Wheelchairs and wheelchair accessories
A systematic review and assessment of medical, economic, social and ethical aspects
Conclusions
Experiences of evaluated interventions
- Studies with a qualitative approach show that wheelchair users feel that the electric wheelchair contributes to participation and independence (high reliability) and that its usability contributes to activity (moderate reliability). For a wheelchair to function well users' experience is that practical training, knowledge, and information are needed (moderate reliability), as is access to service (low reliability) and that the wheelchair is adjusted based on individual needs (low reliability).
Effect of evaluated interventions
- There is a need for more research in order to assess how activity, participation, freedom of action, quality of life, and health for adults, or young people and children are affected by:
different variants, combinations, and individual adaptations of wheelchairs, additional equipment for manual wheelchairs, as well as freedom to be able to choose a wheelchair and additional equipment (freedom of choice) and exemption from fees. - It is possible that practically oriented educational and the wheelchair skills training programs (WSTP, WheelSeeYou, EpicWheels) can lead to better maneuverability for adult users (low reliability). For children and young people who use wheelchairs, there is a lack of scientific studies on the effect of such programs on activity and health program.
Cost effectiveness
There is a lack of evidence to calculate the cost-effectiveness of having both electric and manual wheelchair instead of only manual wheelchair.
Background
For many people with reduced mobility, the wheelchair is a prerequisite for being able to participate and be active in society. The wheelchair's characteristics and design, how it can be run and used, as well as access to additional wheelchair equipment can affect the user’s possibilities for participation and freedom of action. Fees can be particularly difficult for people who rely on a wheelchair, as people with disabilities have, in general, a lower socioeconomic status compared to their peers without disabilities.
Aim
The aim of this systematic review was to evaluate the effect of different variants, combinations, and individual adaptations of wheelchairs
- additional equipment for manual wheelchairs
- education and practical training for wheelchair users as well as
- freedom to be able to choose a wheelchair and additional equipment, exemption from fees
on the individual's activity, participation, freedom of action, quality of life and health, as well as on user’s experiences of using a wheelchair.
To make informed decisions about resource distribution municipalities and regions need to understand not only how factors related to wheelchairs affect individuals, but also the impact of those factors affect resource consumption. Therefore, this report also highlights financial aspects.
The evaluation concerns people of all ages, with permanently reduced mobility, who use a wheelchair they operate themselves (self-propelled).
Method
This systematic review follows the international guidelines PRISMA and SBU's method book.
Results
Experiences of evaluated efforts
A meta-synthesis was made based on 20 studies that investigated user experiences. Most studies were carried out in Europe and North America. Data was primarily collected through interviews and focus groups. The result of the meta synthesis was that experiences were linked to five themes and 15 sub-themes.
Effect of evaluated efforts
The 17 primary studies that addressed efficacy recruited people between 18–89 years, most of whom were men. None of the primary studies applied to children and young people (<18 years). Primary studies were found which investigated the following three questions:
- Has the use of different variants of electric wheelchairs effect on wheelchair maneuverability and mobility?
- Do individualized wheelchair settings have an effect when it comes to wheelchair maneuverability?
- Has practical education and training in the use of a wheelchair and additional equipment for wheelchair effect in terms of wheelchair maneuverability and usefulness?
- No studies were identified for thirteen of the study questions.
Cost effectiveness
When resources are limited, decisions must be made about how different needs are to be met and prioritized. A cost-effectiveness analysis compares two or more alternatives by identifying, quantifying and evaluate costs and effects for different efforts. The systematic review of economic literature aimed to investigate the cost-effectiveness of an electric wheelchair as a complement to a manual wheelchair compared to a manual wheelchair alone. The overview generated three studies with medium and high transferability, but these were excluded due to low quality. There is a lack of studies of good quality that examine the effect and resource consumption. The cost-effectiveness has not been able to be calculated for the combination of an electric and manual wheelchair compared to a manual wheelchair alone. Based on collected data from two regions and two municipalities, it appears that the cost of electric wheelchairs varies. Further, the cost of interventions that can be important supplements to a wheelchair varies, such as home care and transportation service, both within and between municipalities. This means that the opportunity cost in economic analyzes varies.
Discussion, ethical and societal aspects
The wheelchair in context
The purpose of the wheelchair is to compensate for reduced mobility. The wheelchair can, in some cases, compensate for deficiencies in society's physical design. However, to achieve freedom of action, equal opportunities for activity and full participation in society must be available to everyone. A person who uses a wheelchair may also need other interventions to be able to be active and participate in social life. Aids and interventions must be synchronized, across different stakeholders such as municipalities and regions, based on the individual's needs and conditions. The quantitative studies in this systematic review indicate that there is some support that wheelchair training programs influence wheelchair maneuverability, which is also supported by the results found in the qualitative the studies. This knowledge can be the starting point for developing guidelines for practical education and training for all wheelchair users in healthcare.
Equal care and equal living conditions
According to the Health Care Act, the healthcare authorities are obliged to offer aids for people with disabilities. Regions and municipalities decide for themselves which, and how many, assistive products are to be offered as one part of the public commitment. There are regional differences in terms of supply of wheelchairs, how the need for a wheelchair is assessed, how the choice of a specific wheelchair is done, as well as whether practical education and training is offered. In addition, some regions charge the individual a fee which may affect access. Restrictions to access can reduce the possibility of attaining good health and care on equal terms for the entire population and can influence the opportunities for individuals to be active and involved in society, achieve freedom of action, quality of life and good health.
When resources are limited, decisions must be made about how different needs are to be met and prioritized. When making public decisions, it is therefore important to have a structured approach to opportunity costs; systems and routines to help decision-makers deliberately weigh costs against benefits.
Option to choose
Ethical dilemmas can arise when the individual's perceived needs differ from the prescriber's assessment in relation to the regulations. A prescription should always be need-based according to current legislation and prescription process, but it is the health authority, not the individual, who assesses that the need meets the criteria for prescription of assistive devices. The person must also be given the opportunity to choose between different aids, but in practice there may be no alternatives to choose between. An actual lack of choice reduces the individual’s ability to have freedom of action, as well as the ability of society to realize the disability policy goals of full participation in society and equal living conditions for everyone.
