskassan. Analys av sjukfrånvarons variation. Väsentliga förklaringar av upp- och nedgång över tid 2014:17: Försäkringskassan Analys och prognos; 2014. Socialförsäkringsrapport 2014:17. [accessed Aug 30 2022]. Available from: Analys av sjukfrånvarons variation (forsakringskassan.se).
- Ekberg K. Den relativa arbetsförmågan : teoretiska och praktiska perspektiv. Lund: Studentlitteratur AB; 2014. 198 p.
- SOU 2009:89. GRÄNSLANDET MELLAN SJUKDOM OCH ARBETE. Arbetsförmåga/Medicinska förutsättningar för arbete/Försörjningsförmåga. Statens offentliga utredningar. Stockholm: Fritzes. [accessed Aug 30 2022]. Available from: https://data.riksdagen.se/fil/5E46FC6B-173B-43BD-93EE-90785463E6CB.
- Johansson G, Lundberg I. Adjustment latitude and attendance requirements as determinants of sickness absence or attendance. Empirical tests of the illness flexibility model. Soc Sci Med. 2004;58(10):1857-68. Available from: https://doi.org/10.1016/S0277-9536(03)00407-6.
- Johansson G. The illness flexibility model and sickness absence [Dissertation]. Stockholm: Karolinska Institutet; 2007. [accessed Nov 22 2022]. Available from: https://openarchive.ki.se/xmlui/handle/10616/39462.
- Loisel P, Buchbinder R, Hazard R, Keller R, Scheel I, van Tulder M, et al. Prevention of work disability due to musculoskeletal disorders: the challenge of implementing evidence. Journal of Occupational Rehabilitation. 2005;15(4):507-24. Available from: https://doi.org/10.1007/s10926-005-8031-2.
- Law M, Cooper B, Strong S, Stewart D, Rigby P, Letts L. The Person-Environment-Occupation Model: A Transactive Approach to Occupational Performance. Canadian Journal of Occupational Therapy. 2016;63(1):9-23. Available from: https://doi.org/10.1177/000841749606300103.
- Ilmarinen JE. Aging workers. Occup Environ Med. 2001;58(8):546-52. Available from: https://doi.org/10.1136/oem.58.8.546.
- Ilmarinen J, Ilmarinen V. Work Ability and Aging. In: Finkelstein LM, Truxillo DM, Fraccaroli F, Kanfer R, editors. Facing the Challenges of a Multi-Age Workforce: A Use-Inspired Approach. SIOP Organizational Frontiers Series. New York: Routledge 2015. p. 134-56. Available from: https://helda.helsinki.fi/bitstream/handle/10138/299167/Ilmarinen_work_ability_and_aging_postprint.pdf?sequence=1.
- Ilmarinen J. From Work Ability Research to Implementation. International Journal of Environmental Research and Public Health. 2019;16(16). Available from: https://doi.org/10.3390/ijerph16162882.
- Helsingfors: Arbetshälsoinstitutet. [Available from: https://www.ttl.fi/sv/teman/arbetshalsa-och-arbetsformaga/arbetsformaga.
- Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196(4286):129-36. Available from: https://doi.org/10.1126/science.847460.
- Fava GA, Sonino N. From the Lesson of George Engel to Current Knowledge: The Biopsychosocial Model 40 Years Later. Psychotherapy and Psychosomatics. 2017;86(5):257-9. Available from: https://doi.org/10.1159/000478808.
- Palmer S, Wegener ST. Rehabilitation psychology. Overview and key concepts. Maryland Medicine. 2003;4(4):20-2.
- Hara KW, Bjorngaard JH, Jacobsen HB, Borchgrevink PC, Johnsen R, Stiles TC, et al. Biopsychosocial predictors and trajectories of work participation after transdiagnostic occupational rehabilitation of participants with mental and somatic disorders: a cohort study. BMC Public Health. 2018;18(1):1014. Available from: https://doi.org/10.1186/s12889-018-5803-0.
- Fisker J, Hjorthoj C, Hellstrom L, Mundy SS, Rosenberg NG, Eplov LF. Predictors of return to work for people on sick leave with common mental disorders: a systematic review and meta-analysis. Int Arch Occup Environ Health. 2022;95(7):1-13. Available from: https://doi.org/10.1007/s00420-021-01827-3.
- Sveriges Riksdag Arbetsmiljölag (1977:1160). ARM A. [accessed Nov 22 2022]. Available from: https://riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/arbetsmiljolag-19771160_sfs-1977-1160#K3.
- Systematiskt arbetsmiljöarbete (AFS 2001:1), föreskrifter. Arbetsmiljöverkets föreskrifter om systematiskt arbetsmiljöarbete och allmänna råd om tillämpningen av föreskrifterna. Ändringar införda t.o.m. 2008-09-30. Solna: Arbetsmiljöverket; 2001. [accessed Nov 30 2022]. Available from: https://www.av.se/globalassets/filer/publikationer/foreskrifter/systematiskt-arbetsmiljoarbete-foreskrifter-afs2001-1.pdf.
- Arbetsanpassning. Arbetsmiljöverkets föreskrifter och allmänna råd om arbetsanpassning. AFS 2020:5. Solna: Arbetsmiljöverket; 2020. [accessed Nov 30 2022]. Available from: https://www.av.se/globalassets/filer/publikationer/foreskrifter/arbetsanpassning-afs2020_5.pdf.
- FORTE. En kunskapsöversikt PSYKISK OHÄLSA, ARBETSLIV OCH SJUKFRÅNVARO. Malmö: Forte – Forskningsrådet för hälsa, arbetsliv och välfärd. [accessed Aug 30 2022]. Available from: https://forte.se/app/uploads/2015/04/psykisk-ohalsa-arbetsliv-2020.pdf.
- SBU. Arbetsmiljöns betydelse för ryggproblem. En systematisk litteraturöversikt. Stockholm: Statens beredning för medicinsk utvärdering (SBU); 2014. SBU Utvärderar 227. [accessed Oct 24 2022]. Available from: https://www.sbu.se/227.
- Ledarskap för hälsa och välbefinnande. Regeringsuppdrag att sammanställa kunskap om faktorer som skapar friska och välmående arbetsplatser A2018/01349/ARM KUNSKAPSSAMMANSTÄLLNING 2020:6. Gävle: Myndigheten för arbetsmiljökunskap (MYNAK); 2020. [accessed Nov 30 2022]. Available from: https://mynak.se/wp-content/uploads/2020/03/ledarskap-for-halsa-och-valbefinnande-kunskapssammanstallning-2020-6.pdf.
- Faktorer som skapar friska och välmående arbetsplatser. RAPPORT KS 2020:2. Gävle: Myndigheten för arbetsmiljökunskap; 2020. [accessed Sep 12 2022]. Available from: https://www.mynak.se/wp-content/uploads/2020/03/faktorer-som-skapar-friska-och-valmaende-arbetsplatser-rapport-ks-2020-2.pdf.
- Waddell G, Burton AK. IS WORK GOOD FOR YOUR HEALTH AND WELL-BEING? London (UK): TSO (The Stationery Office); 2006. [accessed Sep 12 2022]. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/209510/hwwb-is-work-good-for-you-exec-summ.pdf.
- SBU. Arbetsmiljöns betydelse för besvär och sjukdom i nacke, axlar, armar och händer Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2022. SBU Utvärderar 349. Available from: https://www.sbu.se/349.
- Försäkringsmedicinskt beslutsstöd. Stockholm: Socialstyrelsen. [accessed Nov 30 2022]. Available from: https://roi.socialstyrelsen.se/fmb.
- Fishbain DA. Multimodal Rehabilitation Treatment and Psychiatric Aspects of Multimodal Treatment for Pain. In: Gebhart GF, Schmidt RF, editors. Encyclopedia of Pain. Berlin, Heidelberg: Springer Berlin Heidelberg; 2013. p. 1938-42.
- Norrefalk JR. How do we define multidisciplinary rehabilitation? Journal of Rehabilitation Medicine. 2003;35(2):100-1. Available from: https://doi.org/10.1080/16501970306118.
