This publication was published more than 5 years ago. The state of knowledge may have changed.
Insulin pumps for diabetes
Summary and conclusions
The SBU assessment of available knowledge
Good control of the blood glucose level is vital to avoid diabetes complications. In type 1 diabetes and sometimes in type 2 diabetes, intensive insulin therapy is required, which involves multiple daily injections. The most common complication associated with this therapy is low blood glucose (hypoglycaemia), which can have serious consequences. An alternative to injections for intensive insulin therapy is continuous insulin delivery using a pump, also known as continuous subcutaneous insulin infusion (CSII).
Conclusions
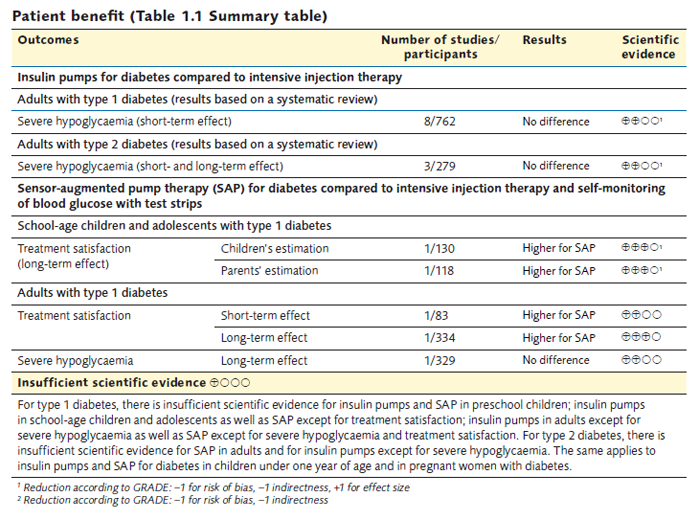
- Insulin pumps for diabetes are commonly used today, especially in the treatment of children and adolescents. However, there is a considerable lack of knowledge regarding the effects of insulin pump therapy on illness and mortality. This lack of knowledge also extends to the use of insulin pumps in combination with continuous glucose monitoring, so called sensor-augmented pump therapy (SAP). More well-performed long-term studies of all patient groups with diabetes are required.
- People with diabetes are considerably more satisfied with SAP than with intensive injection therapy and self-monitoring of blood glucose with test strips. Being satisfied with the treatment may be important in terms of achieving better blood glucose control. Available knowledge is less clear when it comes to treatment satisfaction with insulin pumps only.
- There is limited or insufficient knowledge regarding the effect of insulin pumps or SAP on quality of life, ketoacidosis and severe hypoglycaemia.
- The intervention cost of insulin pump therapy is SEK 11,000 more per patient and year compared to injection therapy. For adults, insulin pumps are used predominantly when injection therapy fails to achieve the treatment goals; it is rarely the first-choice treatment. The higher cost must be contrasted with the short- and long-term benefits from a well-functioning diabetes therapy. Individual assessment is therefore warranted pending new studies.
- For children of preschool age, insulin pumps tend to be the first-choice treatment when diabetes is diagnosed. This can be particularly important when it is difficult to inject sufficiently small doses or there is fear of needles.
- The most important measure for long-term glucose control is HbA1c, which is also closely linked to diabetes complications. Insulin pump therapy has shown some improvement in HbA1c in the short term. Studies on SAP indicate additional improvement in HbA1c. If future studies with longer follow-up periods show continued improvement, the risk of diabetes complications would be reduced.
Surrogate measures (such as HbA1c, C-peptide and glucose variability) are not evidence-graded, but are described in the report. In addition, HbA1c is reported in Appendix 3.
Study of practice
There are no comprehensive statistics on the use of insulin pumps either alone or in combination with continuous subcutaneous glucose monitoring (SAP) in Sweden. In order to chart practice of the use of these methods in specialist care more closely, a major study of practice was conducted that involved all the diabetes clinics in Sweden.
Economic aspects
Insulin pump therapy costs SEK 11 000 more per patient and year than intensive injection therapy. Since approximately 10 000 patients are treated with insulin pumps in Sweden today, it would currently amount to an additional cost of about SEK 110 million per year. If insulin pump therapy is combined with continuous glucose monitoring (SAP), the annual additional cost increases by around another SEK 28 000 per patient.
In order to calculate whether insulin pump therapy and SAP are cost-effective methods compared to injection therapy and self-monitoring of blood glucose with test strips, the increased treatment costs need to be considered in relation to the long-term effects on health.
Ethical and social aspects
Diabetes is a disease that requires considerable patient effort both day and night in a very different way from most other illnesses. Other values than the medical effects must therefore be taken into account. The methods of administrating insulin and monitoring blood glucose have considerable impact on the individual patients and their families.
Patient benefit (Table 1.1 Summary table)
How to cite this report: SBU. Insulin pumps for diabetes. Stockholm: Swedish Council on Health Technology Assessment (SBU); 2013. SBU report no 2013-03 (in Swedish).
Project group
Experts
- Unn-Britt Johansson (Professor)
- Ragnar Hanås (Associate Professor)
- Per-Olof Olsson (PhD)
- Anna Lindholm Olinder (PhD)
- Martina Persson (PhD)
SBU
- Sophie Werkö (Project Director)
- Stella Jacobson (Assistant Project Director)
- Emelie Heintz (Health Economist)
- Derya Akcan (Information Specialist)
- Anna Attergren Granath (Project Administrator)
- Thomas Davidson (Health Economist, Co-reader)
 Swedish Agency for Health Technology Assessment and Assessment of Social Services
Swedish Agency for Health Technology Assessment and Assessment of Social Services