Scientific knowledge gaps
Most of the questions that SBU evaluated in this report could not be answered because there is a lack of scientific studies. Because so many research questions are unanswered, it is necessary to prioritize among these, preferably in consultation with those affected by the results (e.g., using the James Lind Alliance method). In the process, a selection of prioritized outcomes (Core Outcome Set) can be defined. The fact that there is a lack of research on children and young people should particularly be addressed. It is also important that future research includes both women and men.
The full report in Swedish

Project group
Experts
- Katarina Baudin, Reg. Occupational therapist, PhD, Karolinska Institutet
- Emelie Butler Forslund, Reg. Physiotherapist, PhD, Karolinska Institutet/Spinalis, Aleris Rehab Station
- Åsa Larsson Ranada, Reg. Occupational therapist, PhD, Associate Professor, Linköping University
- Eva Månsson Lexell, Reg. Occupational therapist, PhD, senior lecturer, Associate professor, Lund University/Skåne University Hospital
- Cecilia Pettersson, Reg. Occupational therapist, PhD, Associate Professor, Örebro University
- Kerstin Wahman, Reg. Physiotherapist, PhD, Associate Professor, Karolinska Institutet /Aleris Rehab Station
SBU
- Susanna Larsson Tholén, Project Manager
- Marit Grönberg Eskel, Ass. Project Manager
- Maria Ahlberg, Project Administrator
- Magnus Börjesson, Digital strategist
- Thérèse Eriksson, Health Economist
- Klas Moberg, Information Specialist (to Jan 2021)
- Carl Gornitzki, Information Specialist (from January 2021
- Hanna Olofsson; Information Specialist (from January 2021)
- Johanna Wiss, Health Economist
Flow Chart
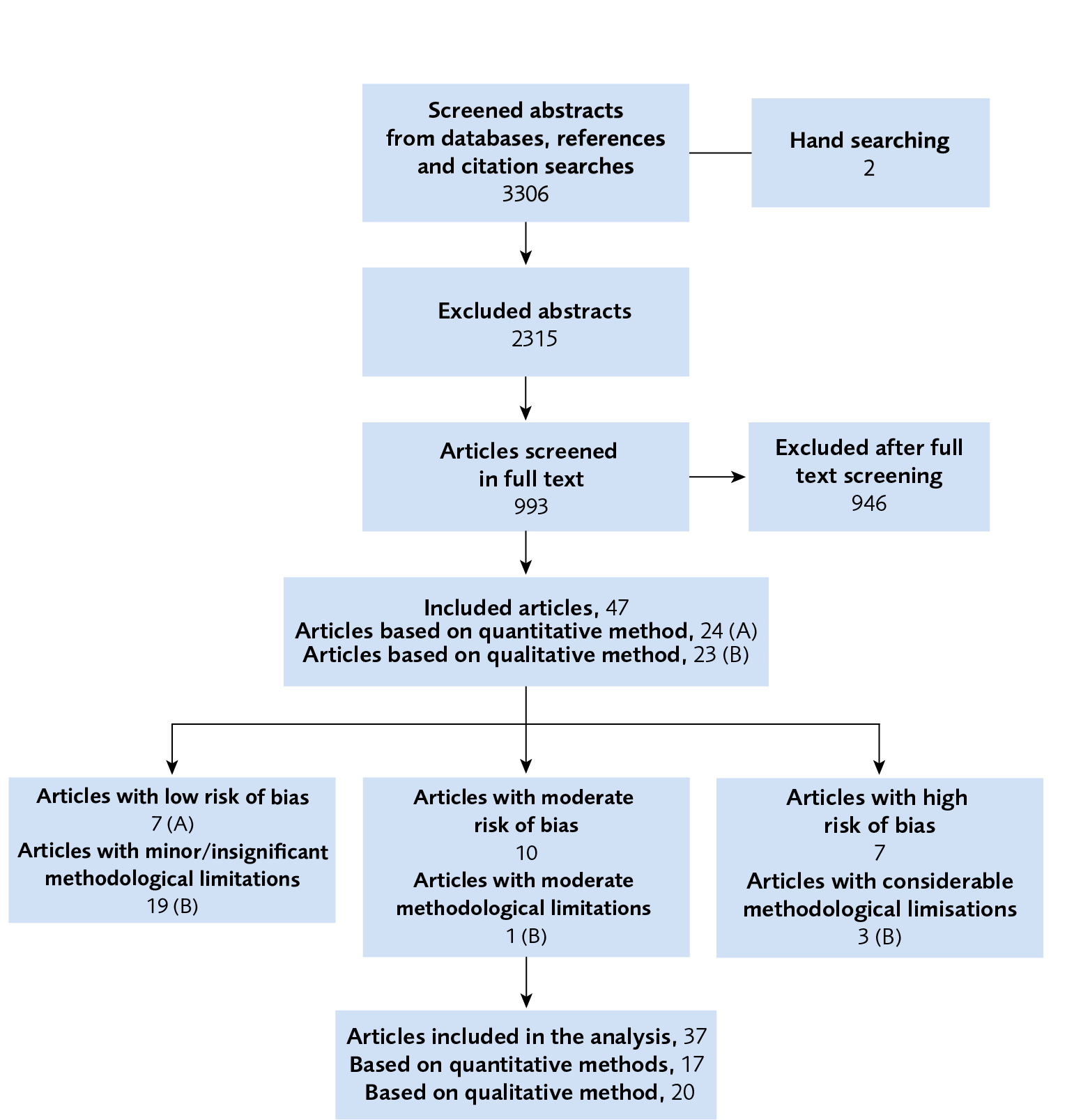
Figure 1 Flow chart over primary studies.
References
- SBU. Utvärdering av metoder i hälso- och sjukvården och insatser i socialtjänsten: en metodbok. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2020. [accessed Sep 20 2021]. Available from: https://www.sbu.se/metodbok.
- Giesbrecht EM, Ripat JD, Cooper JE, Quanbury AO. Experiences with using a pushrim-activated power-assisted wheelchair for community-based occupations: a qualitative exploration. Canadian Journal of Occupational Therapy - Revue Canadienne d Ergotherapie. 2011;78(2):127-36. Available from: https://doi.org/10.2182/cjot.2011.78.2.8
- Pettersson C, Iwarsson S, Brandt A, Norin L, Mansson Lexell E. Men's and women's perspectives on using a powered mobility device: benefits and societal challenges. Scand J Occup Ther. 2014;21(6):438-46. Available from: https://doi.org/https://dx.doi.org/10.3109/11038128.2014.905634.