- LoMartire R, Bjork M, Dahlstrom O, Constan L, Frumento P, Vixner L, et al. The value of interdisciplinary treatment for sickness absence in chronic pain: A nationwide register-based cohort study. European Journal of Pain (London, England). 2021;25(10):2190-201. Available from: https://doi.org/10.1002/ejp.1832.
- Wade DT. Describing rehabilitation interventions. Clinical Rehabilitation. 2005;19(8):811-8. Available from: https://doi.org/10.1191/0269215505cr923ed.
- SBU. Samverkan vid psykisk ohälsa inom hälso- och sjukvård, socialtjänst samt socialförsäkring. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2017. SBU Kartlägger 273. [accessed Dec 1 2022]. Available from: https://www.sbu.se/contentassets/8b34180cd1394d4b8eec8c46ffbc542f/samverkan-psykisk-ohalsa.pdf.
- Franche RL, Cullen K, Clarke J, Irvin E, Sinclair S, Frank J, et al. Workplace-based return-to-work interventions: a systematic review of the quantitative literature. Journal of Occupational Rehabilitation. 2005;15(4):607-31. Available from: https://doi.org/10.1007/s10926-005-8038-8.
- Dol M, Varatharajan S, Neiterman E, McKnight E, Crouch M, McDonald E, et al. Systematic Review of the Impact on Return to Work of Return-to-Work Coordinators. Journal of Occupational Rehabilitation. 2021;31(4):675-98. Available from: https://doi.org/10.1007/s10926-021-09975-6.
- Schandelmaier S, Ebrahim S, Burkhardt SC, de Boer WE, Zumbrunn T, Guyatt GH, et al. Return to work coordination programmes for work disability: a meta-analysis of randomised controlled trials. PloS One. 2012;7(11):e49760. Available from: https://doi.org/10.1371/journal.pone.0049760.
- Vogel N, Schandelmaier S, Zumbrunn T, Ebrahim S, de Boer WE, Busse JW, et al. Return-to-work coordination programmes for improving return to work in workers on sick leave. Cochrane Database of Systematic Reviews. 2017;3(3):CD011618. Available from: https://doi.org/10.1002/14651858.CD011618.pub2.
- MacEachen E, McDonald E, Neiterman E, McKnight E, Malachowski C, Crouch M, et al. Return to work for mental ill-health: A scoping review exploring the impact and role of return-to-work coordinators. Journal of Occupational Rehabilitation. 2020;30(3):455-65. Available from: https://doi.org/10.1007/s10926-020-09873-3.
- Eskilsson T, Lehti A, Sturesson M, Ståhlnacke BM. METODSTÖD ADA+ ArbetsplatsDialog för Arbetsåtergång; Planering, uppföljning och stöd. Umeå: Umeå universitet; 2017. [accessed Dec 1 2022]. Available from: https://www.umu.se/globalassets/centralwebb/forskningswebb/forskningsprojekt/ada-metodstod/metodstod-ada_t.pdf.
- SBU. Effekter av arbetsmarknadsinsatser för personer med varaktigt försörjningsstöd. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2022. SBU Utvärderar 351. [accessed Dec 1 2022]. Available from: https://www.sbu.se/351.
- SBU. Effekter av arbetsmarknadsinsatser för personer långvarigt sjukskrivna på grund av depression, ångest eller stressreaktion. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2022. SBU Utvärderar 352. [accessed Dec 1 2022]. Available from: https://www.sbu.se/352.
- Kazdin AE. Treatment as usual and routine care in research and clinical practice. Clinical Psychology Review. 2015;42:168-78. Available from: https://doi.org/10.1016/j.cpr.2015.08.006.
- Munder T, Geisshusler A, Krieger T, Zimmermann J, Wolf M, Berger T, et al. Intensity of Treatment as Usual and Its Impact on the Effects of Face-to-Face and Internet-Based Psychotherapy for Depression: A Preregistered Meta-Analysis of Randomized Controlled Trials. Psychotherapy and Psychosomatics. 2022;91(3):200-9. Available from: https://doi.org/10.1159/000521951.
- Wampold BE, Budge SL, Laska KM, Del Re AC, Baardseth TP, Fluckiger C, et al. Evidence-based treatments for depression and anxiety versus treatment-as-usual: a meta-analysis of direct comparisons. Clinical Psychology Review. 2011;31(8):1304-12. Available from: https://doi.org/10.1016/j.cpr.2011.07.012.
- Ravinskaya M, Verbeek JH, Langendam M, Daams JG, Hulshof CTJ, Madan I, et al. Extensive variability of work participation outcomes measured in randomized controlled trials: a systematic review. Journal of Clinical Epidemiology. 2022;142:60-99. Available from: https://doi.org/10.1016/j.jclinepi.2021.10.013.
- Development of a Core Outcome Set for Work Participation (COS-WP). Liverpool, UK: COMET Initiative. [accessed Dec 1 2022]. Available from: https://www.comet-initiative.org/Studies/Details/1195.
- SBU. Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten: en metodbok. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2020. [accessed Sep 12 2022]. Available from: https://www.sbu.se/metodbok.
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. Available from: https://doi.org/10.1136/bmj.n71.
- SBU. Individanpassat stöd till arbete (IPS) för personer med psykisk funktionsnedsättning. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2020. SBU Kommenterar 2020_10. [accessed Dec 1 2022]. Available from: https://www.sbu.se/2020_10.
- Tingulstad A, Meneses-Echavez J, Evensen LH, Bjerk M, Holte HH. Arbeidsrettede rehabiliteringstiltak ved langtidssykmelding: en systematisk oversikt [Work-related interventions for people on long-term sick leave: a systematic review] Rapport −2021. Oslo: Folkehelseinstituttet; 2021. [accessed Sep 12 2022]. Available from: https://www.fhi.no/globalassets/dokumenterfiler/rapporter/2021/arbeidsrettede-rehabiliteringstiltak-ved-langtidssykmelding-rapport-2021.pdf.
- The EndNote Team. EndNote. EndNote X9 uppl. Philadelphia, PA: Clarivate; 2013.
- Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. Journal of the Medical Library Association. 2016;104(3):240-3. Available from: https://doi.org/10.3163/1536-5050.104.3.014.
- Covidence systematic review software. Available at www.covidence.org. Melbourne, Australia: Veritas Health Innovation.
- Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ. 2020;368:l6890. Available from: https://doi.org/10.1136/bmj.l6890.
- SBU. Etiska aspekter på insatser inom hälso- och sjukvården: En vägledning för att identifiera relevanta etiska aspekter. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2021. [accessed Sep 12 2022]. Available from: www.sbu.se/globalassets/ebm/etiska_aspekter_halso_sjukvarden.pdf.
- Arends I, van der Klink JJ, van Rhenen W, de Boer MR, Bultmann U. Prevention of recurrent sickness absence in workers with common mental disorders: results of a cluster-randomised controlled trial. Occup Environ Med. 2014;71(1):21-9. Available from: https://doi.org/10.1136/oemed-2013-101412.
- Bakker IM, Terluin B, van Marwijk HW, van der Windt DA, Rijmen F, van Mechelen W, et al. A cluster-randomised trial evaluating an intervention for patients with stress-related mental disorders and sick leave in primary care. PLoS Clinical Trials. 2007;2(6):e26. Available from: https://doi.org/10.1371/journal.pctr.0020026.
- Björkelund C, Svenningsson I, Hange D, Udo C, Petersson EL, Ariai N, et al. Clinical effectiveness of care managers in collaborative care for patients with depression in Swedish primary health care: a pragmatic cluster randomized controlled trial. BMC Family Practice. 2018;19(1):28. Available from: https://doi.org/10.1186/s12875-018-0711-z.
- Brouwers EP, Tiemens BG, Terluin B, Verhaak PF. Effectiveness of an intervention to reduce sickness absence in patients with emotional distress or minor mental disorders: a randomized controlled effectiveness trial. General Hospital Psychiatry. 2006;28(3):223-9. Available from: https://doi.org/10.1016/j.genhosppsych.2006.02.005.