- Rushton PW, Mortenson BW, Viswanathan P, Wang RH, Miller WC, Hurd Clarke L. Intelligent power wheelchair use in long-term care: potential users’ experiences and perceptions. Disability & Rehabilitation: Assistive Technology. 2017;12(7):740-6. Available from: https://doi.org/10.1080/17483107.2016.1260653.
- Mandy A, Stew G, Michaelis J, Scott W, White E. User evaluation of the Neater Uniwheelchair in the home environment: an exploratory pilot study...including commentary by Scott W and White E. International Journal of Therapy & Rehabilitation. 2011;18(4):231-7. Available from: https://doi.org/10.12968/ijtr.2011.18.4.231.
- Krantz O, Egard H. Use of active wheelchairs in everyday life: experiences among experienced users of active ultra lightweight rigid frame wheelchairs. Disability & Rehabilitation Assistive Technology. 2017;12(1):65-72. Available from: https://doi.org/10.3109/17483107.2015.1065514
- Mattie J, Aitken-Mundhenk L, Bicknell L, Mortenson WB, Borisoff J. Exploring the lived experience of people using ultralight wheelchairs with on-the-fly adjustable seating function. Disability & Rehabilitation Assistive Technology. 2020;15(8):878-84. Available from: https://doi.org/https://dx.doi.org/10.1080/17483107.2019.1626920.
- Titus LC, Miller Polgar J. Reasons for using power tilt: perspectives from clients and therapists. Disability & Rehabilitation: Assistive Technology. 2018;13(2):132-9. Available from: https://doi.org/10.1080/17483107.2017.1299803.
- Arthanat S, Desmarais JM, Eikelberg P. Consumer perspectives on the usability and value of the iBOT( R) wheelchair: findings from a case series. Disability & Rehabilitation Assistive Technology. 2012;7(2):153-67. Available from: https://doi.org/https://dx.doi.org/10.3109/17483107.2011.589487.
- Fomiatti R, Moir L, Richmond J, Millsteed J. The experience of being a motorised mobility scooter user. Disability & Rehabilitation Assistive Technology. 2014;9(3):183-7. Available from: https://doi.org/https://dx.doi.org/10.3109/17483107.2013.814171.
- Gudgeon S, Kirk S. Living with a powered wheelchair: exploring children's and young people's experiences. Disability & Rehabilitation Assistive Technology. 2015;10(2):118-25. Available from: https://doi.org/https://dx.doi.org/10.3109/17483107.2013.870609.
- Mattie J, Tavares J, Matheson B, Smith E, Denison I, Miller WC, et al. Evaluation of the Nino R Two-Wheeled Power Mobility Device: A Pilot Study. IEEE Trans Neural Syst Rehabil Eng. 2020;28(11):2497-506. Available from: https://doi.org/https://dx.doi.org/10.1109/TNSRE.2020.3028327.
- Titus LC, Miller-Polgar J. To tilt or not to tilt; the decision-making process. Disability & Rehabilitation Assistive Technology. 2019:1-9. Available from: https://doi.org/https://dx.doi.org/10.1080/17483107.2019.1632943.
- Rice LA, Yarnot R, Mills S, Sonsoff J. A pilot investigation of anterior tilt use among power wheelchair users. Disability & Rehabilitation: Assistive Technology. 2021;16(2):152-9. Available from: https://doi.org/10.1080/17483107.2019.1644676.
- Rice LA, Sung J, Peters J, Bartlo WD, Sosnoff JJ. Perceptions of fall circumstances, injuries and recovery techniques among power wheelchair users: a qualitative study. Clin Rehabil. 2018;32(7):985-93. Available from: https://doi.org/10.1177/0269215518768385.
- Borisoff JF, Ripat J, Chan F. Seasonal Patterns of Community Participation and Mobility of Wheelchair Users Over an Entire Year. Arch Phys Med Rehabil. 2018;99(8):1553-60. Available from: https://doi.org/10.1016/j.apmr.2018.02.011.
- Blach Rossen C, Sorensen B, Wurtz Jochumsen B, Wind G. Everyday life for users of electric wheelchairs - a qualitative interview study. Disability & Rehabilitation Assistive Technology. 2012;7(5):399-407. Available from: https://doi.org/https://dx.doi.org/10.3109/17483107.2012.665976.
- Frank AO, De Souza LH, Frank JL, Neophytou C. The pain experiences of powered wheelchair users. Disabil Rehabil. 2012;34(9):770-8. Available from: https://doi.org/https://dx.doi.org/10.3109/09638288.2011.619620.
- Hughes M, Burton AE, Dempsey RC. 'I am free in my wheelchair but pain does have a say in it though': The meaning and experience of quality of life when living with paraplegia and chronic pain. J Health Psychol. 2019;24(10):1356-67. Available from: https://doi.org/https://dx.doi.org/10.1177/1359105317750254.
- Bowers D, Morgan K, Abbott LR, Fishleigh L, Cousins AL, Taylor R. User perceptions of powered wheelchair features. Technology, Mind, and Behavior. 2020;1(2). Available from: https://doi.org/10.1037/tmb0000011.
- Barbareschi G, Holloway C. Understanding independent wheelchair transfers. Perspectives from stakeholders. Disability & Rehabilitation: Assistive Technology. 2020;15(5):545-52. Available from: https://doi.org/10.1080/17483107.2019.1594407.
- Giesbrecht EM, Ripat JD, Quanbury AO, Cooper JE. Participation in community-based activities of daily living: comparison of a pushrim-activated, power-assisted wheelchair and a power wheelchair. Disability & Rehabilitation Assistive Technology. 2009;4(3):198-207. Available from: https://doi.org/https://dx.doi.org/10.1080/17483100802543205.
- Chen W-L, Chen S-C, Chen Y-L, Chen S-H, Hsieh J-C, Lai J-S, et al. The M3S-based electric wheelchair for the people with disabilities in Taiwan. Disability and Rehabilitation: An International, Multidisciplinary Journal. 2005;27(24):1471-7. Available from: https://doi.org/10.1080/09638280500264725.
- Brienza DM, Karg PE, Bertolet M, Schmeler M, Poojary-Mazzotta P, Vlachos H, et al. A Randomized Clinical Trial of Wheeled Mobility for Pressure Injury Prevention and Better Function. J Am Geriatr Soc. 2018;66(9):1752-9. Available from: https://doi.org/https://dx.doi.org/10.1111/jgs.15495.
- Rice IM, Pohlig RT, Gallagher JD, Boninger ML. Handrim wheelchair propulsion training effect on overground propulsion using biomechanical real-time visual feedback. Arch Phys Med Rehabil. 2013;94(2):256-63. Available from: https://doi.org/https://dx.doi.org/10.1016/j.apmr.2012.09.014.
- Rice LA, Smith I, Kelleher AR, Greenwald K, Boninger ML. Impact of a wheelchair education protocol based on practice guidelines for preservation of upper-limb function: a randomized trial. Arch Phys Med Rehabil. 2014;95(1):10-9.e1. Available from: https://doi.org/https://dx.doi.org/10.1016/j.apmr.2013.06.028.
- Wang YT, Limroongreungrat W, Chang LS, Ke X, Tsai LC, Chen YP, et al. Immediate video feedback on ramp, wheelie, and curb wheelchair skill training for persons with spinal cord injury. J Rehabil Res Dev. 2015;52(4):421-30. Available from: https://doi.org/https://dx.doi.org/10.1682/JRRD.2014.11.0286.
- Best KL, Kirby RL, Smith C, MacLeod DA. Wheelchair skills training for community-based manual wheelchair users: a randomized controlled trial. Arch Phys Med Rehabil. 2005;86(12):2316-23. Available from: https://doi.org/10.1016/j.apmr.2005.07.300
- Giesbrecht EM, Miller WC. Effect of an mHealth Wheelchair Skills Training Program for Older Adults: A Feasibility Randomized Controlled Trial. Arch Phys Med Rehabil. 2019;100(11):2159-66. Available from: https://doi.org/https://dx.doi.org/10.1016/j.apmr.2019.06.010.
- Kirby RL, Mitchell D, Sabharwal S, McCranie M, Nelson AL. Manual Wheelchair Skills Training for Community-Dwelling Veterans with Spinal Cord Injury: A Randomized Controlled Trial. PLoS ONE [Electronic Resource]. 2016;11(12):e0168330. Available from: https://doi.org/https://dx.doi.org/10.1371/journal.pone.0168330.
- MacPhee AH, Kirby RL, Coolen AL, Smith C, MacLeod DA, Dupuis DJ. Wheelchair skills training program: A randomized clinical trial of wheelchair users undergoing initial rehabilitation. Arch Phys Med Rehabil. 2004;85(1):41-50.
- Miller WC, Best KL, Eng JJ, Routhier F. Influence of Peer-led Wheelchair Training on Wheelchair Skills and Participation in Older Adults: Clinical Outcomes of a Randomized Controlled Feasibility Trial. Arch Phys Med Rehabil. 2019;100(6):1023-31. Available from: https://doi.org/https://dx.doi.org/10.1016/j.apmr.2018.10.018.
- Mountain AD, Kirby RL, Smith C, Eskes G, Thompson K. Powered wheelchair skills training for persons with stroke: a randomized controlled trial. Am J Phys Med Rehabil. 2014;93(12):1031-43. Available from: https://doi.org/https://dx.doi.org/10.1097/PHM.0000000000000229.
- Routhier F, Kirby RL, Demers L, Depa M, Thompson K. Efficacy and retention of the French-Canadian version of the wheelchair skills training program for manual wheelchair users: a randomized controlled trial. Arch Phys Med Rehabil. 2012;93(6):940-8. Available from: https://doi.org/https://dx.doi.org/10.1016/j.apmr.2012.01.017.
- Yeo SS, Kwon JW. Wheelchair Skills Training for Functional Activity in Adults with Cervical Spinal Cord Injury. Int J Sports Med. 2018;39(12):924-8. Available from: https://doi.org/https://dx.doi.org/10.1055/a-0635-0941.
- Best KL, Miller WC, Huston G, Routhier F, Eng JJ. Pilot Study of a Peer-Led Wheelchair Training Program to Improve Self-Efficacy Using a Manual Wheelchair: A Randomized Controlled Trial. Arch Phys Med Rehabil. 2016;97(1):37-44. Available from: https://doi.org/https://dx.doi.org/10.1016/j.apmr.2015.08.425.
- Kirby RL, Miller WC, Routhier F, Demers L, Mihailidis A, Polgar JM, et al. Effectiveness of a Wheelchair Skills Training Program for Powered Wheelchair Users: A Randomized Controlled Trial. Arch Phys Med Rehabil. 2015;96(11):2017-26.e3. Available from: https://doi.org/https://dx.doi.org/10.1016/j.apmr.2015.07.009.
- Worobey LA, Kirby RL, Heinemann AW, Krobot EA, Dyson-Hudson TA, Cowan RE, et al. Effectiveness of Group Wheelchair Skills Training for People With Spinal Cord Injury: A Randomized Controlled Trial. Arch Phys Med Rehabil. 2016;97(10):1777-84.e3. Available from: https://doi.org/https://dx.doi.org/10.1016/j.apmr.2016.04.006.
- Uppföljning av funktionshinderspolitiken 2020 del II - Statistik om förutsättningar och levnadsvillkor för personer med funktionsnedsättning. Sundbyberg: Myndigehten för delaktighet; 2020. [accessed Feb 28 2022]. Available from: https://www.mfd.se/vart-uppdrag/publikationer/rapport/uppfoljning-av-funktionshinderspolitiken-2020-del-ii/.
- Sjöberg M. Uppdraget slutfört – Hjälpmedelsinstitutets historia: Hjälpmedelsinstitutet; 2016. [accessed Feb 18 2022]. Available from: https://www.mfd.se/contentassets/8302d2c7ab93474085b4e0e7f18d824c/uppdraget-slutfort---hjalpmedelsinstitutets-historia.
- Från mottagare till medskapare. Ett kunskapsunderlag för en mer personcentrerad hälso- och sjukvård: Myndigheten för vård- och omsorgsanalys; 2018. [accessed Feb 18 2022]. Available from: https://www.vardanalys.se/wp-content/uploads/2018/11/Rapport-2018-08-Fr%C3%A5n-mottagare-till-medskapare.pdf.
- Personcentrerad vård i Sverige. Stockholm: Sveriges Kommuner och Regioner (SKR); 2018. [accessed Feb 28 2022]. Available from: https://skr.se/skr/tjanster/rapporterochskrifter/publikationer/personcentreradvardisverige.54829.html.