- Cederberg M, Alsen S, Ali L, Ekman I, Glise K, Jonsdottir IH, et al. Effects of a Person-Centered eHealth Intervention for Patients on Sick Leave Due to Common Mental Disorders (PROMISE Study): Open Randomized Controlled Trial. JMIR Ment Health. 2022;9(3):e30966. Available from: https://doi.org/10.2196/30966.
- Dalgaard VL, Aschbacher K, Andersen JH, Glasscock DJ, Willert MV, Carstensen O, et al. Return to work after work-related stress: a randomized controlled trial of a work-focused cognitive behavioral intervention. Scand J Work Environ Health. 2017;43(5):436-46. Available from: https://doi.org/10.5271/sjweh.3655.
- de Vente W, Kamphuis JH, Emmelkamp PM, Blonk RW. Individual and group cognitive-behavioral treatment for work-related stress complaints and sickness absence: a randomized controlled trial. Journal of Occupational Health Psychology. 2008;13(3):214-31. Available from: https://doi.org/10.1037/1076-8998.13.3.214.
- Finnes A, Ghaderi A, Dahl J, Nager A, Enebrink P. Randomized controlled trial of acceptance and commitment therapy and a workplace intervention for sickness absence due to mental disorders. Journal of Occupational Health Psychology. 2019;24(1):198-212. Available from: https://doi.org/10.1037/ocp0000097.
- Glasscock DJ, Carstensen O, Dalgaard VL. Recovery from work-related stress: a randomized controlled trial of a stress management intervention in a clinical sample. Int Arch Occup Environ Health. 2018;91(6):675-87. Available from: https://doi.org/10.1007/s00420-018-1314-7.
- Hees HL, de Vries G, Koeter MW, Schene AH. Adjuvant occupational therapy improves long-term depression recovery and return-to-work in good health in sick-listed employees with major depression: results of a randomised controlled trial. Occup Environ Med. 2013;70(4):252-60. Available from: https://doi.org/10.1136/oemed-2012-100789.
- Hoff A, Fisker J, Poulsen RM, Hjorthoj C, Rosenberg NK, Nordentoft M, et al. Integrating vocational rehabilitation and mental healthcare to improve the return-to-work process for people on sick leave with stress-related disorders: results from a randomized trial. Scand J Work Environ Health. 2022;48(5):361-71. Available from: https://doi.org/10.5271/sjweh.4021.
- Hoff A, Poulsen RM, Fisker J, Hjorthoj C, Rosenberg N, Nordentoft M, et al. Integrating vocational rehabilitation and mental healthcare to improve the return-to-work process for people on sick leave with depression or anxiety: results from a three-arm, parallel randomised trial. Occup Environ Med. 2022;79(2):134-42. Available from: https://doi.org/10.1136/oemed-2021-107894.
- Huibers MJ, Beurskens AJ, Van Schayck CP, Bazelmans E, Metsemakers JF, Knottnerus JA, et al. Efficacy of cognitive-behavioural therapy by general practitioners for unexplained fatigue among employees: Randomised controlled trial. British Journal of Psychiatry. 2004;184:240-6. Available from: https://doi.org/10.1192/bjp.184.3.240.
- Leone SS, Huibers MJ, Kant I, van Amelsvoort LG, van Schayck CP, Bleijenberg G, et al. Long-term efficacy of cognitive-behavioral therapy by general practitioners for fatigue: a 4-year follow-up study. Journal of Psychosomatic Research. 2006;61(5):601-7. Available from: https://doi.org/10.1016/j.jpsychores.2006.04.010.
- Keus van de Poll M, Nybergh L, Lornudd C, Hagberg J, Bodin L, Kwak L, et al. Preventing sickness absence among employees with common mental disorders or stress-related symptoms at work: a cluster randomised controlled trial of a problem-solving-based intervention conducted by the Occupational Health Services. Occup Environ Med. 2020;77(7):454-61. Available from: https://doi.org/10.1136/oemed-2019-106353.
- Noordik E, van der Klink JJ, Geskus RB, de Boer MR, van Dijk FJ, Nieuwenhuijsen K. Effectiveness of an exposure-based return-to-work program for workers on sick leave due to common mental disorders: a cluster-randomized controlled trial. Scand J Work Environ Health. 2013;39(2):144-54. Available from: https://doi.org/10.5271/sjweh.3320.
- Pedersen P, Sogaard HJ, Labriola M, Nohr EA, Jensen C. Effectiveness of psychoeducation in reducing sickness absence and improving mental health in individuals at risk of having a mental disorder: a randomised controlled trial. BMC Public Health. 2015;15:763. Available from: https://doi.org/10.1186/s12889-015-2087-5.
- Rebergen DS, Bruinvels DJ, Bezemer PD, van der Beek AJ, van Mechelen W. Guideline-based care of common mental disorders by occupational physicians (CO-OP study): a randomized controlled trial. J Occup Environ Med. 2009;51(3):305-12. Available from: https://doi.org/10.1097/JOM.0b013e3181990d32.
- Reme SE, Grasdal AL, Lovvik C, Lie SA, Overland S. Work-focused cognitive-behavioural therapy and individual job support to increase work participation in common mental disorders: a randomised controlled multicentre trial. Occup Environ Med. 2015;72(10):745-52. Available from: https://doi.org/10.1136/oemed-2014-102700.
- Overland S, Grasdal AL, Reme SE. Long-term effects on income and sickness benefits after work-focused cognitive-behavioural therapy and individual job support: a pragmatic, multicentre, randomised controlled trial. Occup Environ Med. 2018;75(10):703-8. Available from: https://doi.org/10.1136/oemed-2018-105137.
- van Beurden KM, Brouwers EPM, Joosen MCW, de Boer MR, van Weeghel J, Terluin B, et al. Effectiveness of an Intervention to Enhance Occupational Physicians' Guideline Adherence on Sickness Absence Duration in Workers with Common Mental Disorders: A Cluster-Randomized Controlled Trial. Journal of Occupational Rehabilitation. 2017;27(4):559-67. Available from: https://doi.org/10.1007/s10926-016-9682-x.
- van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ. Reducing long term sickness absence by an activating intervention in adjustment disorders: a cluster randomised controlled design. Occup Environ Med. 2003;60(6):429-37. Available from: https://doi.org/10.1136/oem.60.6.429.
- van Oostrom SH, van Mechelen W, Terluin B, de Vet HC, Knol DL, Anema JR. A workplace intervention for sick-listed employees with distress: results of a randomised controlled trial. Occup Environ Med. 2010;67(9):596-602. Available from: https://doi.org/10.1136/oem.2009.050849.
- Vlasveld MC, van der Feltz-Cornelis CM, Ader HJ, Anema JR, Hoedeman R, van Mechelen W, et al. Collaborative care for sick-listed workers with major depressive disorder: a randomised controlled trial from the Netherlands Depression Initiative aimed at return to work and depressive symptoms. Occup Environ Med. 2013;70(4):223-30. Available from: https://doi.org/10.1136/oemed-2012-100793.
- Volker D, Zijlstra-Vlasveld MC, Anema JR, Beekman AT, Brouwers EP, Emons WH, et al. Effectiveness of a blended web-based intervention on return to work for sick-listed employees with common mental disorders: results of a cluster randomized controlled trial. Journal of Medical Internet Research. 2015;17(5):e116. Available from: https://doi.org/10.2196/jmir.4097.
- de Weerd BJ, van Dijk MK, van der Linden JN, Roelen CA, Verbraak MJ. The effectiveness of a convergence dialogue meeting with the employer in promoting return to work as part of the cognitive-behavioural treatment of common mental disorders: A randomized controlled trial. Work. 2016;54(3):647-55. Available from: https://doi.org/10.3233/WOR-162307.
- Malmberg Gavelin H, Eskilsson T, Boraxbekk CJ, Josefsson M, Stigsdotter Neely A, Slunga Jarvholm L. Rehabilitation for improved cognition in patients with stress-related exhaustion disorder: RECO - a randomized clinical trial. Stress. 2018;21(4):279-91. Available from: https://doi.org/10.1080/10253890.2018.1461833.
- Nieuwenhuijsen K, Schoutens AMC, Frings-Dresen MHW, Sluiter JK. Evaluation of a randomized controlled trial on the effect on return to work with coaching combined with light therapy and pulsed electromagnetic field therapy for workers with work-related chronic stress. BMC Public Health. 2017;17(1):761. Available from: https://doi.org/10.1186/s12889-017-4720-y.
- Salomonsson S, Santoft F, Lindsater E, Ejeby K, Ljotsson B, Ost LG, et al. Cognitive-behavioural therapy and return-to-work intervention for patients on sick leave due to common mental disorders: a randomised controlled trial. Occup Environ Med. 2017;74(12):905-12. Available from: https://doi.org/10.1136/oemed-2017-104342.
- Wormgoor MEA, Indahl A, Andersen E, Egeland J. Effectiveness of Briefer Coping-Focused Psychotherapy for Common Mental Complaints on Work-Participation and Mental Health: A Pragmatic Randomized Trial with 2-Year Follow-Up. Journal of Occupational Rehabilitation. 2020;30(1):22-39. Available from: https://doi.org/10.1007/s10926-019-09841-6.
- Abasolo L, Blanco M, Bachiller J, Candelas G, Collado P, Lajas C, et al. A health system program to reduce work disability related to musculoskeletal disorders. Annals of Internal Medicine. 2005;143(6):404-14. Available from: https://doi.org/10.7326/0003-4819-143-6-200509200-00005.
- Anema JR, Steenstra IA, Bongers PM, de Vet HC, Knol DL, Loisel P, et al. Multidisciplinary rehabilitation for subacute low back pain: graded activity or workplace intervention or both? A randomized controlled trial. Spine. 2007;32(3):291-8; discussion 9-300. Available from: https://doi.org/10.1097/01.brs.0000253604.90039.ad.
- Bultmann U, Sherson D, Olsen J, Hansen CL, Lund T, Kilsgaard J. Coordinated and tailored work rehabilitation: a randomized controlled trial with economic evaluation undertaken with workers on sick leave due to musculoskeletal disorders. Journal of Occupational Rehabilitation. 2009;19(1):81-93. Available from: https://doi.org/10.1007/s10926-009-9162-7.
- Elvsåshagen H, Tellnes G, Abdelnoor MH. Does early intervention by a specialist in physical medicine and rehabilitation reduce the duration of long term sick leave among persons with musculoskeletal diseases? Norsk Epidemiologi. 2009;19(2):219-22.
- Gross DP, Asante AK, Miciak M, Battie MC, Carroll LJ, Sun A, et al. A cluster randomized clinical trial comparing functional capacity evaluation and functional interviewing as components of occupational rehabilitation programs. Journal of Occupational Rehabilitation. 2014;24(4):617-30. Available from: https://doi.org/10.1007/s10926-013-9491-4.
- Gross DP, Asante AK, Miciak M, Battie MC, Carroll LJ, Sun A, et al. Are performance-based functional assessments superior to semistructured interviews for enhancing return-to-work outcomes? Archives of Physical Medicine and Rehabilitation. 2014;95(5):807-15 e1. Available from: https://doi.org/10.1016/j.apmr.2014.01.017.
- Hagen EM, Odelien KH, Lie SA, Eriksen HR. Adding a physical exercise programme to brief intervention for low back pain patients did not increase return to work. Scandinavian Journal of Public Health. 2010;38(7):731-8. Available from: https://doi.org/10.1177/1403494810382472.
- Hagen EM, Eriksen HR, Ursin H. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain? Spine. 2000;25(15):1973-6. Available from: https://doi.org/10.1097/00007632-200008010-00017.
- Molde Hagen E, Grasdal A, Eriksen HR. Does early intervention with a light mobilization program reduce long-term sick leave for low back pain: a 3-year follow-up study. Spine. 2003;28(20):2309-15; discussion 16. Available from: https://doi.org/10.1097/01.BRS.0000085817.33211.3F.
- Haldorsen EM, Grasdal AL, Skouen JS, Risa AE, Kronholm K, Ursin H. Is there a right treatment for a particular patient group? Comparison of ordinary treatment, light multidisciplinary treatment, and extensive multidisciplinary treatment for long-term sick-listed employees with musculoskeletal pain. Pain. 2002;95(1-2):49-63. Available from: https://doi.org/10.1016/s0304-3959(01)00374-8.
- Skouen JS, Grasdal AL, Haldorsen EM, Ursin H. Relative cost-effectiveness of extensive and light multidisciplinary treatment programs versus treatment as usual for patients with chronic low back pain on long-term sick leave: randomized controlled study. Spine. 2002;27(9):901-9; discussion 9-10. Available from: https://doi.org/10.1097/00007632-200205010-00002.
- Skouen JS, Grasdal A, Haldorsen EM. Return to work after comparing outpatient multidisciplinary treatment programs versus treatment in general practice for patients with chronic widespread pain. European Journal of Pain (London, England). 2006;10(2):145-52. Available from: https://doi.org/10.1016/j.ejpain.2005.02.005.
- Heymans MW, de Vet HC, Bongers PM, Knol DL, Koes BW, van Mechelen W. The effectiveness of high-intensity versus low-intensity back schools in an occupational setting: a pragmatic randomized controlled trial. Spine. 2006;31(10):1075-82. Available from: https://doi.org/10.1097/01.brs.0000216443.46783.4d.
- Jensen IB, Bergstrom G, Ljungquist T, Bodin L, Nygren AL. A randomized controlled component analysis of a behavioral medicine rehabilitation program for chronic spinal pain: are the effects dependent on gender? Pain. 2001;91(1-2):65-78. Available from: https://doi.org/10.1016/s0304-3959(00)00420-6.
- Jensen IB, Bergstrom G, Ljungquist T, Bodin L. A 3-year follow-up of a multidisciplinary rehabilitation programme for back and neck pain. Pain. 2005;115(3):273-83. Available from: https://doi.org/10.1016/j.pain.2005.03.005.
- Busch H, Bodin L, Bergstrom G, Jensen IB. Patterns of sickness absence a decade after pain-related multidisciplinary rehabilitation. Pain. 2011;152(8):1727-33. Available from: https://doi.org/10.1016/j.pain.2011.02.004.
- Jensen C, Jensen OK, Christiansen DH, Nielsen CV. One-year follow-up in employees sick-listed because of low back pain: randomized clinical trial comparing multidisciplinary and brief intervention. Spine. 2011;36(15):1180-9. Available from: https://doi.org/10.1097/BRS.0b013e3181eba711.
- Jensen C, Jensen OK, Nielsen CV. Sustainability of return to work in sick-listed employees with low-back pain. Two-year follow-up in a randomized clinical trial comparing multidisciplinary and brief intervention. BMC Musculoskeletal Disorders. 2012;13:156. Available from: https://doi.org/10.1186/1471-2474-13-156.
- Pedersen P, Nielsen CV, Jensen OK, Jensen C, Labriola M. Employment status five years after a randomised controlled trial comparing multidisciplinary and brief intervention in employees on sick leave due to low back pain. Scandinavian Journal of Public Health. 2018;46(3):383-8. Available from: https://doi.org/10.1177/1403494817722290.
- Lambeek LC, van Mechelen W, Knol DL, Loisel P, Anema JR. Randomised controlled trial of integrated care to reduce disability from chronic low back pain in working and private life. BMJ. 2010;340:c1035. Available from: https://doi.org/10.1136/bmj.c1035.
- Lindell O, Johansson SE, Strender LE. Subacute and chronic, non-specific back and neck pain: cognitive-behavioural rehabilitation versus primary care. A randomized controlled trial. BMC Musculoskeletal Disorders. 2008;9:172. Available from: https://doi.org/10.1186/1471-2474-9-172.
- Marhold C, Linton SJ, Melin L. A cognitive-behavioral return-to-work program: effects on pain patients with a history of long-term versus short-term sick leave. Pain. 2001;91(1-2):155-63. Available from: https://doi.org/10.1016/s0304-3959(00)00431-0.