- Förskrivning av hjälpmedel. Stöd vid förskrivning av hjälpmedel till personer med funktionsnedsättning. Stockholm: Socialstyrelsen; 2021. [accessed Feb 22 2022]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2021-12-7673.pdf.
- S2019/01378/FST (delvis). Regeringsbeslut. Uppdrag om statistik på hjälpmedelsområdet: Regeringen. [accessed Feb 22 2022]. Available from: https://www.regeringen.se/495df5/contentassets/b40e7171c4434fe29505cb5fb4126b67/uppdrag-om-statistik-pa-hjalpmedelsomradet.pdf.
- Uppdrag statistik på hjälpmedelsområdet – slutrapport. Stockholm: Socialstyrelsen; 2021. [accessed Feb 21 2022]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/statistik/2021-12-7696.pdf.
- Brundell S. Förflyttnings- och kognitionshjälpmedel. Metodbeskrivning statistik: Hjälpmedelsinstitutet; 2014. [accessed Feb 22 2022]. Available from: https://docplayer.se/10193482-Forflyttningsoch-kognitionshjalpmedel-metodbeskrivning-statistik.html.
- SOU. Hjälpmedel för förflyttning. In: På lika villkor! Delaktighet, jämlikhet och effektivitet i hjälpmedelsförsörjningen. Statens offentliga utredningar SOU 2017:43 Stockholm: Regeringen; 2017. [accessed Feb 22 2022]; p. 127. Available from: https://www.regeringen.se/49c8c5/contentassets/09ba8e1b70554a88a21c6450cc10af8e/sou-2017_43_webb_ta.pdf.
- Hälso- och sjukvårdslag (2017:30). 8 kap. Ansvar att erbjuda hälso- och sjukvård 7 §. 12 kap. Ansvar att erbjuda hälso- och sjukvård 5 §. Stockholm: Sveriges riksdag. [accessed Feb 24 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/halso--och-sjukvardslag_sfs-2017-30.
- SOU. Hjälpmedel för förflyttning. In: På lika villkor! Delaktighet, jämlikhet och effektivitet i hjälpmedelsförsörjningen. Statens offentliga utredningar SOU 2017:43. Stockholm: Regeringen; 2017. [accessed Feb 24 2022]; p. 66. Available from: https://www.regeringen.se/49c8c5/contentassets/09ba8e1b70554a88a21c6450cc10af8e/sou-2017_43_webb_ta.pdf.
- Lag (2007:1091) om offentlig upphandling. Stockholm: Sveriges riksdag. [accessed Feb 24 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/lag-20071091-om-offentlig-upphandling_sfs-2007-1091.
- Hjälpmedel i kommuner och landsting. En nationell kartläggning av regler, avgifter, tillgång och förskrivning. Stockholm: Socialstyrelsen; 2016. [accessed Feb 22 2022]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2016-4-1.pdf.
- Lag (1993:584) om medicintekniska produkter. Stockholm: Sveriges riksdag. [accessed Feb 24 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/lag-1993584-om-medicintekniska-produkter_sfs-1993-584.
- Regelverk för medicintekniska produkter. Stockholm: Läkemedelsverket; 2019. [updated July 16 2021; accessed Feb 24 2022]. Available from: https://www.lakemedelsverket.se/sv/medicinteknik/tillverka/regelverk.
- EUR-Lex home . Document 02017R0745-20200424. Luxemburg: European Union. [accessed Feb 24 2022]. Available from: https://eur-lex.europa.eu/legal-content/SV/TXT/?uri=CELEX:02017R0745-20200424.
- Läkemedelsverkets föreskrifter (LVFS 2003:11) om medicintekniska produkter. Stockholm: Läkemedelsverket. [accessed Feb 24 2022]. Available from: https://www.lakemedelsverket.se/sv/lagar-och-regler/foreskrifter/2003-11.
- Patientlag (2014:821). Stockholm: Sveriges riksdag. [accessed Feb 24 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/patientlag-2014821_sfs-2014-821.
- Uppföljning av patientlagen inom hjälpmedelsområdet. Stockholm: Socialstyrelsen; 2017. [accessed Feb 24 2022]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2017-12-12.pdf.
- Socialdepartementets proposition 2013/14:67. Mer inflytande för den enskilde i valet av hjälpmedel. Stockholm: Regeringskansliet. [accessed Feb 24 2022]. Available from: https://www.regeringen.se/rattsliga-dokument/proposition/2014/01/prop.-20131467/.
- Konvention om rättigheter för personer med funktionsnedsättning SÖ 2008:26. Stockholm: Regeringskansliet. [accessed Feb 24 2022]. Available from: https://www.regeringen.se/4ae1cb/globalassets/regeringen/dokument/socialdepartementet/funktionshinder/konvention-om-rattigheter-for-personer-med-funktionsnedsattning.pdf.
- SOU. Hjälpmedel för förflyttning. In: På lika villkor! Delaktighet, jämlikhet och effektivitet i hjälpmedelsförsörjningen. Statens offentliga utredningar SOU 2017:43. Stockholm: Regeringen; 2017. [accessed Feb 24 2022]; p. 58. Available from: https://www.regeringen.se/49c8c5/contentassets/09ba8e1b70554a88a21c6450cc10af8e/sou-2017_43_webb_ta.pdf.
- FN:s konvention om rättigheter för personer med funktionsnedsättning S2019/05119/FST. Stockholm: Sveriges riksdag. [accessed Feb 24 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svar-pa-skriftlig-fraga/fns-konvention-om-rattigheter-for-personer-med_H712547.
- Lag (2018:1197) om Förenta nationernas konvention om barnets rättigheter. Stockholm: Sveriges riksdag. [accessed Feb 24 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/lag-20181197-om-forenta-nationernas-konvention_sfs-2018-1197.
- SOU. Barnkonventionen och svensk rätt. Statens offentliga utredningar 2020:63; Vol 1 p 298. Stockholm: Regeringskansliet. [accessed Feb 24 2022]. Available from: https://www.regeringen.se/4abd8f/contentassets/3c4668adf3534dbc8ac4a7a9daa6416a/barnkonventionen-och-svensk-ratt-sou-202063-volym-1.pdf.
- SOU. Barnkonventionen och svensk rätt Statens offentliga utredningar SOU 2020:63; Vol 1 p 298-299. Stockholm: Regeringskansliet. [accessed Feb 24 2022]. Available from: https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/2020/11/sou-202063/.