- Rossignol M, Abenhaim L, Séguin P, Neveu A, Collet J, Ducruet T, et al. Coordination of primary health care for back pain. A randomized controlled trial. Spine (03622436). 2000;25(2):251-9. Available from: https://doi.org/10.1097/00007632-200001150-00018.
- Scheel IB, Hagen KB, Herrin J, Carling C, Oxman AD. Blind faith? The effects of promoting active sick leave for back pain patients: a cluster-randomized controlled trial. Spine. 2002;27(23):2734-40. Available from: https://doi.org/10.1097/00007632-200212010-00014.
- Strand LI, Ljunggren AE, Haldorsen EM, Espehaug B. The impact of physical function and pain on work status at 1-year follow-up in patients with back pain. Spine. 2001;26(7):800-8. Available from: https://doi.org/10.1097/00007632-200104010-00022.
- Verbeek JH, van der Weide WE, van Dijk FJ. Early occupational health management of patients with back pain: a randomized controlled trial. Spine. 2002;27(17):1844-51; discussion 51. Available from: https://doi.org/10.1097/00007632-200209010-00006.
- Vermeulen SJ, Anema JR, Schellart AJ, Knol DL, van Mechelen W, van der Beek AJ. A participatory return-to-work intervention for temporary agency workers and unemployed workers sick-listed due to musculoskeletal disorders: results of a randomized controlled trial. Journal of Occupational Rehabilitation. 2011;21(3):313-24. Available from: https://doi.org/10.1007/s10926-011-9291-7.
- Brendbekken R, Eriksen HR, Grasdal A, Harris A, Hagen EM, Tangen T. Return to Work in Patients with Chronic Musculoskeletal Pain: Multidisciplinary Intervention Versus Brief Intervention: A Randomized Clinical Trial. Journal of Occupational Rehabilitation. 2017;27(1):82-91. Available from: https://doi.org/10.1007/s10926-016-9634-5.
- Brendbekken R, Vaktskjold A, Harris A, Tangen T. Predictors of return-to-work in patients with chronic musculoskeletal pain: A randomized clinical trial. Journal of Rehabilitation Medicine. 2018;50(2):193-9. Available from: https://doi.org/10.2340/16501977-2296.
- Du Bois M, Donceel P. Guiding low back claimants to work: a randomized controlled trial. Spine. 2012;37(17):1425-31. Available from: https://doi.org/10.1097/BRS.0b013e31824e4ada.
- Harris A, Moe TF, Eriksen HR, Tangen T, Lie SA, Tveito TH, et al. Brief intervention, physical exercise and cognitive behavioural group therapy for patients with chronic low back pain (The CINS trial). European Journal of Pain (London, England). 2017;21(8):1397-407. Available from: https://doi.org/10.1002/ejp.1041.
- Reme SE, Tveito TH, Harris A, Lie SA, Grasdal A, Indahl A, et al. Cognitive Interventions and Nutritional Supplements (The CINS Trial): A Randomized Controlled, Multicenter Trial Comparing a Brief Intervention With Additional Cognitive Behavioral Therapy, Seal Oil, and Soy Oil for Sick-Listed Low Back Pain Patients. Spine. 2016;41(20):1557-64. Available from: https://doi.org/10.1097/BRS.0000000000001596.
- Kool J, Bachmann S, Oesch P, Knuesel O, Ambergen T, de Bie R, et al. Function-centered rehabilitation increases work days in patients with nonacute nonspecific low back pain: 1-year results from a randomized controlled trial. Archives of Physical Medicine and Rehabilitation. 2007;88(9):1089-94. Available from: https://doi.org/10.1016/j.apmr.2007.05.022.
- Langagergaard V, Jensen OK, Nielsen CV, Jensen C, Labriola M, Sorensen VN, et al. The comparative effects of brief or multidisciplinary intervention on return to work at 1 year in employees on sick leave due to low back pain: A randomized controlled trial. Clinical Rehabilitation. 2021;35(9):1290-304. Available from: https://doi.org/10.1177/02692155211005387.
- Pedersen KKW, Langagergaard V, Jensen OK, Nielsen CV, Sorensen VN, Pedersen P. Two-Year Follow-Up on Return to Work in a Randomised Controlled Trial Comparing Brief and Multidisciplinary Intervention in Employees on Sick Leave Due to Low Back Pain. Journal of Occupational Rehabilitation. 2022;32(4):697-704. Available from: https://doi.org/10.1007/s10926-022-10030-1.
- Moll LT, Jensen OK, Schiottz-Christensen B, Stapelfeldt CM, Christiansen DH, Nielsen CV, et al. Return to Work in Employees on Sick Leave due to Neck or Shoulder Pain: A Randomized Clinical Trial Comparing Multidisciplinary and Brief Intervention with One-Year Register-Based Follow-Up. Journal of Occupational Rehabilitation. 2018;28(2):346-56. Available from: https://doi.org/10.1007/s10926-017-9727-9.
- Myhre K, Marchand GH, Leivseth G, Keller A, Bautz-Holter E, Sandvik L, et al. The effect of work-focused rehabilitation among patients with neck and back pain: a randomized controlled trial. Spine. 2014;39(24):1999-2006. Available from: https://doi.org/10.1097/BRS.0000000000000610.
- Marchand GH, Myhre K, Leivseth G, Sandvik L, Lau B, Bautz-Holter E, et al. Change in pain, disability and influence of fear-avoidance in a work-focused intervention on neck and back pain: a randomized controlled trial. BMC Musculoskeletal Disorders. 2015;16:94. Available from: https://doi.org/10.1186/s12891-015-0553-y.
- Schweikert B, Jacobi E, Seitz R, Cziske R, Ehlert A, Knab J, et al. Effectiveness and cost-effectiveness of adding a cognitive behavioral treatment to the rehabilitation of chronic low back pain. Journal of Rheumatology. 2006;33(12):2519-26.
- van den Hout JH, Vlaeyen JW, Heuts PH, Zijlema JH, Wijnen JA. Secondary prevention of work-related disability in nonspecific low back pain: does problem-solving therapy help? A randomized clinical trial. Clinical Journal of Pain. 2003;19(2):87-96. Available from: https://doi.org/10.1097/00002508-200303000-00003.
- Viikari-Juntura E, Kausto J, Shiri R, Kaila-Kangas L, Takala EP, Karppinen J, et al. Return to work after early part-time sick leave due to musculoskeletal disorders: a randomized controlled trial. Scand J Work Environ Health. 2012;38(2):134-43. Available from: https://doi.org/10.5271/sjweh.3258.
- Carlsson L, Englund L, Hallqvist J, Wallman T. Early multidisciplinary assessment was associated with longer periods of sick leave: a randomized controlled trial in a primary health care centre. Scandinavian Journal of Primary Health Care. 2013;31(3):141-6. Available from: https://doi.org/10.3109/02813432.2013.811943.
- Fleten N, Johnsen R. Reducing sick leave by minimal postal intervention: a randomised, controlled intervention study. Occup Environ Med. 2006;63(10):676-82. Available from: https://doi.org/10.1136/oem.2005.020438.
- Nystuen P, Hagen KB. Solution-focused intervention for sick listed employees with psychological problems or muscle skeletal pain: a randomised controlled trial [ISRCTN39140363]. BMC Public Health. 2006;6:69. Available from: https://doi.org/10.1186/1471-2458-6-69.
- Brattberg G. Internet-based rehabilitation for individuals with chronic pain and burnout II: a long-term follow-up. International Journal of Rehabilitation Research. 2007;30(3):231-4. Available from: https://doi.org/10.1097/MRR.0b013e32829fa545.
- Aasdahl L, Pape K, Vasseljen O, Johnsen R, Gismervik S, Halsteinli V, et al. Effect of Inpatient Multicomponent Occupational Rehabilitation Versus Less Comprehensive Outpatient Rehabilitation on Sickness Absence in Persons with Musculoskeletal- or Mental Health Disorders: A Randomized Clinical Trial. Journal of Occupational Rehabilitation. 2018;28(1):170-9. Available from: https://doi.org/10.1007/s10926-017-9708-z.