- SOU. Barnkonventionen och svensk rätt. Statens offentliga utredningar SOU 2020:63; Vol 1 p 300. Stockholm: Regeringskansliet. [Available from: https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/2020/11/sou-202063/.
- Norsten Å. Drivkraft - Körergonomi, rullstolsteknik & metodik ISBN 91-631-0025-8: Aleris Rehab Station Stockholm; 2003.
- Engström B. Ergonomi. Sittande & rullstolar ISBN 91-972379-2-2: Engström Concept AB; 2007.
- Handbok till bra sittande. Stockholm: Hjälpmedelsinstitutet. [accessed Feb 24 2022]. Available from: https://docplayer.se/210773-Handbok-till-bra-sittande-en-vagledning-genom-forskrivningsprocessen.html.
- Statistik om personer med funktionsnedsättning, tabeller 2018–2019. Statistikmyndigheten. [accessed Feb 24 2022]. Available from: https://www.scb.se/hitta-statistik/statistik-efter-amne/levnadsforhallanden/levnadsforhallanden/undersokningarna-av-levnadsforhallanden-ulf-silc/pong/tabell-och-diagram/statistik-om-personer-med-funktionsnedsattning/tabeller-20182019/.
- Tinghög G. SNS Analys 77. Alternativkostnadens psykologi – känslor och kostnadseffektivitet vid beslut i offentlig sektor. Stockholm: SNS analys; 2021. [accessed Feb 24 2022]. Available from: https://www.sns.se/artiklar/sns-analys-77-alternativkostnadens-psykologi-kanslor-och-kostnadseffektivitet-vid-beslut-i-offentlig-sektor/.
- Persson J, Arlinger S, Husberg M. Kostnader och effekter vid förskrivning av hörapparat. CMT Rapport 2008:5: LiU-Tryck, Linköpings universitet; 2008. [accessed Feb 24 2022]. Available from: http://liu.diva-portal.org/smash/get/diva2:265372/FULLTEXT01.pdf.
- Persson J, Husberg M, Hellbom G, Fries A. Kostnader och effekter vid förskrivning av rollatorer. CMT Rapport 2007:3: LiU-Tryck, Linköpings universitet; 2007. [accessed Feb 24 2022]. Available from: http://www.diva-portal.org/smash/get/diva2:261598/FULLTEXT01.pdf.
- Svensson M, Nilsson FO, Arnberg K. Reimbursement Decisions for Pharmaceuticals in Sweden: The Impact of Disease Severity and Cost Effectiveness. Pharmacoeconomics. 2015;33(11):1229-36. Available from: https://doi.org/10.1007/s40273-015-0307-6.
- Brodin H, Persson J. Cost-utility analysis of assistive technologies in the European Commission's TIDE Program. Technology Initiative for Disabled and Elderly People. Int J Technol Assess Health Care. 1995;11(2):276-83. Available from: https://doi.org/10.1017/s0266462300006899.
- SOU. 1995: Vårdens svåra val. Statens offentliga utredningar SOU 1995:5. Stockholm: Socialdepartementet. [updated April 2 2015; accessed Feb 24 2022]. Available from: https://www.regeringen.se/rattsliga-dokument/statens-offentliga-utredningar/1995/03/sou-19955/.
- Regeringens proposition 1996/1996/97:60. Prioriteringar inom hälso- och sjukvården. Stockholm: Regeringen. [accessed Feb 21 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/proposition/prioriteringar-inom-halso--och-sjukvarden_GK0360.
- PRISMA. [accessed Feb 24 2022]. Available from: http://www.prisma-statement.org/.
- Hjälpmedel för personer med funktionsnedsättning - Klassificering och terminologi. Assistive products for persons with disability - Classification and terminology (ISO 9999:2016). Stockholm: Svenska institutet för standarder. [accessed Feb 28 2022]. Available from: https://www.sis.se/produkter/halso-och-sjukvard/hjalpmedel-for-personer-med-funktionsnedsattning/hjalpmedel-for-personer-med-funktionsnedsattningar/ss-en-iso-99992016/.
- Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016;104(3):240-3. Available from: https://doi.org/10.3163/1536-5050.104.3.014.
- Cochrane RevMan. London: The Cochrane Collaboration. [accessed Feb 17 2022]. Available from: https://training.cochrane.org/online-learning/core-software-cochrane-reviews/revman.
- The Cochrane Collaboration. 9.4.5.2 Meta-analysis of change scores. In: Cochrane Handbook for Systematic Reviews of Interventions. London: The Cochrane Collaboration; 2011. [accessed Feb 21 2022]. Available from: https://handbook-5-1.cochrane.org/chapter_9/9_4_5_2_meta_analysis_of_change_scores.htm.
- Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol. 2008;8:45. Available from: https://doi.org/10.1186/1471-2288-8-45.
- GRADE-CERQual. The GRADE-CERQual Project Group. [accessed Sep 20 2021]. Available from: https://www.cerqual.org/.
- Socialtjänstlag (2001:453). Stockholm: Sveriges riksdag. [accessed Feb 24 2022]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/socialtjanstlag-2001453_sfs-2001-453.
- Lag (1993:387) om stöd och service till vissa funktionshindrade. Stockholm: Sveriges riksdag. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/lag-1993387-om-stod-och-service-till-vissa_sfs-1993-387.
- Statistik om insatser i kommunal hälso- och sjukvård. Stockholm: Socialstyrelsen; 2020. [Available from: https://www.socialstyrelsen.se/statistik-och-data/statistik/statistikamnen/insatser-i-kommunal-halso-och-sjukvard/.
- SBU. Etiska aspekter på insatser inom hälso- och sjukvården. En vägledning för att identifiera relevanta etiska aspekter. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2021. [accessed Dec 16 2021]. Available from: https://www.sbu.se/globalassets/ebm/etiska_aspekter_halso_sjukvarden.pdf.
- SBU. Etiska aspekter på insatser inom det sociala området. En vägledning för att identifiera relevanta etiska frågor. Stockholm: Statens beredning för medicinsk och social utvärdering (SBU); 2019. Available from: https://www.sbu.se/globalassets/ebm/etiska_aspekter_sociala_omradet.pdf.
- Jannink MJ, Erren-Wolters CV, de Kort AC, van der Kooij H. An electric scooter simulation program for training the driving skills of stroke patients with mobility problems: a pilot study. Cyberpsychology & Behavior. 2008;11(6):751-4. Available from: https://doi.org/https://dx.doi.org/10.1089/cpb.2007.0271.