- Gismervik SO, Aasdahl L, Vasseljen O, Fors EA, Rise MB, Johnsen R, et al. Inpatient multimodal occupational rehabilitation reduces sickness absence among individuals with musculoskeletal and common mental health disorders: a randomized clinical trial. Scand J Work Environ Health. 2020;46(4):364-72. Available from: https://doi.org/10.5271/sjweh.3882.
- Aasdahl L, Vasseljen O, Gismervik SO, Johnsen R, Fimland MS. Two-Year Follow-Up of a Randomized Clinical Trial of Inpatient Multimodal Occupational Rehabilitation Vs Outpatient Acceptance and Commitment Therapy for Sick Listed Workers with Musculoskeletal or Common Mental Disorders. Journal of Occupational Rehabilitation. 2021;31(4):721-8. Available from: https://doi.org/10.1007/s10926-021-09969-4.
- Hara KW, Bjorngaard JH, Brage S, Borchgrevink PC, Halsteinli V, Stiles TC, et al. Randomized Controlled Trial of Adding Telephone Follow-Up to an Occupational Rehabilitation Program to Increase Work Participation. Journal of Occupational Rehabilitation. 2018;28(2):265-78. Available from: https://doi.org/10.1007/s10926-017-9711-4.
- Skagseth M, Fimland MS, Rise MB, Johnsen R, Borchgrevink PC, Aasdahl L. Effectiveness of adding a workplace intervention to an inpatient multimodal occupational rehabilitation program: A randomized clinical trial. Scand J Work Environ Health. 2020;46(4):356-63. Available from: https://doi.org/10.5271/sjweh.3873.
- Bjorneklett HG, Rosenblad A, Lindemalm C, Ojutkangas ML, Letocha H, Strang P, et al. A randomized controlled trial of support group intervention after breast cancer treatment: results on sick leave, health care utilization and health economy. Acta Oncologica. 2013;52(1):38-47. Available from: https://doi.org/10.3109/0284186X.2012.734921.
- Tamminga SJ, Verbeek JH, Bos MM, Fons G, Kitzen JJ, Plaisier PW, et al. Effectiveness of a hospital-based work support intervention for female cancer patients - a multi-centre randomised controlled trial. PloS One. 2013;8(5):e63271. Available from: https://doi.org/10.1371/journal.pone.0063271.
- Tamminga SJ, Verbeek J, Bos M, Fons G, Kitzen J, Plaisier PW, et al. Two-Year Follow-Up of a Multi-centre Randomized Controlled Trial to Study Effectiveness of a Hospital-Based Work Support Intervention for Cancer Patients. Journal of Occupational Rehabilitation. 2019;29(4):701-10. Available from: https://doi.org/10.1007/s10926-019-09831-8.
- Brouwers EP, de Bruijne MC, Terluin B, Tiemens BG, Verhaak PF. Cost-effectiveness of an activating intervention by social workers for patients with minor mental disorders on sick leave: a randomized controlled trial. European Journal of Public Health. 2007;17(2):214-20. Available from: https://doi.org/10.1093/eurpub/ckl099.
- Hlobil H, Staal JB, Twisk J, Koke A, Ariens G, Smid T, et al. The effects of a graded activity intervention for low back pain in occupational health on sick leave, functional status and pain: 12-month results of a randomized controlled trial. Journal of Occupational Rehabilitation. 2005;15(4):569-80. Available from: https://doi.org/10.1007/s10926-005-8035-y.
- Staal JB, Hlobil H, Twisk JW, Smid T, Koke AJ, van Mechelen W. Graded activity for low back pain in occupational health care: a randomized, controlled trial. Annals of Internal Medicine. 2004;140(2):77-84. Available from: https://doi.org/10.7326/0003-4819-140-2-200401200-00007.
- Steenstra IA, Anema JR, Bongers PM, de Vet HC, Knol DL, van Mechelen W. The effectiveness of graded activity for low back pain in occupational healthcare. Occup Environ Med. 2006;63(11):718-25. Available from: https://doi.org/10.1136/oem.2005.021675.
- Salomonsson S, Santoft F, Lindsater E, Ejeby K, Ingvar M, Ljotsson B, et al. Effects of cognitive behavioural therapy and return-to-work intervention for patients on sick leave due to stress-related disorders: Results from a randomized trial. Scandinavian Journal of Psychology. 2020;61(2):281-9. Available from: https://doi.org/10.1111/sjop.12590.
- Aanesen F, Berg R, Lochting I, Tingulstad A, Eik H, Storheim K, et al. Motivational Interviewing and Return to Work for People with Musculoskeletal Disorders: A Systematic Mapping Review. Journal of Occupational Rehabilitation. 2021;31(1):63-71. Available from: https://doi.org/10.1007/s10926-020-09892-0.
- Arends I, Bruinvels DJ, Rebergen DS, Nieuwenhuijsen K, Madan I, Neumeyer-Gromen A, et al. Interventions to facilitate return to work in adults with adjustment disorders. Cochrane Database of Systematic Reviews. 2012;12:CD006389. Available from: https://doi.org/10.1002/14651858.CD006389.pub2.
- Axen I, Bjork Bramberg E, Vaez M, Lundin A, Bergstrom G. Interventions for common mental disorders in the occupational health service: a systematic review with a narrative synthesis. Int Arch Occup Environ Health. 2020;93(7):823-38. Available from: https://doi.org/10.1007/s00420-020-01535-4.
- Cullen KL, Irvin E, Collie A, Clay F, Gensby U, Jennings PA, et al. Effectiveness of Workplace Interventions in Return-to-Work for Musculoskeletal, Pain-Related and Mental Health Conditions: An Update of the Evidence and Messages for Practitioners. Journal of Occupational Rehabilitation. 2018;28(1):1-15. Available from: https://doi.org/10.1007/s10926-016-9690-x.
- Doki S, Sasahara S, Matsuzaki I. Psychological approach of occupational health service to sick leave due to mental problems: a systematic review and meta-analysis. Int Arch Occup Environ Health. 2015;88(6):659-67. Available from: https://doi.org/10.1007/s00420-014-0996-8.
- Finnes A, Enebrink P, Ghaderi A, Dahl J, Nager A, Ost LG. Psychological treatments for return to work in individuals on sickness absence due to common mental disorders or musculoskeletal disorders: a systematic review and meta-analysis of randomized-controlled trials. Int Arch Occup Environ Health. 2019;92(3):273-93. Available from: https://doi.org/10.1007/s00420-018-1380-x.
- Nieuwenhuijsen K, Bultmann U, Neumeyer-Gromen A, Verhoeven AC, Verbeek JH, van der Feltz-Cornelis CM. Interventions to improve occupational health in depressed people. Cochrane Database of Systematic Reviews. 2008(2):CD006237. Available from: https://doi.org/10.1002/14651858.CD006237.pub2.
- Nigatu YT, Liu Y, Uppal M, McKinney S, Rao S, Gillis K, et al. Interventions for enhancing return to work in individuals with a common mental illness: systematic review and meta-analysis of randomized controlled trials. Psychological Medicine. 2016;46(16):3263-74. Available from: https://doi.org/10.1017/S0033291716002269.
- Schaafsma FG, Whelan K, van der Beek AJ, van der Es-Lambeek LC, Ojajarvi A, Verbeek JH. Physical conditioning as part of a return to work strategy to reduce sickness absence for workers with back pain. Cochrane Database of Systematic Reviews. 2013;2013(8):CD001822. Available from: https://doi.org/10.1002/14651858.CD001822.pub3.
- Wainwright E, Wainwright D, Coghill N, Walsh J, Perry R. Resilience and return-to-work pain interventions: systematic review. Occupational Medicine (Oxford, England). 2019;69(3):163-76. Available from: https://doi.org/10.1093/occmed/kqz012.