- Mahajan HP, Spaeth DM, Dicianno BE, Brown K, Cooper RA. Preliminary evaluation of variable compliance joystick for people with multiple sclerosis. J Rehabil Res Dev. 2014;51(6):951-62. Available from: https://doi.org/https://dx.doi.org/10.1682/JRRD.2013.01.0023.
- Ozturk A, Ucsular FD. Effectiveness of a wheelchair skills training programme for community-living users of manual wheelchairs in Turkey: a randomized controlled trial. Clin Rehabil. 2011;25(5):416-24. Available from: https://doi.org/https://dx.doi.org/10.1177/0269215510386979.
- Rice IM, Rice LA, Motl RW. Promoting Physical Activity Through a Manual Wheelchair Propulsion Intervention in Persons With Multiple Sclerosis. Arch Phys Med Rehabil. 2015;96(10):1850-8. Available from: https://doi.org/https://dx.doi.org/10.1016/j.apmr.2015.06.011.
- Park JM, Jung HS. A study on the effects of modified wheelchair skills program (WSP) for hemiplegic clients. Assist Technol. 2019:1-8. Available from: https://doi.org/https://dx.doi.org/10.1080/10400435.2019.1678534.
- Mandy A, Walton C, Michaelis J. Comparison of activities of daily living (ADLs) in two different one arm drive wheelchairs: A study of individuals/participants with hemiplegia. Disability and Rehabilitation: Assistive Technology. 2015;10(2):108-12. Available from: https://doi.org/10.3109/17483107.2013.845612.
- Presperin Pedersen J, Smith C, Dahlin M, Henry M, Jones J, McKenzie K, et al. Wheelchair backs that support the spinal curves: Assessing postural and functional changes. J Spinal Cord Med. 2020:1-10. Available from: https://doi.org/https://dx.doi.org/10.1080/10790268.2020.1760530.
- Shankar S, Mortenson WB, Wallace J. Taking Control: An Exploratory Study of the Use of Tilt-in-Space Wheelchairs in Residential Ca. Am J Occup Ther. 2015;69(2):1-8. Available from: https://doi.org/10.5014/ajot.2014.013565.
- Giacobbi PR, Jr., Levy CE, Dietrich FD, Winkler SH, Tillman MD, Chow JW. Wheelchair users' perceptions of and experiences with power assist wheels. Am J Phys Med Rehabil. 2010;89(3):225-34. Available from: https://doi.org/https://dx.doi.org/10.1097/PHM.0b013e3181c9d7df.
- Özcan E, Topcu ZG, Arasli H. Determinants of travel participation and experiences of wheelchair users traveling to the bodrum region: A qualitative study. Int J Environ Res Public Health. 2021;18(5):1-28. Available from: https://doi.org/10.3390/ijerph18052218.
- Paralyzed Veterans of America Consortium for Spinal Cord Medicine. Preservation of upper limb function following spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med. 2005;28(5):434-70. Available from: https://doi.org/10.1080/10790268.2005.11753844.
- Wheelchair skills program. Halifax Canada: Dalhousie University and Capital Health. [accessed Feb 27 2022]. Available from: https://wheelchairskillsprogram.ca/en/.
- Best KL, Miller WC, Eng JJ, Routhier F, Goldsmith C. Randomized controlled trial protocol feasibility: The Wheelchair Self-Efficacy Enhanced for Use (WheelSeeU). Canadian Journal of Occupational Therapy - Revue Canadienne d Ergotherapie. 2014;81(5):308-19. Available from: https://doi.org/10.1177/0008417414546743
- Scobbie L, Wyke S, Dixon D. Identifying and applying psychological theory to setting and achieving rehabilitation goals. Clin Rehabil. 2009;23(4):321-33. Available from: https://doi.org/10.1177/0269215509102981.
- Giesbrecht EM, Miller WC, Eng JJ, Mitchell IM, Woodgate RL, Goldsmith CH. Feasibility of the Enhancing Participation In the Community by improving Wheelchair Skills (EPIC Wheels) program: study protocol for a randomized controlled trial. Trials [Electronic Resource]. 2013;14:350. Available from: https://doi.org/https://dx.doi.org/10.1186/1745-6215-14-350.
- Andrich R, Salatino C, Converti RM, Saruggia M. Cost-effectiveness of powered wheelchairs: findings of a study. Stud Health Technol Inform. 2015;217:84-91. Available from: https://doi.org/10.3233/978-1-61499-566-1-84
- Salatino C, Andrich R, Converti RM, Saruggia M. An observational study of powered wheelchair provision in Italy. Assist Technol. 2016;28(1):41-52. Available from: https://doi.org/https://dx.doi.org/10.1080/10400435.2015.1074631.
- Samuelsson K, Wressle E. Powered wheelchairs and scooters for outdoor mobility: a pilot study on costs and benefits. Disability & Rehabilitation Assistive Technology. 2014;9(4):330-4. Available from: https://doi.org/https://dx.doi.org/10.3109/17483107.2013.827244.
- Levy CE, Buman MP, Chow JW, Tillman MD, Fournier KA, Giacobbi P, Jr. Use of power assist wheels results in increased distance traveled compared with conventional manual wheeling. Am J Phys Med Rehabil. 2010;89(8):625-34. Available from: https://doi.org/https://dx.doi.org/10.1097/PHM.0b013e3181e72286.
- Vägar till ökad delaktighet. Kunskapsstöd för socialtjänsten om arbete med stöd och service enligt LS. tockholm: Socialstyrelsen; 2017. [accessed Feb 28 2022]. Available from: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/kunskapsstod/2017-12-21.pdf.
- Slutrapportering av regeringsuppdrag inom ramen för ”En strategi för genomförande av funktionshinderspolitiken 2011–2016. Stockholm: Folkhälsomyndigheten; 2016. [accessed Feb 28 2022]. Available from: https://www.folkhalsomyndigheten.se/contentassets/a9f9f81fd47c40ecb2241b5d2658bfe2/slutrapport-funktionshindersuppdraget-2011-2016.pdf.
- Larsson Ranada A, Lidstrom H. Satisfaction with assistive technology device in relation to the service delivery process-A systematic review. Assist Technol. 2019;31(2):82-97. Available from: https://doi.org/10.1080/10400435.2017.1367737.