- Finnes A, Enebrink P, Sampaio F, Sorjonen K, Dahl J, Ghaderi A, et al. Cost-Effectiveness of Acceptance and Commitment Therapy and a Workplace Intervention for Employees on Sickness Absence due to Mental Disorders. J Occup Environ Med. 2017;59(12):1211-20. Available from: https://doi.org/10.1097/JOM.0000000000001156.
- Keus Van De Poll M, Bergstrom G, Jensen I, Nybergh L, Kwak L, Lornudd C, et al. Cost-Effectiveness of a Problem-Solving Intervention Aimed to Prevent Sickness Absence among Employees with Common Mental Disorders or Occupational Stress. International Journal of Environmental Research and Public Health. 2020;17(14):1‐15. Available from: https://doi.org/10.3390/ijerph17145234.
- Arends I, Bultmann U, van Rhenen W, Groen H, van der Klink JJ. Economic evaluation of a problem solving intervention to prevent recurrent sickness absence in workers with common mental disorders. PloS One. 2013;8(8):e71937. Available from: https://doi.org/10.1371/journal.pone.0071937.
- Dewa CS, Hoch JS, Loong D, Trojanowski L, Bonato S. Evidence for the Cost-Effectiveness of Return-to-Work Interventions for Mental Illness Related Sickness Absences: A Systematic Literature Review. Journal of Occupational Rehabilitation. 2021;31(1):26-40. Available from: https://doi.org/10.1007/s10926-020-09904-z.
- Workplace health: longterm sickness absence and capability to work. Evidence reviews for workplace health: cost effectiveness outcomes. NICE guideline NG146 Evidence reviews. London, UK: National Institute for Health and Care Excellence, (NICE); 2019. [accessed Dec 6 2022]. Available from: https://www.nice.org.uk/guidance/ng146/evidence/cost-effectiveness-outcomes-pdf-6967146929.
- C-CEMG-EPPI Cost Converter. London: The Cochrane and Campbell Economic Methods Group; 2022. [accessed Sep 12 2022]. Available from: https://methods.cochrane.org/economics/workshops.
- Goorden M, Vlasveld MC, Anema JR, van Mechelen W, Beekman AT, Hoedeman R, et al. Cost-utility analysis of a collaborative care intervention for major depressive disorder in an occupational healthcare setting. Journal of Occupational Rehabilitation. 2014;24(3):555-62. Available from: https://doi.org/10.1007/s10926-013-9483-4.
- Rebergen DS, Bruinvels DJ, van Tulder MW, van der Beek AJ, van Mechelen W. Cost-effectiveness of guideline-based care for workers with mental health problems. J Occup Environ Med. 2009;51(3):313-22. Available from: https://doi.org/10.1097/JOM.0b013e3181990d8e.
- van Oostrom SH, Heymans MW, de Vet HC, van Tulder MW, van Mechelen W, Anema JR. Economic evaluation of a workplace intervention for sick-listed employees with distress. Occup Environ Med. 2010;67(9):603-10. Available from: https://doi.org/10.1136/oem.2009.051979.
- Lambeek LC, Bosmans JE, Van Royen BJ, Van Tulder MW, Van Mechelen W, Anema JR. Effect of integrated care for sick listed patients with chronic low back pain: economic evaluation alongside a randomised controlled trial. BMJ. 2010;341:c6414. Available from: https://doi.org/10.1136/bmj.c6414.
- Steenstra IA, Anema JR, van Tulder MW, Bongers PM, de Vet HC, van Mechelen W. Economic evaluation of a multi-stage return to work program for workers on sick-leave due to low back pain. Journal of Occupational Rehabilitation. 2006;16(4):557-78. Available from: https://doi.org/10.1007/s10926-006-9053-0.
- Sociala avgifter. Stockholm: Ekonomifakta. [accessed Dec 6 2022]. Available from: https://www.ekonomifakta.se/Fakta/Skatter/Skatt-pa-arbete/Sociala-avgifter/.
- Läkarförbundets etiska regler. Stockholm: Sveriges läkarförbund. [accessed Dec 6 2022]. Available from: https://slf.se/rad-och-stod/etik/lakarforbundets-etiska-regler/.
- Kadowaki Å. Svensk sjukvård till vanvett : om patienten bestämmer... BoD; 2018.
- Sveriges Riksdag Lag (2019:1297) om koordineringsinsatser för sjukskrivna patienter. Socialdepartementet. Stockholm. [accessed Dec 6 2022].
- Koordineringsinsatser inom hälso- och sjukvården. En nationell kartläggning 2021 och jämförelse med 2018. Stockholm: Sveriges Kommuner och Regioner (SKR); 2022. [accessed Dec 6 2022]. Available from: https://e-handel.skr.se/bilder/artiklar/pdf/8047-004-9.pdf?issuusl=ignore.
- Nordling P, Alexanderson K, Hensing G, Lytsy P. Factors associated with general practitioners' contacts with sick-listed patients' employers: A Swedish nationwide questionnaire study. Scandinavian Journal of Public Health. 2021;0(0):14034948211053141. Available from: https://doi.org/10.1177/14034948211053141.
- Rehabiliteringskedjan. Stockholm: Försäkringskassan. [Available from: https://www.forsakringskassan.se/om-forsakringskassan/vart-uppdrag/om-socialforsakringen/rehabiliteringskedjan.
- 2022:Dir. 2022:63. Utredning om läkarintygets betydelse i sjukpenningärenden. Stockholm: Regeringskansliet. [accessed Dec 6 2022]. Available from: https://www.regeringen.se/rattsliga-dokument/kommittedirektiv/2022/06/dir.-202263/.
- Skillnader i avslag för sjukpenning mellan olika grupper. En registerstudie om avslagsbeslut på initial ansökan och efter dag 180 i rehabiliteringskedjan. Stockholm: Försäkringskassan, Analysavdelningen. Socialförsäkringsrapport 2022:1. [accessed Dec 6 2022]. Available from: https://www.forsakringskassan.se/download/18.7fc616c01814e179a9f30c/1656597702920/skillnader-i-avslag-for-sjukpenning-mellan-olika-grupper-socialforsakringsrapport-2022-1.pdf.
- Upmark M, Hagberg J, Alexanderson K. Negative encounters with social insurance officers – experiences of women and men on long‐term sick leave. International Journal of Social Welfare. 2011;20(3):309-17. Available from: https://doi.org/10.1111/j.1468-2397.2009.00702.x.
- SYSTEMATISKT ARBETSMILJÖARBETE Arbetsmiljöverkets föreskrifter om systematiskt arbetsmiljöarbete och allmänna råd om tillämpningen av föreskrifterna. AFS 2001:1. Solna: Arbetsmiljöverket; 2001. [accessed Dec 7 2022]. Available from: https://www.av.se/globalassets/filer/publikationer/foreskrifter/systematiskt-arbetsmiljoarbete-foreskrifter-afs2001-1.pdf.
- Bengtsson M, Carlsson L, Oldertz C, Nikolovska S. Förstärkt rehabilitering för återgång i arbete. Göteborg: Inspektionen för socialförsäkringen (ISF). [accessed Dec 12 2022]. Available from: https://isf.se/publikationer/rapporter/2021/2021-11-30-forstarkt-rehabilitering-for-atergang-i-arbete.
- Blomberg A, Hensing G, Bertilsson M. Chefens perspektiv en saknad pusselbit. En webbaserad enkät om svenska chefers kunskap, erfarenheter och strategier för medarbetare med nedsatt arbetsförmåga på grund av depression och ångest: Göteborgs universitet, Sahlgrenska akademin. [accessed Dec 12 2022]. Available from: https://gup.ub.gu.se/file/208297.
- SBU. Arbetsmiljöns betydelse för artrosbesvär. En systematisk översikt och utvärdering av medicinska, sociala och etiska aspekter. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2016. SBU Utvärderar 253. [accessed Dec 12 2022]. Available from: https://www.sbu.se/sv/publikationer/SBU-utvarderar/arbetsmiljons-betydelse-for-artrosbesvar/.
- SBU. Arbetsmiljöns betydelse för symtom på depression och utmattningssyndrom. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2014. SBU Utvärderar 223. [accessed Dec 12 2022]. Available from: https://www.sbu.se/sv/publikationer/SBU-utvarderar/arbetsmiljons-betydelse-for-symtom-pa-depression-och-utmattningssyndrom/.
- Shutzberg M. Doctors that “doctor” sickness certificates: cunning intelligence as an ability and possibly a virtue among Swedish GPs. Medicine, Health Care and Philosophy. 2020;23(3):445-56. Available from: https://doi.org/10.1007/s11019-020-09954-3.
- Sveriges Riksdag 2017:Hälso- och sjukvårdslag (2017:30). Socialdepartementet. Stockholm. [accessed Dec 12 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/halso--och-sjukvardslag_sfs-2017-30#K3.
- Sveriges Riksdag Patientlag (2014:821). Socialdepartementet. Stockholm. [accessed Dec 12 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/patientlag-2014821_sfs-2014-821#K4.
- Holmlund L, Sandman L, Hellman T, Kwak L, Björk Brämberg E. Ethical aspects of the coordination of return-to-work among employees on sick leave due to common mental disorders: a qualitative study. Disability and Rehabilitation. 2022:1-10. Available from: https://doi.org/10.1080/09638288.2022.2084779.
- Socialförsäkringen i siffror 2021. Stockholm: Försäkringskassan; 2021. [accessed Dec 12 2022]. Available from: https://www.forsakringskassan.se/download/18.3dc760f6179960511041308/1628676456116/socialforsakringen-i-siffror-2021.pdf.
- Regeringskansliet 2018:Regleringsbrev för budgetåret 2018 avseende Försäkringskassan. S2019/00547/SF. [Available from: https://www.esv.se/statsliggaren/regleringsbrev/?rbid=19877.
- Regeringens mål om ett sjukpenningtal på 9,0 dagar. En redovisning av hur regeringen styr Försäkringskassan och hur myndigheten arbetar för att bidra till att målet uppnås. Göteborg: Inspektionen för socialförsäkringen (ISF); 2018 17. [accessed Dec 12 2022]. Available from: https://isf.se/download/18.6e75aae16a591304896ba5/1565330431157/Regeringens%20ma%CC%8Al%20om%20ett%20sjukpenningtal%20pa%CC%8A%209,0%20dagar-ISF-Rapport%202018-17.pdf.
- Förändrad styrning av och i Försäkringskassan. En analys av hur regeringens mål om ett sjukpenningtal på 9,0 dagar påverkar handläggningen av sjukpenning. Göteborg: Inspektionen för socialförsäkringen (ISF); 2018 6. [accessed Dec 12 2022]. Available from: https://isf.se/download/18.6e75aae16a591304896ba4/1565330431186/Fo%CC%88ra%CC%88ndrad%20styrning%20av%20och%20i%20Fo%CC%88rsa%CC%88kringskassan-ISF-Rapport%202018-16.pdf.
- Psykosocial arbetsmiljö – hälsa och välbefinnande. KUNSKAPSSAMMANSTÄLLNING 2020:5. Gävle: Myndigheten för arbetsmiljökunskap, MYNAK. [accessed Dec 12 2022]. Available from: https://mynak.se/wp-content/uploads/2021/12/psykosocial-arbetsmiljo-halsa-och-valbefinnande-kunskapssammanstallning-2021-12.pdf.
- Sennehed CP, Holmberg S, Stigmar K, Forsbrand M, Petersson IF, Nyberg A, et al. Referring to multimodal rehabilitation for patients with musculoskeletal disorders – a register study in primary health care. BMC Health Services Research. 2017;17(1):15. Available from: https://doi.org/10.1186/s12913-016-1948-7.
- Sveriges Riksdag Socialförsäkringsbalk (2010:110). Socialdepartementet. Stockholm. [accessed Dec 12 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/socialforsakringsbalk-2010110_sfs-2010-110#K30.
- Lytsy P, Larsson K, Anderzén I. Health in women on long-term sick leave because of pain or mental illness. International Journal of Rehabilitation Research. 2015;38(1):27-33. Available from: https://doi.org/10.1097/mrr.0000000000000080.
- Liedberg GM, Björk M, Dragioti E, Turesson C. Qualitative evidence from studies of interventions aimed at return to work and staying at work for persons with chronic musculoskeletal pain. Journal of Clinical Medicine. 2021;10(6):1-21. Available from: https://doi.org/10.3390/jcm10061247.
- På tal om kvinnor och män. Lathund om jämställdhet. Stockholm: Statistiska centralbyrån, SCB; 2022. [accessed Dec 14 2022]. Available from: https://www.scb.se/contentassets/b3ba3d3ad7a74749936c7fd2e3b4bee6/le0201_2021b22_x10br2201.pdf.
- Socialstyrelsen. Utmattningssyndrom. Stressrelaterad psykisk ohälsa. Stockholm: Socialstyrelsen; 2003.
- Försäkringskassan. Sjukfrånvaro i psykiatriska diagnoser. En registerstudie av Sveriges arbetande befolkning i åldern 20–69 år. Stockholm: Försäkringskassan; 2020. Socialförsäkringsrapport 2020:8. [accessed Dec 14 2022]. Available from: https://www.forsakringskassan.se/download/18.7fc616c01814e179a9f329/1656660446139/sjukfranvaro-i-psykiatriska-diagnoser-socialforsakringsrapport-2020-8.pdf.
- Lindsäter E, Svärdman F, Wallert J, Ivanova E, Söderholm A, Fondberg R, et al. Exhaustion disorder: scoping review of research on a recently introduced stress-related diagnosis. BJPsych Open. 2022;8(5):e159. Available from: https://doi.org/10.1192/bjo.2022.559.
- Wallensten J, Asberg M, Wiklander M, Nager A. Role of rehabilitation in chronic stress-induced exhaustion disorder: A narrative review. Journal of Rehabilitation Medicine. 2019;51(5):331-42. Available from: https://doi.org/10.2340/16501977-2545.
- Lindegård A, Glise K, Wiegner L, Reinhardt P, Ellbin S, Pettersson S, et al. Effects of Additional Individually Tailored Interventions on Sick-Leave and Symptoms in Patients with Exhaustion Disorder: A Randomized Controlled Trial. Journal of Rehabilitation Medicine. 2022;54:jrm00321. Available from: https://doi.org/10.2340/jrm.v54.2941.
- Andersen A, Berglund E, Anderzen I. Rehabilitation coordinator intervention versus control in psychiatric specialist care for return to work and reduced sick leave: study protocol of a randomised controlled trial. BMC Public Health. 2020;20(1):250. Available from: https://dx.doi.org/10.1186/s12889-020-8238-3.
- Munthe-Kaas H, Nøkleby H, Lewin S, Glenton C. The TRANSFER Approach for assessing the transferability of systematic review findings. BMC Medical Research Methodology. 2020;20(1):11. Available from: https://doi.org/10.1186/s12874-019-0834-5.
- Sennehed CP, Stigmar K, Grahn B, Fischer MR, Forsbrand M, Nyberg A, et al. Evaluation of a multimodal pain rehabilitation programme in primary care based on clinical register data: a feasibility study. Primary Health Care Research & Development. 2020;21:e2. Available from: https://doi.org/https://dx.doi.org/10.1017/S1463423619000884.
- Aasdahl L, Fimland MS. Is there really a "golden hour" for work disability interventions? A narrative review. Disability and Rehabilitation. 2020;42(4):586-93. Available from: https://dx.doi.org/10.1080/09638288.2018.1503735.
- Bell E, Taylor M. Workplace Health: Long-Term Sickness Absence and Capability to Work. London, UK: The National Institute for Health and Care Excellence, NICE; 2019. [accessed Dec 14 2022]. Available from: https://www.nice.org.uk/guidance/ng146/evidence/economic-modelling-report-pdf-6967149517.
- Squires H, Rick J, Carroll C, Hillage J. Cost-effectiveness of interventions to return employees to work following long-term sickness absence due to musculoskeletal disorders. J Public Health (Oxf). 2012;34(1):115-24. Available from: https://doi.org/10.1093/pubmed/fdr057.
 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services