- Skuldran och skuldersmärta. Solna: Stiftelsen Spinalis. [accessed Feb 22 2022]. Available from: https://xn--ryggmrgsskada-ffb.se/axlar-skuldror/.
- Claesson IM, Stahle A, Johansson S. Being limited by Parkinson's disease and struggling to keep up exercising; is the group the glue? Disabil Rehabil. 2020;42(9):1270-4. Available from: https://doi.org/10.1080/09638288.2018.1522552.
- Lund K, Argentzell E, Leufstadius C, Tjornstrand C, Eklund M. Joining, belonging, and re-valuing: A process of meaning-making through group participation in a mental health lifestyle intervention. Scand J Occup Ther. 2019;26(1):55-68. Available from: https://doi.org/10.1080/11038128.2017.1409266.
- Gillisdotter A, Regardt M, Mansson Lexell E. The "Managing Fatigue" programme - experiences shared by MS participants. Scand J Occup Ther. 2021:1-10. Available from: https://doi.org/10.1080/11038128.2021.1905057.
- Bandura A. Self-efficacy: The exercise of control. New York: W H Freeman/Times Books/ Henry Holt & Co; 1997.
- Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Ann Behav Med. 2003;26(1):1-7. Available from: https://doi.org/10.1207/S15324796ABM2601_01.
- Sakakibara BM, Miller WC, Routhier F, Backman CL, Eng JJ. Association between self-efficacy and participation in community-dwelling manual wheelchair users aged 50 years or older. Phys Ther. 2014;94(5):664-74. Available from: https://doi.org/10.2522/ptj.20130308.
- Skymne C, Dahlin-Ivanoff S, Claesson L, Eklund K. Getting used to assistive devices: ambivalent experiences by frail elderly persons. Scand J Occup Ther. 2012;19(2):194-203. Available from: https://doi.org/10.3109/11038128.2011.569757.
- Edwards K, McCluskey A. A survey of adult power wheelchair and scooter users. Disabil Rehabil Assist Technol. 2010;5(6):411-9. Available from: https://doi.org/10.3109/17483101003793412.
- Fristedt S. Occupational participation through community mobility among older men and women 2012. Dissertation Series School of Health Sciences, ISSN 1654-3602 ; 33 Jönköping: School of Health Sciences. [accessed Feb 24 2022]. Available from: http://umu.diva-portal.org/smash/record.jsf?pid=diva2%3A555397&dswid=1063.
- Lund C. Kostnader och effekter vid hjälpmedelsförskrivning. Sundbyberg: Handikapp förbunden; 2010. [accessed Feb 21 2022]. Available from: http://funktionsratt.se/wp-content/uploads/2017/11/Hj%C3%A4lpmedelsrapport-3.pdf.
- Samlad prislista för färdtjänstresor. Göteborgs Stad. [accessed Feb 21 2022]. Available from: https://goteborg.se/wps/portal/start/fardtjanst/priser/samlad-prislista.
- Avgifter och kostnader för hjälp i hemmet. Göteborgs Stad. [accessed Feb 21 2022]. Available from: https://goteborg.se/wps/portal/start/aldre/hjalp-i-hemmet/avgifter-och-kostnader.
- Avgift för hemtjänst. Umeå Kommun. [accessed Feb 21 2022]. Available from: https://www.umea.se/omsorgochhjalp/hjalpihemmet/hemtjansthemhjalp/avgiftforhemtjanst.4.7d7d901172bb372c5d4ab3.html.
- Avgift för resa i färdtjänstfordon. Umeå Kommun. [accessed Feb 21 2022]. Available from: https://www.umea.se/omsorgochhjalp/resortransporterochbesok/fardtjanst/prislista.4.1c16b00a1742340e02e2769.html.
- Vad är en ryggmärgsskada? Solna: Stiftelsen Spinalis. [accessed Feb 22 2022]. Available from: https://xn--ryggmrgsskada-ffb.se/vad-ar-en-ryggmargsskada/.
- Lanutti JNL, Medola FO, Gonçalves DD, da Silva LM, Nicholl ARJ, Paschoarelli LC. The Significance of Manual Wheelchairs: A Comparative Study on Male and Female Users. Procedia Manufacturing. 2015;3:6079-85. Available from: https://doi.org/10.1016/j.promfg.2015.07.752.
- Koll på hemtjänsten? En handledning för analys av kommunens hemtjänstkostnader. Stockholm: Sveriges Kommuner och Landsting (SKL) och Rådet för främjande av kommunala analyser (rka); 2015. [accessed Feb 27 2022]. Available from: https://rka.nu/download/18.16f404af1773f47655a20264/1612887010052/RKA-koll-pa-hemtjansten-2015.pdf.
- Hagberg L, Hermansson L, Fredriksson C, Pettersson I. Cost-effectiveness of powered mobility devices for elderly people with disability. Disabil Rehabil Assist Technol. 2017;12(2):115-20. Available from: https://doi.org/10.3109/17483107.2014.1002540.
- Koll på funktionshinderområdet. Rådet för främjande av kommunala analyser (RKA) och Sveriges Kommuner och Regioner (SKR). Stockholm. [accessed Feb 27 2022]. Available from: https://rka.nu/radetforframjandeavkommunalaanalyser/analys/stodochomsorg/kollpafunktionshinderomradet.44777.html.
- Folkmängd, topp 50. Stockholm: Statistikmydigheten (SCB); 2021. [accessed Feb 27 2022]. Available from: https://www.scb.se/hitta-statistik/statistik-efter-amne/befolkning/befolkningens-sammansattning/befolkningsstatistik/pong/tabell-och-diagram/topplistor-kommuner/folkmangd-topp-50/.
- Internationell klassifikation av funktionstillstånd, funktionshinder och hälsa (ICF) Svensk version 2022. Stockholm: Socialstyrelsen. [accessed Feb 28 2022]. Available from: https://www.socialstyrelsen.se/statistik-och-data/klassifikationer-och-koder/icf/.
- Effekt utvärdering. Att välja upplägg 2006:8: Ekonomistyrningsverket. [accessed Feb 25 2022]. Available from: https://www.esv.se/contentassets/52ef54497f7a41d6a7958887d101e044/effektutvardering.pdf.
- Socialstyrelsens termbank. Stockholm: Socialstyrelsen. [accessed Feb 28 2022]. Available from: https://termbank.socialstyrelsen.se.
 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services



